When you're dealing with severe pain-after surgery, from cancer, or due to a serious injury-opioids can be a lifeline. But they come with a price. For most people, the side effects aren't just inconvenient; they can make life harder than the pain itself. The three most common ones? Constipation, drowsiness, and nausea. These aren't rare or temporary quirks. They happen to nearly everyone who takes opioids long-term. And if you don't plan for them, they can derail your treatment before you even get relief.
Constipation: The One Side Effect That Never Goes Away
Almost every single person who takes opioids for more than a few days will get constipated. It's not a matter of if-it's a matter of when. Unlike drowsiness or nausea, which often fade after a week or two, constipation sticks around. Why? Opioids slow down your gut. They bind to receptors in your intestines, making muscles contract less, fluids get absorbed more, and stool moves slower. It's not about eating too little fiber or drinking too little water. It's pharmacology.
Doctors used to wait until constipation showed up before acting. That’s a mistake. By then, you’re already stuck-literally. The American Academy of Family Physicians recommends starting a laxative on day one of opioid therapy. Not when you haven’t gone in three days. Not when you’re in pain from bloating. Right away.
The best combo? A stimulant laxative like senna, which wakes up your intestines, plus an osmotic agent like polyethylene glycol (Miralax), which pulls water into your colon to soften stool. Together, they work better than either alone. For those who don’t respond, there’s methylnaltrexone (Relistor), a shot that blocks opioid effects in the gut without touching the brain. That means pain relief stays intact while your bowels get back to work.
Don’t rely on prune juice or fiber supplements alone. They’re not enough. If you’re on opioids, you need a real plan. Skip the shame. Talk to your provider. This isn’t a personal failure-it’s a predictable side effect with proven fixes.
Drowsiness: When Your Brain Feels Like It’s Underwater
When you first start opioids, you might feel like you’ve had five glasses of wine without drinking any. That foggy, heavy-headed feeling? That’s drowsiness. Between 20% and 60% of patients experience it when starting treatment. It’s your central nervous system being slowed down. Opioids reduce brain activity, especially in areas that keep you alert.
Good news? For most people, this fades within a week or two. Your brain adapts. But for 10% to 15% of long-term users, the drowsiness doesn’t lift. It lingers. And that’s dangerous-not just because you can’t focus at work or drive safely, but because it increases your risk of falls, accidents, and even breathing problems.
Here’s what actually helps: timing. Take your dose at night if possible. Avoid driving or operating machinery for the first few days. Cut out other sedatives-alcohol, benzodiazepines like Xanax, sleep aids. Mixing these with opioids can shut down your breathing. That’s how overdoses happen.
If drowsiness won’t go away, your doctor might consider lowering the dose. Sometimes, switching to a different opioid helps. A few studies have looked at low-dose stimulants like methylphenidate (Ritalin) to fight the fog, but the evidence is thin. And stimulants come with their own risks-increased heart rate, anxiety, insomnia. Don’t try this on your own. Talk to your provider. There’s no one-size-fits-all fix, but there are options.
Also, check your other meds. Some blood pressure pills, antihistamines, or muscle relaxants can make drowsiness worse. Your pharmacist can help you spot the culprits.
Nausea: Why Your Stomach Feels Like It’s in Revolt
Nausea hits about one in four people starting opioids. It’s not just feeling queasy-it’s the urge to vomit, sometimes with actual vomiting. This happens because opioids irritate a part of your brain called the chemoreceptor trigger zone. They also slow down your stomach, so food sits there longer, making you feel full and sick.
Like drowsiness, nausea often fades after a few days. But for 1 in 10 people, it sticks around. And when it does, it makes people stop taking their meds. That’s dangerous. If you stop opioids suddenly, you can get withdrawal: sweating, diarrhea, anxiety, and yes-more nausea. That’s why tapering off slowly matters.
There are several anti-nausea drugs, and they work differently:
- Metoclopramide and prochlorperazine block dopamine receptors. Good for nausea tied to slow digestion.
- Ondansetron blocks serotonin. Better if nausea hits fast or feels like motion sickness.
- Promethazine is an antihistamine that helps with dizziness and nausea together.
There’s no single best choice. It’s trial and error. Your doctor might start with metoclopramide because it’s cheap and works for many. If it doesn’t help, they’ll try ondansetron. Some people need to switch back and forth until they find what clicks.
Don’t wait until you’re vomiting to act. Start an antiemetic at the same time as your opioid if you’ve had nausea before. Even if you’ve never had it, ask about it. Prevention beats reaction every time.

Why These Side Effects Matter More Than You Think
These three side effects aren’t just annoying. They’re why so many people stop taking opioids-or misuse them.
The CDC says more than two-thirds of people who misuse prescription opioids do it to relieve pain. Not to get high. To feel better. But if constipation makes them miserable, drowsiness makes them useless, and nausea makes them sick to their stomach, they might skip doses. Or take extra ones to overcome the pain. Or turn to street drugs when their prescription runs out.
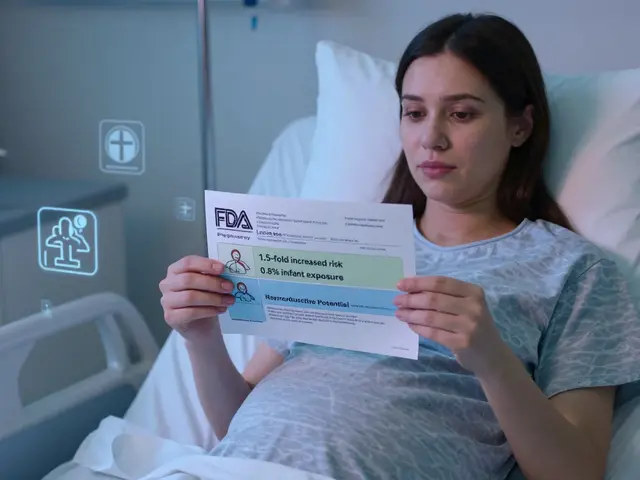
And here’s the hidden risk: when side effects aren’t managed, people are more likely to stop opioids abruptly. That triggers withdrawal. The FDA warns this can lead to uncontrolled pain, panic attacks, and even suicide. That’s not an exaggeration. It’s a documented danger.
Proactive management isn’t optional. It’s part of the treatment. If your doctor doesn’t talk to you about constipation, drowsiness, and nausea before you start opioids, ask. If they say, “It’ll go away,” push back. It won’t. Not for constipation. And you deserve to feel better-not just in pain, but in your whole body.
What You Can Do Right Now
If you’re on opioids:
- Start a laxative today. Senna + Miralax is a solid first step. No waiting.
- Don’t drive or operate heavy machinery for the first 5 days. Your brain is still adjusting.
- Keep a nausea journal. Note when it happens, what you ate, what meds you took. This helps your doctor pick the right antiemetic.
- Never stop cold turkey. If you want to quit, talk to your doctor about a slow taper.
- Review all your meds with your pharmacist. Many common drugs make these side effects worse.
If you’re a caregiver or family member: watch for signs of confusion, extreme sleepiness, or not going to the bathroom for 3+ days. These are red flags. Call the doctor.

What’s Next for Opioid Side Effect Management
Science is catching up. New drugs like naloxegol (Movantik) and naldemedine (Symproic) are designed to block constipation without affecting pain relief. They’re expensive and not for everyone, but they’re proof that researchers are finally treating side effects as seriously as pain.
There’s also growing interest in “biased agonists”-new opioids that trigger pain relief without activating the brain pathways that cause nausea or constipation. They’re still in trials, but they could change everything.
Until then, the best tool you have is awareness. Know what’s coming. Plan for it. Speak up. Your body isn’t broken. Your treatment just needs better support.
Does constipation from opioids ever go away on its own?
No. Unlike drowsiness or nausea, constipation caused by opioids doesn’t improve with time. It persists as long as you’re taking them. That’s why doctors recommend starting laxatives on day one-waiting only makes it worse and harder to treat.
Can I take over-the-counter laxatives with opioids?
Yes, and you should. Stimulant laxatives like senna and osmotic agents like polyethylene glycol (Miralax) are safe and effective when used together. Avoid bulk-forming laxatives like psyllium-they can make opioid-induced constipation worse by adding bulk without improving movement.
Why do opioids make me feel sleepy even if I take them at night?
Opioids affect your brain’s alertness centers regardless of when you take them. Even nighttime doses can cause lingering drowsiness the next day, especially if you’re sensitive or on a high dose. Try splitting your dose or lowering it slightly-always under your doctor’s guidance.
Is nausea from opioids a sign I’m addicted?
No. Nausea is a direct physical reaction to how opioids interact with your brainstem and gut. It’s not a sign of addiction-it’s a side effect. Many people who take opioids exactly as prescribed still get nauseous. It’s about biology, not behavior.
Can I drink alcohol while taking opioids?
Absolutely not. Alcohol and opioids both depress your central nervous system. Together, they can slow your breathing to dangerous levels-even cause death. This combination is responsible for a large portion of opioid overdose deaths. Avoid alcohol completely while on opioids.
What should I do if I miss a dose and feel withdrawal symptoms like nausea?
Don’t double up to make up for the missed dose. That can cause overdose. Instead, call your doctor. If you’re experiencing withdrawal-nausea, sweating, anxiety, diarrhea-it means your body is dependent. Your provider can help you adjust your schedule or taper safely. Abrupt stops can be dangerous.
Final Thoughts
Opioids are powerful tools. But they’re not magic. They come with real, predictable, and often overlooked side effects. Ignoring constipation, drowsiness, and nausea doesn’t make them go away-it makes your treatment harder, riskier, and less effective. The goal isn’t just to manage pain. It’s to help you live your life. And that means taking care of your whole body, not just the part that hurts.



Sameer Tawde
18 November 2025 - 17:00 PM
Just started opioids after my back surgery and honestly? I was terrified of the side effects. But this post? Lifesaver. Started Miralax + senna day one. No more panic when I haven’t gone in two days. You’re right-it’s not laziness, it’s pharmacology. Thanks for saying it like it is.
Ronald Stenger
19 November 2025 - 18:17 PM
Typical liberal medical advice. Everyone’s so scared of opioids now they treat them like poison. I’ve been on them for 12 years. Constipation? Yeah. So what? I take a laxative. Big deal. Stop coddling people. Pain doesn’t care if you’re ‘uncomfortable.’ You take the medicine and deal with it. That’s America.
Samkelo Bodwana
21 November 2025 - 10:10 AM
Look, I come from a place where pain management is a luxury, not a right. In South Africa, most people never even get to this point-no access to opioids at all. So when I see someone complaining about constipation or drowsiness? I feel a little guilty. But also, I get it. This post is one of the clearest, most practical guides I’ve ever read. The part about not waiting for constipation to hit before acting? That’s gold. If every doctor in my country had this mindset, we’d save so many from unnecessary suffering. Thank you for writing this with such care.
Emily Entwistle
21 November 2025 - 23:51 PM
OMG YES!! 🙌 I was so ashamed to tell my doctor I hadn’t pooped in 5 days… then he just handed me a prescription for Relistor and said, ‘Welcome to the club.’ No judgment. Just science. You’re not broken. You’re just on opioids. 💪❤️
Duncan Prowel
23 November 2025 - 06:43 AM
While the clinical recommendations presented are largely sound and evidence-based, one must consider the epistemological limitations of anecdotal patient reporting in the context of pharmacovigilance. The assertion that constipation 'never goes away' may be statistically accurate within a cohort, yet individual neurogastroenterological variability remains underexplored in current literature. Furthermore, the conflation of pharmacological inevitability with therapeutic inevitability warrants cautious interpretation.
Bruce Bain
23 November 2025 - 14:06 PM
I’m just a regular guy. Had a bad car crash. Got opioids. Got constipated. Got sleepy. Got nauseous. Didn’t know what to do. Found this post. Did what it said. Now I’m not in pain AND I can actually leave the house. No magic. Just good advice. Share this with someone who needs it.
Jonathan Gabriel
23 November 2025 - 16:42 PM
So let me get this straight… you’re telling me that after 30 years of doctors treating pain like it’s a moral failing, we’re finally admitting that opioids cause constipation? Groundbreaking. Next you’ll tell me water is wet and gravity exists. Oh wait-those are already FDA-approved. 😏 Also, ‘trial and error’ for nausea? That’s not a treatment plan, that’s a Russian roulette game with your stomach. And why is no one talking about how these drugs make you feel like a zombie for months? But sure, ‘it fades.’ Right. Just like my will to live.
Don Angel
23 November 2025 - 18:07 PM
I’ve been on opioids for 7 years. Constipation? Managed. Drowsiness? Controlled with timing. Nausea? Ondansetron saved me. But the biggest thing? I didn’t know any of this until I read this post. Why didn’t my doctor tell me? Why is this information so hard to find? It shouldn’t be this hard to get basic info. Please, if you’re reading this-ask your doctor. Don’t wait. Seriously. Don’t wait.
benedict nwokedi
25 November 2025 - 14:41 PM
Of course they’re telling you to take laxatives… because the pharmaceutical companies own the AMA, the FDA, and your doctor’s paycheck. They want you dependent-not just on painkillers, but on laxatives, anti-nausea meds, stimulants… it’s a cycle. They don’t care if you live or die. They care about your insurance billing codes. And now they’ve got you hooked on three drugs instead of one. Wake up.
deepak kumar
27 November 2025 - 02:59 AM
As someone from India who’s seen people suffer because they’re scared of opioids, this is gold. The part about not relying on prune juice? So true. We think ‘natural’ means safe-but your gut doesn’t care if it’s a pill or a fruit. Senna + Miralax works. And yes, talk to your pharmacist. They’re the unsung heroes. Also, if you’re on pain meds, don’t skip doses because you’re embarrassed about constipation. That’s how people end up in worse pain. You’re not weak. You’re human.
Gregory Gonzalez
28 November 2025 - 13:26 PM
How refreshing to see someone actually admit that opioids are just… not that great. But of course, the solution isn’t to fix the drug-it’s to fix the patient’s bowel habits. How convenient. Next, they’ll tell us to just ‘eat more fiber’ while the opioid industry rakes in billions. Truly, the pinnacle of medical innovation: manage the side effect, never question the cause.