Cyclosporine Level Checker
Enter your information above to see if your levels are within target range.
When you take cyclosporine after a transplant, your body needs just the right amount-too little and your immune system attacks the new organ; too much and your kidneys start to fail. This isn’t a guess game. It’s science with real stakes. About 30 to 50% of long-term kidney transplant failures are tied to poorly managed cyclosporine levels, according to the NCBI StatPearls 2023 update. That’s not a small number. It’s the difference between keeping your transplant working for 10 years or losing it in 3.
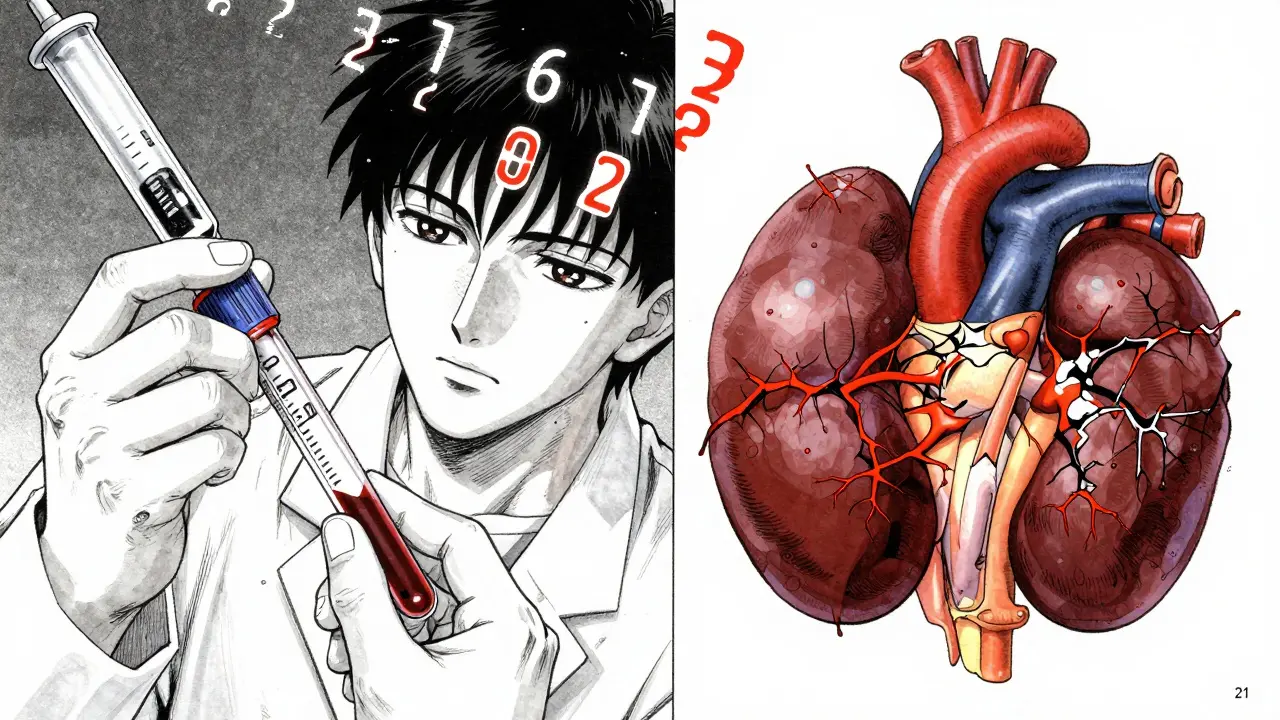
What Makes Cyclosporine So Dangerous for Your Kidneys?
Cyclosporine isn’t just any drug. It’s a calcineurin inhibitor, designed to silence your immune system so your body doesn’t reject the new kidney, heart, or liver. But it doesn’t know the difference between a bad cell and a good one. It attacks blood vessels in the kidneys, tightening them up and cutting off blood flow. This is called renal vasoconstriction. The result? Your kidneys can’t filter waste properly. Creatinine rises. Blood pressure climbs. Magnesium drops. And over time, permanent scarring sets in.
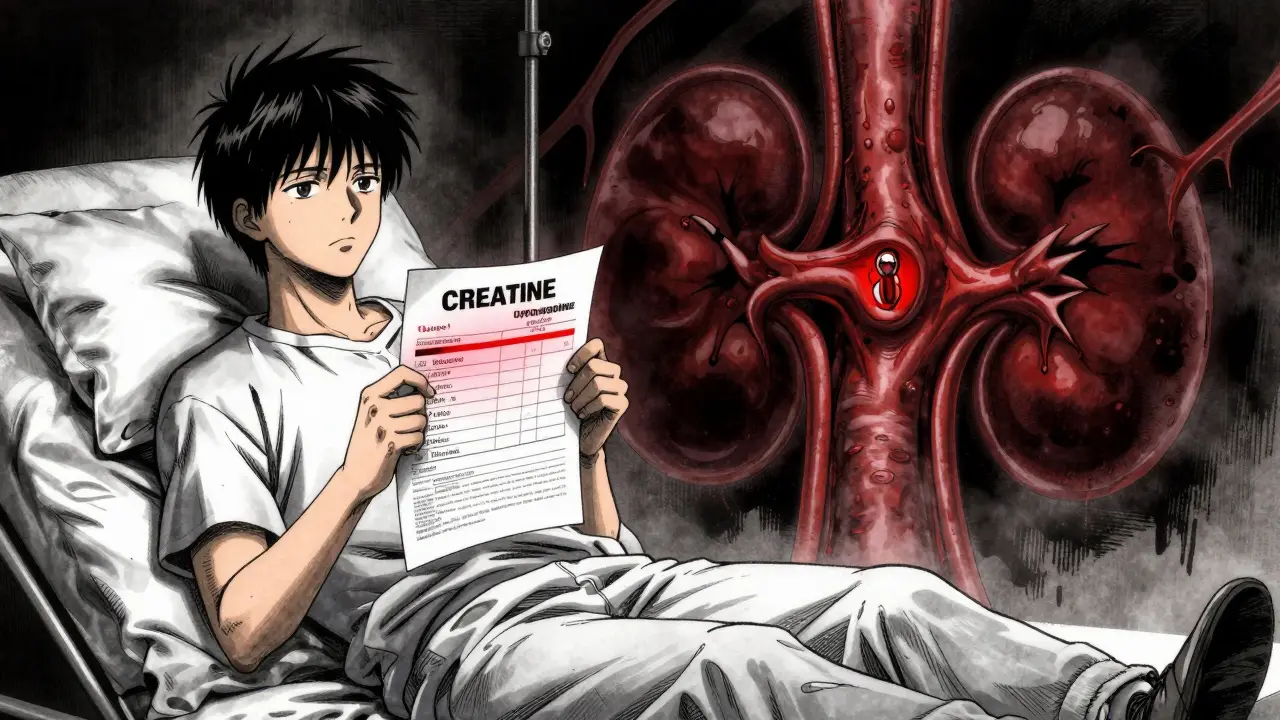
Early signs are quiet. You might feel fine. Your urine looks normal. But your blood tests tell the real story. A serum creatinine level above 1.5 mg/dL is a red flag. A BUN-to-creatinine ratio over 20:1 means your kidneys are under strain. High blood pressure-above 130/80 mmHg-is another warning sign. These aren’t just numbers. They’re your kidneys screaming for help.
Structural damage shows up as arteriolar hyalinosis and tubular vacuolization-terms you won’t hear in everyday conversation, but they mean your kidney’s tiny filtering units are dying. The good news? If caught early, this damage can reverse. Studies from the 1980s, like J. Chapman’s 1985 Lancet paper, showed that reducing cyclosporine doses within three months of early signs led to kidney recovery in most patients.
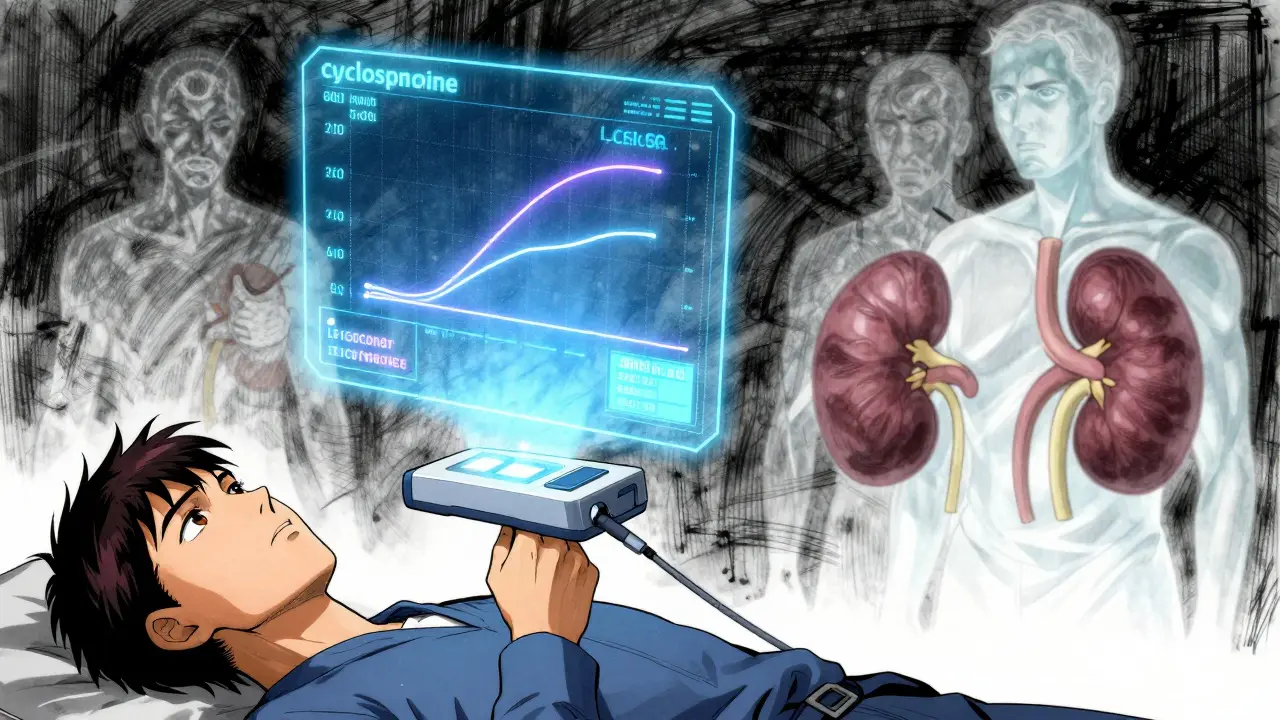
How Do Doctors Measure Cyclosporine Levels?
Measuring cyclosporine isn’t like checking your blood sugar. You can’t use a fingerstick. You need a blood draw-and the right kind of tube. EDTA tubes are mandatory. Serum separator tubes? They give falsely high results by 15-20%. That’s not a typo. That’s a dangerous mistake.
There are three main ways labs measure cyclosporine: immunoassays, HPLC, and LC-MS/MS. For years, most labs used non-isotopic immunoassays because they’re fast and cheap-around $15 to $25 per test. But here’s the catch: they can’t tell the difference between cyclosporine and its metabolites. That means if your body breaks down the drug into similar-looking compounds, the machine reads them as cyclosporine. Result? Your level looks higher than it really is. You might get your dose cut, and then your body rejects the transplant.
HPLC was the gold standard for accuracy, but it’s slow and expensive-$35 to $50 per test, with results taking 6 to 8 hours. Today, almost all U.S. transplant centers use LC-MS/MS. It’s faster than HPLC, more accurate than immunoassays, and can detect levels as low as 5 ng/mL. It’s the only method that gives you the real picture.
According to a 2021 American Journal of Transplantation review, 92% of centers now use LC-MS/MS. That’s a huge shift from 2002, when 85% still used less reliable methods. The change saved lives.
What Are the Right Cyclosporine Levels?
There’s no single number that works for everyone. Your target depends on your transplant type, how long ago it happened, and whether you’re an extensive or poor metabolizer of the drug.
For a kidney transplant:
- First week: 200-400 ng/mL
- Weeks 2-6: 125-275 ng/mL
- Months 7-12: 100-150 ng/mL
- After 1 year: 75-160 ng/mL
For heart or liver transplants, the targets are similar: 250-350 ng/mL for the first six months, then 100-200 ng/mL long-term.
But here’s the twist: some people break down cyclosporine faster than others. That’s because of a gene called CYP3A5. If you’re an extensive metabolizer (about 50% of people), you need 30-40% more drug to reach the same blood level as someone who metabolizes it slowly. The 2023 KDIGO guidelines now recommend testing for this gene before starting treatment. No more guessing.
Traditionally, doctors checked levels right before your next dose-called C0 (trough). But newer research shows that measuring the level 2 hours after your dose-C2-is a better predictor of how much drug your body actually absorbed. Studies from 2018 show C2 monitoring reduces acute rejection by nearly 18%. And since 2022, European data confirms it cuts nephrotoxicity by over 22%.
How Often Should You Get Tested?
Monitoring isn’t a one-time thing. It’s a rhythm.
- First month after transplant: twice a week
- Months 2-6: once a week
- Months 7-12: every two weeks
- After year one: monthly or as needed
But timing matters. If you’re on C2 monitoring, you have to take your dose at the same time every day. Then, exactly two hours later, you go for the blood draw. No food, no coffee, no extra meds-unless your doctor says otherwise. Even small changes throw off the numbers.
It takes 4 to 6 weeks for your blood levels to stabilize after a dose change. That means if your doctor adjusts your pill amount, you can’t expect immediate results. Patience is part of the treatment.
What Drugs Can Mess With Cyclosporine?
Cyclosporine doesn’t play well with others. It’s broken down by liver enzymes-CYP3A4, mostly. So anything that affects those enzymes changes your cyclosporine level.
Drugs that boost cyclosporine levels:
- Ketoconazole (antifungal): increases levels by 30-50%
- Verapamil (blood pressure pill): increases by 20-40%
- Clarithromycin (antibiotic): increases by 30-50%
Drugs that drop cyclosporine levels:
- Rifampin (TB drug): cuts levels by 40-60%
- Phenytoin (seizure drug): reduces by 30-50%
- St. John’s Wort (herbal supplement): cuts levels by up to 50%
Even grapefruit juice can raise your levels. One glass in the morning can cause a spike. That’s why transplant teams give you a strict list of what to avoid.
What Else Should You Watch For?
Beyond creatinine and blood pressure, other markers matter:
- Magnesium: Cyclosporine makes your kidneys dump magnesium. Levels below 1.7 mg/dL are common. Low magnesium causes muscle cramps, irregular heartbeat, and fatigue. Supplementing helps-but only under supervision.
- Uric acid: Cyclosporine can raise uric acid, leading to gout. Not everyone gets it, but if you notice swollen, painful toes, tell your doctor.
- Fluid retention: Swelling in ankles or face? Could be kidney-related. Or it could be from high blood pressure meds. Only testing tells you which.
Some patients develop tremors, headaches, or gum overgrowth. These aren’t kidney issues, but they’re side effects too. Don’t ignore them. They’re clues your dose might be too high.
What’s Next for Cyclosporine Monitoring?
The future is here. Labs are testing AI algorithms that track 17 different factors-your weight, age, liver function, genetic profile, even your diet-and predict your ideal dose with 89.7% accuracy. Early trials show this could cut blood draws in half without risking rejection or toxicity.
Point-of-care devices are also in Phase 3 trials. Imagine a handheld machine at your doctor’s office that gives you your cyclosporine level in 10 minutes, using just a drop of blood. FDA approval is expected by late 2025. That’s a game-changer for people who live far from transplant centers.
For now, the rules are simple: know your numbers. Stick to your schedule. Tell your doctor about every new pill, supplement, or even herbal tea. Your kidney isn’t just an organ-it’s your second chance. And cyclosporine? It’s a powerful tool. But only if you use it right.
Can cyclosporine nephrotoxicity be reversed?
Yes, if caught early. Studies from the 1980s show that reducing the cyclosporine dose within three months of early kidney damage signs-like rising creatinine or high blood pressure-can lead to partial or full recovery of kidney function. But if the damage is left untreated for over a year, scarring becomes permanent. Early detection is everything.
Is LC-MS/MS testing better than immunoassays for cyclosporine?
Yes, significantly. LC-MS/MS is 99.2% specific and can detect levels as low as 5 ng/mL. Immunoassays, used by most labs until recently, can’t distinguish between cyclosporine and its metabolites, leading to falsely high readings in 10-15% of cases. That means patients were often given lower doses than needed, increasing rejection risk. LC-MS/MS is now the standard in 92% of U.S. transplant centers.
Why do I need to take cyclosporine at the same time every day?
Cyclosporine has high variability in how your body absorbs it. Taking it at inconsistent times makes blood levels unpredictable. For accurate monitoring-especially C2 testing-you need to take your dose at the exact same time each day. This ensures your lab results reflect your true drug exposure, not random fluctuations from timing errors.
Can I take grapefruit juice with cyclosporine?
No. Grapefruit juice blocks the liver enzyme that breaks down cyclosporine, causing levels to spike by up to 50%. Even a single glass can push you into toxic range. The same applies to pomelo, Seville oranges, and some herbal supplements. Always check with your transplant team before trying anything new.
How do I know if my cyclosporine level is too high?
Symptoms of high levels include shaking hands, headaches, nausea, high blood pressure, swelling in your legs or face, and a rising creatinine level on blood tests. But often, there are no symptoms until kidney damage is advanced. That’s why regular blood tests are non-negotiable. Never adjust your dose based on how you feel-only on lab results.
Is cyclosporine still used today, or have newer drugs replaced it?
Cyclosporine is still used in about 150,000 transplant patients annually in the U.S. Newer drugs like tacrolimus are more common because they’re slightly more effective and less toxic. But cyclosporine remains vital for patients who can’t tolerate tacrolimus due to side effects like diabetes or neurological issues. It’s not outdated-it’s specialized.
What happens if I miss a dose of cyclosporine?
If you miss a dose, take it as soon as you remember-if it’s within a few hours of your scheduled time. If it’s close to your next dose, skip the missed one. Never double up. Missing doses increases rejection risk. But frequent missed doses or erratic timing can also cause dangerous spikes in levels when you catch up. Consistency is more important than perfection.
Do I need to avoid all supplements while on cyclosporine?
Not all, but many. St. John’s Wort, echinacea, garlic pills, and high-dose vitamin E can interfere with cyclosporine levels. Even common vitamins and minerals can interact. Always tell your transplant team about every supplement, herb, or over-the-counter product you take. They’ll tell you what’s safe.
Final Thoughts: Stay in Control
Cyclosporine is a lifeline. But it’s also a tightrope. You need to walk it carefully. The numbers don’t lie. Your kidneys are telling you something every time you get blood drawn. Listen. Follow your schedule. Know your meds. Ask questions. Don’t let a missed test or a misunderstood side effect cost you your transplant. This isn’t just about taking a pill. It’s about protecting the second chance you were given.




Nisha Marwaha
30 December 2025 - 16:33 PM
Cyclosporine nephrotoxicity is a classic example of pharmacodynamic precision requiring therapeutic drug monitoring (TDM) at the molecular level. The renal vasoconstriction mediated by endothelin-1 upregulation and nitric oxide suppression is well-documented in calcineurin inhibitor toxicity. LC-MS/MS remains the gold standard due to its specificity for the parent compound versus hydroxylated metabolites-immunoassays overestimate by 15–20% due to cross-reactivity with M1, M9, and M17 metabolites. C2 monitoring has demonstrated superior correlation with AUC(0–4) than C0, reducing acute rejection by 18% in prospective trials. Genetic polymorphisms in CYP3A5*3 significantly alter clearance; non-expressors require 30% lower doses. Magnesium wasting is underappreciated-hypomagnesemia exacerbates nephrotoxicity via renal tubular dysfunction. Always rule out drug interactions: azoles, calcium channel blockers, and macrolides inhibit CYP3A4, while rifampin and St. John’s wort induce it. The future lies in AI-driven pharmacokinetic modeling integrating genomics, renal function, and concomitant meds-early data shows 89.7% predictive accuracy.
Paige Shipe
30 December 2025 - 23:45 PM
Anyone who thinks cyclosporine is outdated clearly hasn't read the 2023 KDIGO guidelines or the 2021 AJT meta-analysis. Tacrolimus might be more popular, but cyclosporine is still the backbone for patients with tacrolimus-induced diabetes or neurotoxicity. The data on C2 monitoring reducing nephrotoxicity by 22% is irrefutable. And yes, grapefruit juice is a hard no-seriously, it's not a rumor, it's in the FDA labeling. If you're on this drug, you don't get to be casual about timing or diet. Your kidney isn't a suggestion, it's your lifeline. And no, you can't just skip a blood test because you're 'feeling fine.' That's how you end up with chronic allograft nephropathy.
Amy Cannon
31 December 2025 - 11:56 AM
It is truly remarkable, and indeed profoundly instructive, to observe the evolution of cyclosporine monitoring from the crude immunoassay methodologies of the 1990s to the exquisitely precise LC-MS/MS platforms now employed in virtually every major transplant center in the United States. The shift from C0 to C2 monitoring represents not merely a technical refinement but a paradigmatic transformation in therapeutic precision, wherein pharmacokinetic exposure is quantified not at the nadir of absorption but at the point of maximal bioavailability, thereby allowing for more accurate dose titration and a significant reduction in both rejection and toxicity. Moreover, the integration of pharmacogenomic data regarding CYP3A5 expression status has rendered the era of empirical dosing obsolete. One must also acknowledge the insidious nature of nephrotoxicity-often asymptomatic until structural damage is irreversible-and the critical importance of longitudinal monitoring of serum magnesium, uric acid, and blood pressure as early biomarkers of renal stress. The future, as noted, lies in point-of-care diagnostics and AI-driven predictive modeling, which may soon render the current protocol of biweekly blood draws antiquated.
Himanshu Singh
1 January 2026 - 04:01 AM
Man, this post is a lifesaver. I’ve been on cyclosporine for 4 years and I had no idea about C2 monitoring or the grapefruit juice thing. My doc just told me to take it at breakfast and come back in a month. Now I know why my levels were all over the place. Also, I’ve been taking magnesium supplements since my cramps started-turns out that’s legit. Thanks for laying it out so clear. I’m gonna print this out and bring it to my next appt.
Jasmine Yule
1 January 2026 - 18:51 PM
I’m so glad someone finally wrote this in plain terms. I spent six months thinking my kidney was failing because I was ‘doing something wrong’-turns out my levels were just being misread because they used the wrong blood tube. I cried when I found out. If you’re on this drug, please, please, please ask your lab if they’re using EDTA tubes and LC-MS/MS. And yes, grapefruit juice is a dealbreaker. I learned that the hard way after one glass. I’m not mad-I’m just really, really careful now. This isn’t just medicine. It’s survival.
Greg Quinn
2 January 2026 - 16:36 PM
There’s something almost poetic about how a molecule designed to silence the immune system ends up silently killing the very organ it’s meant to protect. Cyclosporine is a paradox wrapped in a pill-both savior and saboteur. The fact that we’ve learned to measure it with such precision, that we now know to check C2 levels and screen for CYP3A5 variants, speaks to how far we’ve come in understanding biological complexity. But the real lesson isn’t in the lab values. It’s in the discipline. The timing. The refusal to take shortcuts. Your kidney doesn’t care if you’re tired, busy, or confused. It just asks for consistency. And in a world that rewards speed, maybe that’s the most radical thing we can do: show up, on time, every day.
Lisa Dore
4 January 2026 - 03:51 AM
This is the kind of post that makes me believe in the power of patient education. I used to think all transplant meds were just ‘take it and hope.’ But this? This is science with soul. I’ve shared this with my support group-three of us are on cyclosporine, and we’ve all started asking our labs about LC-MS/MS and EDTA tubes. One lady even got her pharmacy to switch her blood draw protocol. We’re not just patients anymore-we’re advocates. And honestly? That’s the best part of surviving this. Not just living-but learning how to fight smart.
Henriette Barrows
5 January 2026 - 06:19 AM
Wait-so if I take my cyclosporine at 8am, I have to get blood drawn at 10am? No coffee, no food, nothing? That’s… actually kind of doable. I thought they just wanted it before my morning dose. I’ve been doing it wrong for two years. I’m gonna call my clinic tomorrow and ask if they do C2 monitoring. Also, I had no idea magnesium was a thing. I’ve been getting leg cramps since March. Maybe that’s why. I’m gonna ask for a level check. Thanks for the info. Seriously. This helped.
Alex Ronald
5 January 2026 - 16:29 PM
One thing the post doesn’t mention but is critical: the psychological toll of constant monitoring. You’re not just managing a drug-you’re managing anxiety. Every blood test feels like a verdict. I’ve been on cyclosporine for 8 years. I know my numbers. I know my limits. But I still check my urine color before every appointment. I still avoid restaurants. I still Google every new symptom. This isn’t just clinical-it’s existential. The science is solid. But the human cost? That’s the part no guideline can quantify.
Teresa Rodriguez leon
6 January 2026 - 08:07 AM
So let me get this straight-you’re telling me I can’t even have a glass of orange juice? And I’ve been taking garlic pills for my cholesterol? I’m so mad at my doctor for never telling me this. Now my creatinine is up and I’m scared. This is why I hate transplant medicine. No one tells you the full story until it’s too late.