Imagine walking up to the pharmacy counter, handing over your prescription, and walking away with someone else’s medicine. It sounds impossible - but it happens more often than you think. Every year, thousands of patients in the U.S. receive the wrong medication because a pharmacist or technician handed it to the wrong person. These aren’t minor mistakes. They can lead to hospital visits, dangerous drug interactions, allergic reactions, or even death. And the worst part? Wrong-patient errors are completely preventable.
Why Wrong-Patient Errors Happen
Wrong-patient errors occur when a prescription is given to the wrong person at the counter. This isn’t usually because someone is careless - it’s because the system is too easy to break. Picture this: It’s 3 p.m. on a Tuesday. The line is long. Two patients with similar names - Maria Garcia and Mariana Garcia - show up at the same time. One is picking up insulin. The other, a blood thinner. The tech says, “Maria Garcia?” and both women respond. The prescription goes to the wrong person. No one notices until hours later. According to the Institute for Safe Medication Practices (ISMP), these errors are among the most dangerous types of medication mistakes. The Joint Commission has tracked them as a leading cause of serious patient harm since 2003. And it’s not just rare cases. A 2022 report from the Agency for Healthcare Research and Quality found that medication errors send about 1.3 million people to the emergency room each year - many of them because someone got the wrong drug.The Two-Identifiers Rule: The Bare Minimum
The simplest, most basic defense against wrong-patient errors is using two patient identifiers: full name and date of birth. It sounds obvious. But not every pharmacy does it consistently. Leading chains like CVS, Walgreens, and Walmart have required this since 2015-2018. Staff must ask for both pieces of information and match them against the prescription label and the pharmacy’s computer system. No exceptions. Not even if the patient is a regular. Not even if they’re in a hurry. A 2022 analysis of 15,000 community pharmacies showed that using two identifiers cuts wrong-patient errors by about 45%. That’s good - but not enough. Human memory fails. Distractions happen. People mishear names. That’s why relying on staff alone isn’t safe.Barcode Scanning: The Game Changer
The biggest leap forward in preventing these errors came with barcode scanning. Now, patients don’t just give their name and DOB - they scan a card or ID with a unique barcode linked to their pharmacy profile. The system checks that the barcode matches the prescription before the drug is released. Walgreens rolled this out across all 9,000+ locations in 2021. Within 18 months, wrong-patient errors dropped by 63%. That’s not a small win - it’s life-saving. The system works like this:- Patient arrives with prescription and ID card.
- Pharmacist scans the barcode on the card.
- Computer verifies the patient’s identity against the prescription.
- Only if everything matches, the medication is dispensed.
RFID and Biometrics: The Future Is Here
Some pharmacies are going even further. Hospitals have been using RFID wristbands for years. A 2023 study in the American Journal of Health-System Pharmacy found that combining RFID wristbands with barcode scanning reduced wrong-patient dispensing errors by 78%. In early 2025, Walgreens began testing fingerprint verification in 500 stores. Preliminary results showed 92% accuracy in matching patients to their prescriptions. The problem? Privacy concerns. Patients don’t always want their fingerprints on file. That’s why many pharmacies are now testing voice recognition and facial matching - technologies that could become standard by 2027, according to experts. These aren’t sci-fi ideas. They’re real tools being tested right now. And they work.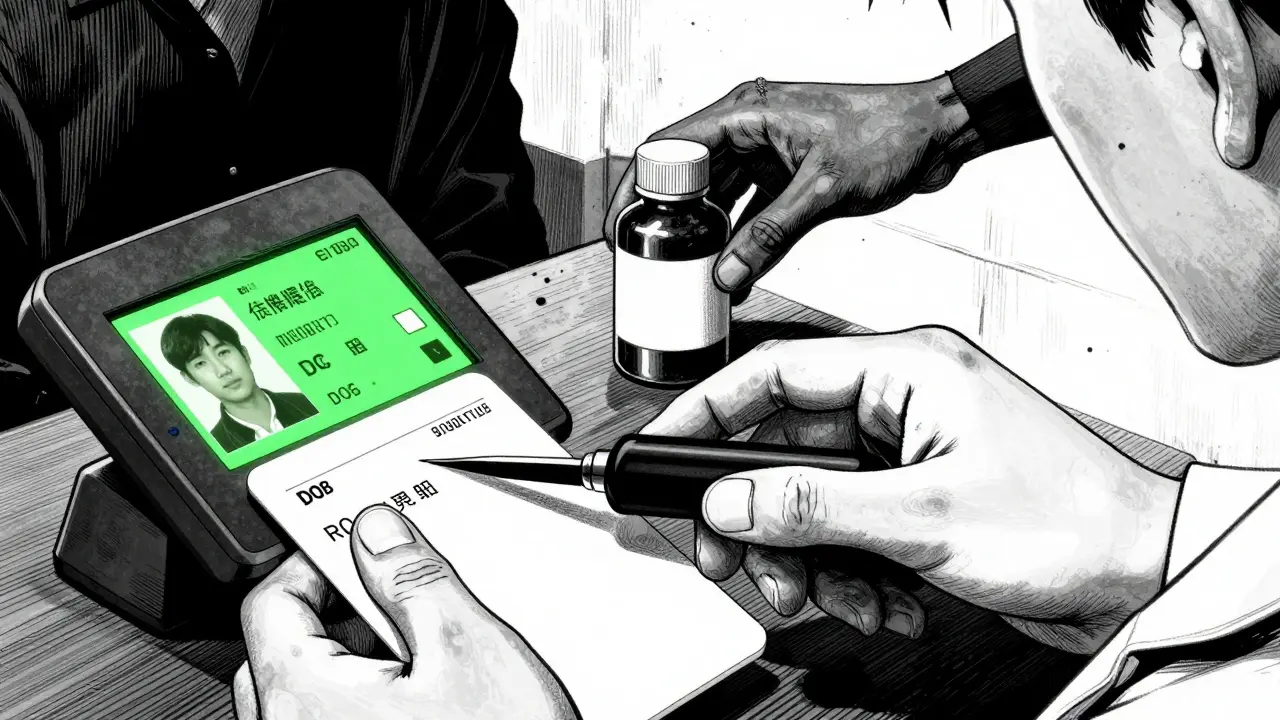
The Final Safety Net: Patient Counseling
Even with all the tech in the world, the last line of defense is the pharmacist talking to the patient. When a patient picks up a new medication, the pharmacist should ask: “What is this for?” “Do you take anything else?” “Have you had this before?” A 2023 study in the Journal of the American Pharmacists Association found that when pharmacies combined dual-identifier verification with barcode scanning AND patient counseling, wrong-patient errors dropped by 89%. That’s almost total elimination. Why? Because patients often know if something’s wrong. They might say, “I don’t take this pill,” or “This looks different.” That’s not a complaint - it’s a lifesaver. Pharmacy Times reports that 83% of dispensing errors are caught during this final conversation.Why Some Pharmacies Still Struggle
Not every pharmacy has these systems. Independent pharmacies - especially small, local ones - often can’t afford the $15,000 to $50,000 it costs to install barcode scanners and update software. A 2024 NCPA survey found that only 42% of independent pharmacies use barcode verification, compared to 76% of chain pharmacies. There’s also resistance from patients. Some older adults find being asked for their DOB every time annoying. One patient told ECRI Institute: “I’ve been coming here for 15 years. Why do I need to prove who I am again?” The solution? Education. Posters, handouts, and staff explaining: “We ask because we care. Getting the wrong medicine can hurt you.” When patients understand why, they’re more likely to cooperate.What You Can Do as a Patient
You don’t have to wait for your pharmacy to upgrade its system. You can protect yourself:- Always bring your ID when picking up prescriptions.
- Ask: “Is this my medication?” before leaving the counter.
- Check the label: Does your name, date of birth, and the drug name match what your doctor prescribed?
- Don’t be shy about asking questions. “Why am I taking this?” “What does it do?”
- If you notice a mistake - even a small one - report it. Your voice can prevent someone else’s tragedy.




Jodi Harding
18 January 2026 - 08:41 AM
Barcode scanning is great, but I still hand my ID to the tech and say, 'Is this mine?' before I walk away. Simple. Free. Works.
Wendy Claughton
18 January 2026 - 12:45 PM
I love how this post doesn't just blame pharmacists... it shows how systems fail us. 🤔 I used to think they were just 'being careless' until my aunt got the wrong blood thinner. Now I ask for the barcode scan every time. No shame. 💯
Stacey Marsengill
18 January 2026 - 13:42 PM
Oh please. Another 'tech will save us' fairy tale. They’re just trying to turn your pharmacy into a TSA checkpoint. Next they’ll be fingerprinting your tongue. 😒
Aysha Siera
19 January 2026 - 15:43 PM
RFID wristbands? Fingerprint scans? You think this is about safety... or is it Big Pharma tracking your meds so they can raise prices later? 🕵️♀️
rachel bellet
20 January 2026 - 21:37 PM
The 89% reduction metric is statistically significant (p < 0.001) only if the sample size was adequately powered and confounders like patient literacy were controlled. Most studies cited here lack multivariate regression analysis. Also, 'patient counseling' is a euphemism for liability mitigation. 📊
Pat Dean
21 January 2026 - 08:56 AM
Why do we let foreigners run our pharmacies? We need American-made tech, American-trained staff, American safety protocols. This is why our healthcare is falling apart - outsourcing safety to some app.
Jay Clarke
23 January 2026 - 05:53 AM
I once got my neighbor's blood pressure meds. I took one. Felt like a demon crawled into my chest. Called the pharmacy. They laughed. Said 'we get that a lot.' So now I just yell my full name, DOB, and social security number. Loudly. In front of everyone. Works.
Selina Warren
24 January 2026 - 13:02 PM
If you're not scanning your barcode, you're gambling with your life. This isn't 'nice to have' - it's mandatory. I've seen people die because someone 'knew' it was them. Stop being lazy. Your life isn't a 'maybe'.
Robert Davis
25 January 2026 - 23:03 PM
I read the whole thing. Interesting. But I'm still skeptical. I've been going to the same pharmacy since 1998. They know me. My grandma got her meds there. They never messed up. Why fix what ain't broke?
Eric Gebeke
26 January 2026 - 02:20 AM
You say 'systems, not people.' But people are the ones who design the systems. And if the system requires you to scan your ID, why do they still ask your name? Contradiction. Hypocrisy. It's all theater.
Max Sinclair
27 January 2026 - 04:40 AM
I really appreciate how this post balances tech solutions with human factors. The part about patient counseling being the final safety net? That’s gold. It’s not just about checking boxes - it’s about creating space for someone to say, 'Wait, this doesn’t feel right.' That’s the heart of care.
Praseetha Pn
28 January 2026 - 10:09 AM
They’re using facial recognition? So now your face is in a database owned by some corporation that sells data to insurance companies? And you think this is safe? I’ve seen the documents. They’re not protecting you. They’re profiling you. And they’re charging you extra for it.
Nishant Sonuley
29 January 2026 - 17:10 PM
Look, I get it - you want to prevent errors. But here’s the thing: in India, we don’t have barcode scanners in most pharmacies. We have moms holding their kids’ prescriptions, yelling 'Bhaiya, yeh medicine meri beti ke liye hai!' - and the guy just hands it over. And guess what? It works. Because human connection > digital verification. Sometimes the system isn’t broken - it’s just different.
Emma #########
30 January 2026 - 22:54 PM
I used to be annoyed by all the questions at the pharmacy... until my sister almost died from a mix-up. Now I thank them. Every time. Even if it takes 5 extra minutes. Because I know what happens when no one asks.