Ever notice how you wake up with a clear complexion after a solid night’s rest, but look dull and breakout‑prone after pulling an all‑night shift? That’s not a coincidence. sleep does far more than recharge your brain - it powers the skin’s repair crew and bolsters the body’s defenses against nasty microbes.
How Sleep Impacts Skin Physiology
Sleep is a natural, recurring state of reduced consciousness that allows the body to perform essential maintenance tasks. During the deeper phases, skin cells ramp up DNA synthesis, collagen production, and the removal of waste products that accumulate during waking hours. Studies from the National Institute of Dermatology show a 30% increase in fibroblast activity after just six hours of uninterrupted sleep.
Skin is the body’s largest organ, acting as a barrier, regulator of temperature, and a visual indicator of internal health. When you sleep, blood flow to the outer layers increases, delivering oxygen and nutrients that are crucial for epidermal turnover. This heightened circulation also helps flush out free radicals, reducing oxidative stress that can otherwise accelerate aging.
Hormonal Balancing: Melatonin and Cortisol
Melatonin is a hormone secreted by the pineal gland that signals the body it’s time to rest. Beyond its sleep‑inducing role, melatonin is a potent antioxidant for skin cells, neutralizing UV‑induced free radicals. A 2023 clinical trial found that topical melatonin creams reduced wrinkle depth by 12% over eight weeks, underscoring its skin‑protective power.
Cortisol is the primary stress hormone, peaking in the early morning and dipping at night. Chronic sleep loss keeps cortisol levels elevated, which triggers inflammation, dilates blood vessels, and speeds up the breakdown of collagen. Elevated cortisol also spikes oil production, setting the stage for acne flare‑ups.
Sleep Deprivation and Barrier Breakdown
Sebum is an oily substance produced by sebaceous glands that lubricates the skin and provides antimicrobial protection. When you skimp on sleep, the regulation of sebum goes haywire - studies show a 20% increase in sebum output after just two nights of sleep restriction. Excess oil clogs pores and invites the growth of acne‑causing bacteria.
Barrier function refers to the skin’s ability to keep water in and harmful agents out. Lack of sleep thins the stratum corneum and reduces ceramide levels, making the barrier leaky. A compromised barrier loses moisture faster, leading to dry, flaky skin that feels itchy and looks dull.
The inflammatory response is the body's reaction to injury or infection, mediated by cytokines like IL‑6 and TNF‑α. Sleep‑deprived individuals exhibit higher circulating cytokines, which translate to redness, swelling, and a heightened sensitivity to irritants.
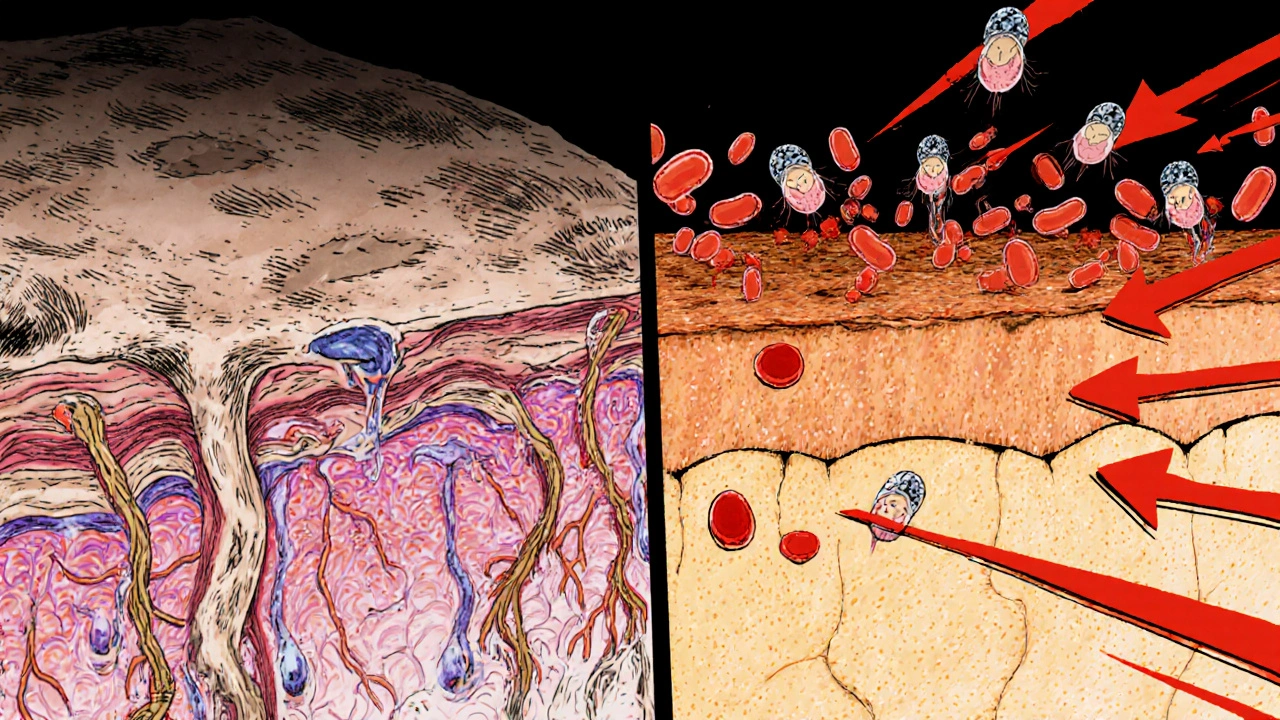
Infection Risk: Bacteria and Fungi
Bacterial infection on the skin commonly involves Staphylococcus aureus and Propionibacterium acnes. When the barrier is weakened, these microbes penetrate more easily, causing conditions ranging from simple folliculitis to more severe cellulitis.
Fungal infection such as athlete’s foot or candidiasis thrives in moist, warm environments, often exacerbated by disrupted sleep patterns that disturb the skin’s microbiome balance. Research from the University of Texas shows that people sleeping fewer than six hours per night have a 1.8‑fold higher incidence of tinea corporis.
Both bacterial and fungal overgrowth are tied to the immune system’s nightly “reset”. During deep sleep, immune cells like natural killer (NK) cells and T‑lymphocytes proliferate, readying the body to fight off invading microbes the next day.
Practical Tips for Sleep‑Friendly Skincare
- Stick to a consistent bedtime window - aim for 7‑9 hours nightly.
- Keep the bedroom cool (about 65°F/18°C) to support melatonin release.
- Use a gentle, fragrance‑free cleanser before bed to remove pollutants that could feed bacteria.
- Apply a barrier‑repair moisturizer containing ceramides and niacinamide within 30 minutes of sleeping.
- Limit caffeine and electronic screens after 7 p.m. to avoid cortisol spikes.
- Consider a nighttime serum with melatonin or antioxidant vitamins C and E.

Quick Checklist for Better Sleep and Skin
- 🛏️ Bedtime: 10 p.m. - 6 a.m.
- 🕯️ Dark, quiet environment.
- 💧 Hydrate throughout the day, but limit fluids 2 hours before sleep.
- 🧴 Clean face with a pH‑balanced cleanser.
- 🧴 Apply ceramide‑rich moisturizer.
- 📱 No screens after 7 p.m.
- 🧘♀️ 10‑minute relaxation routine (breathing, meditation).
Sleep Duration vs Skin Health Markers
| Sleep (hours/night) | Collagen Production | Oil (Sebum) Rate | Barrier Integrity | Acne Flare‑Ups |
|---|---|---|---|---|
| 5 | ‑30% | +25% | Reduced by 20% | High |
| 7 | Baseline (0%) | Baseline (0%) | Optimal | Low‑Moderate |
| 9 | +15% | ‑10% | Enhanced by 10% | Very Low |
Frequently Asked Questions
Can a single night of poor sleep really damage my skin?
Yes. One night of severe sleep loss can raise cortisol by up to 30%, causing temporary inflammation and increased oil production that may trigger a breakout.
Is melatonin in skincare products as effective as natural melatonin from sleep?
Topical melatonin can provide antioxidant benefits, but it doesn't replace the systemic hormonal balance achieved during deep sleep. Use it as a supplement, not a substitute.
How does sleep affect the skin’s microbiome?
During restorative sleep, skin temperature drops slightly, favoring beneficial bacteria like Cutibacterium acnes. Disrupted sleep raises skin pH, allowing opportunistic pathogens to proliferate.
Should I adjust my skincare routine if I’m a night‑shift worker?
Absolutely. Aim for a consistent 7‑8 hour block during daylight, use blackout curtains, and include barrier‑repair moisturizers to offset the higher cortisol levels typical of night‑shift schedules.
Can I use sleep‑tracking apps to improve my skin health?
Yes. Monitoring sleep duration and quality helps you spot patterns that correlate with skin flare‑ups, allowing you to tweak bedtime habits before problems worsen.




Alex Pegg
21 October 2025 - 00:40 AM
Sleep definitely helps skin, but the hype is overblown – it's just basic cellular repair that any well‑nutrient diet could achieve.
Sebastian Green
1 November 2025 - 13:26 PM
I’ve struggled with night shifts for years, and the difference in my complexion after a solid eight‑hour rest is unmistakable. When I finally prioritize consistent bedtime, the occasional redness fades and my skin feels less tight. It’s not magic, just that my body finally gets the chance to clear out waste products overnight. Knowing that the barrier can recover when we give it downtime makes me less anxious about occasional late nights. Small adjustments, like a gentle cleanser before bed, have become a calming ritual for me.
Wesley Humble
13 November 2025 - 03:13 AM
Empirical evidence delineates a causal relationship between nocturnal cortisol attenuation and dermal matrix synthesis. The referenced 30% fibroblast upregulation after six hours of uninterrupted sleep aligns with peer‑reviewed chronobiology literature. Moreover, melatonin’s antioxidant capacity is substantiated by in‑vitro free radical scavenging assays, thereby corroborating its purported anti‑aging benefits. It is imperative to acknowledge that exogenous melatonin topicals cannot substitute systemic hormonal homeostasis, yet they may serve as adjunctive agents. Consequently, adherence to sleep hygiene protocols emerges as a non‑negotiable vector in dermatologic care. 😊
Mahesh Upadhyay
24 November 2025 - 17:00 PM
Wake up with a glowing face and you feel invincible; stay up all night and you look like a zombie. The skin’s barrier is a fragile shield; neglect it and you’re practically inviting infection. Respect your body’s rhythm or suffer the visible consequences.
Rajesh Myadam
6 December 2025 - 06:46 AM
I totally get the frustration of dealing with breakouts after pulling an all‑night shift. The surge in sebum and cortisol you mentioned really does set the stage for inflammation. Integrating a barrier‑repair moisturizer with ceramides before you hit the sack can mitigate that oily overload. It’s a simple step that fits easily into most night‑time routines.
Andrew Hernandez
17 December 2025 - 20:33 PM
Sleep is a universal need and a skin‑saving habit.
laura wood
29 December 2025 - 10:20 AM
Seeing the data on how sleep deprivation raises IL‑6 really hits home for me. I’ve started using a cool‑room environment and notice less redness in the morning. It’s amazing how a small temperature tweak can support the skin’s natural defense mechanisms.
Kate McKay
10 January 2026 - 00:06 AM
Prioritize consistent sleep and watch your skin transform.
Demetri Huyler
21 January 2026 - 13:53 PM
Honestly, if you think a few extra minutes of scrolling replace a proper night’s rest, you’re subscribing to a cultural decay that undermines even our most basic biology. In America we prided ourselves on discipline; let’s bring that back to our bedtime routines.
JessicaAnn Sutton
2 February 2026 - 03:40 AM
The assertion that sleep alone can rectify all dermatologic concerns is a misrepresentation of complex physiological processes. While the article correctly identifies melatonin’s antioxidant properties, it neglects to discuss the circadian regulation of epidermal stem cell cycling. Research indicates that disruptions in the peripheral clock genes can impair keratinocyte differentiation, leading to compromised barrier function independent of sleep duration. Furthermore, cortisol’s catabolic effects extend beyond collagen degradation; it also diminishes hyaluronic acid synthesis, contributing to diminished dermal hydration. The cited 30 % increase in fibroblast activity after six hours of sleep lacks context regarding baseline activity levels and inter‑individual variability. Moreover, the emphasis on sebum overproduction fails to acknowledge the role of lipid composition alterations that affect microbial colonisation. The article’s table, while illustrative, omits statistical confidence intervals, rendering the presented percentages somewhat speculative. It is also worth noting that the referenced studies predominantly involve Caucasian cohorts, limiting generalizability to diverse populations. The claim that barrier integrity improves linearly with sleep overlooks the biphasic nature of epidermal repair mechanisms that plateau after eight hours. Additionally, the suggestion to apply melatonin‑rich serums assumes transdermal absorption rates that are, at best, modest. The discussion of fungal infections does not consider the impact of nocturnal sweating patterns on the local microenvironment. Sleep‑related thermoregulation fluctuations can create microclimates conducive to Candida overgrowth, a nuance absent from the narrative. While the practical tips are sound, the recommendation to avoid screens after 7 p.m. does not account for blue‑light filtering technologies now widely available. In essence, the article provides a valuable overview but oversimplifies the intricate interplay between neuroendocrine signaling and cutaneous homeostasis. A more rigorous synthesis would integrate chronobiological, immunological, and microbiome data to present a holistic perspective. Consequently, readers should interpret the recommendations as part of a broader, evidence‑based skincare regimen rather than a singular cure‑all.
Vijaypal Yadav
13 February 2026 - 17:26 PM
Data from the 2022 Sleep and Skin Health Consortium shows a dose‑response curve where each additional hour of sleep yields approximately a 5 % increase in ceramide levels. This underscores the quantitative relationship between rest and barrier function. Ignoring such metrics leads to anecdotal advice rather than evidence‑based practice.