Opioid Withdrawal Timeline Calculator
Important: Medical supervision is strongly recommended. Withdrawal can be dangerous without proper care.
When someone stops using opioids after regular use, their body doesn’t just adjust quietly. It reacts. Hard. Opioid withdrawal isn’t a choice-it’s a physical reality. And while it’s not usually deadly for healthy adults, it’s one of the most uncomfortable experiences a person can go through. Knowing what to expect and how to handle it can mean the difference between giving up and getting through.
When Do Withdrawal Symptoms Start?
The clock starts ticking the moment you take your last dose. But the timing depends on what kind of opioid you were using. For short-acting drugs like heroin, oxycodone, or hydrocodone, symptoms usually show up within 8 to 12 hours. You might feel restless, anxious, or start yawning nonstop. Your nose runs. Your eyes water. You can’t sleep. These early signs are easy to miss-people often think they’re just getting a cold. With long-acting opioids like methadone or extended-release oxycodone, the wait is longer. Symptoms don’t show up until 24 to 36 hours after the last dose. That delay can be misleading. Some people think they’re fine because they don’t feel sick right away. But when the symptoms hit, they hit hard-and they last longer.What Does Opioid Withdrawal Feel Like?
Withdrawal isn’t one thing. It’s a cascade of physical and emotional symptoms that build over days. In the first 1 to 3 days, it’s mostly physical: muscle aches, stomach cramps, nausea, vomiting, diarrhea, sweating, chills, and a racing heart. Your pupils widen. You get goosebumps even in a warm room. Sleep disappears. The body feels like it’s being pulled apart from the inside. By day 3 to 5, the worst of the physical symptoms peak. Many people describe this time as the most intense period-like having the flu, but amplified tenfold. You can’t sit still. You feel weak. Your bones ache. You’re exhausted but can’t rest. This is also when anxiety and depression often spike. Some people feel hopeless. Others panic. The urge to use again becomes overwhelming. After day 7, most of the physical symptoms begin to fade. Nausea slows. Diarrhea stops. Sweating eases. But the emotional toll lingers. Irritability, low mood, trouble concentrating, and insomnia can stick around for weeks. This is why so many people relapse-not because they can’t handle the physical pain, but because the emotional emptiness feels unbearable.How Long Does Opioid Withdrawal Last?
There’s no single answer. For most people using short-acting opioids, the acute phase lasts about 7 to 10 days. After that, the body starts to stabilize. But for those on methadone or long-acting prescriptions, withdrawal can stretch to 14 days or even longer. The physical symptoms may fade, but the brain doesn’t reset overnight. The truth is, withdrawal doesn’t end when the last symptom disappears. For many, the real challenge begins after the first two weeks. Cravings, sleep problems, and emotional instability can persist for months. This is called Post-Acute Withdrawal Syndrome (PAWS). It’s not dangerous, but it’s real. And without support, it can lead to relapse.
Medical Help Makes All the Difference
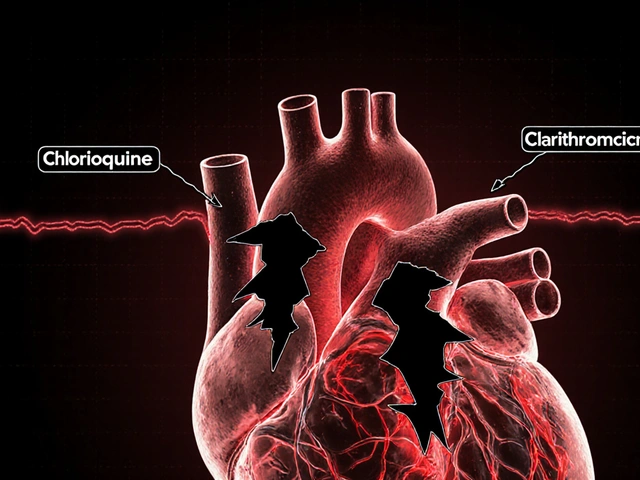
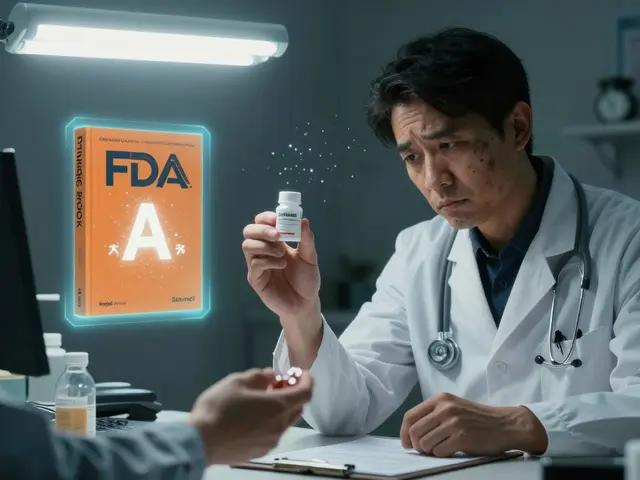
Going through withdrawal alone is risky. Dehydration from vomiting and diarrhea can lead to dangerous electrolyte imbalances. Heart rhythm problems can develop. And the risk of overdose after detox is 3 to 5 times higher because your tolerance drops fast. That’s why medical supervision matters. Clinics use tools like the Clinical Opioid Withdrawal Scale (COWS) to measure severity. It scores 11 symptoms-from sweating to anxiety-on a scale from 0 to 47. A score above 37 means severe withdrawal. That’s when medication becomes critical. Three FDA-approved medications are the gold standard: methadone, buprenorphine, and naltrexone. Buprenorphine, especially in the form of Suboxone, reduces withdrawal symptoms by 60 to 70% in clinical trials. It works by calming the nervous system without causing the same high as other opioids. Methadone does something similar but requires daily clinic visits. Naltrexone blocks opioids entirely but can only be started after full detox-so it’s not used during withdrawal itself. The biggest shift in treatment? You don’t need to suffer through withdrawal to start medication. A decade ago, patients had to go cold turkey before getting help. Now, experts like Dr. Nora Volkow from NIDA say: start medication as soon as someone is ready. No more punishment. No more waiting. Just care.What You Can Do at Home (With Medical Guidance)
Even with medical help, your own actions matter. Hydration is non-negotiable. Drink at least 2.5 liters of fluids a day-water, broth, or oral rehydration solutions. Electrolytes lost through vomiting and diarrhea need replacing. Coconut water, sports drinks, or electrolyte powders help. Eat small, easy meals. Bananas, rice, toast, and yogurt are gentle on the stomach. Avoid caffeine and sugar-they make anxiety and insomnia worse. Non-drug tools help too. Acupuncture has been shown in studies to reduce withdrawal symptoms by 25 to 30% in two-thirds of participants. Gentle movement like walking or stretching can ease muscle pain and improve sleep. Meditation and breathing exercises reduce panic and help with emotional regulation. Tapering, not quitting cold turkey, cuts symptom severity by up to 80%. If you’re on a prescription opioid, your doctor should create a step-by-step plan-cutting your dose by 10 to 20% every 3 to 7 days. This isn’t weakness. It’s strategy.What Doesn’t Work
There are a lot of myths. Cold turkey? It’s brutal and often fails. Most people relapse within days. Klonopin or Xanax to calm nerves? Dangerous. Mixing benzodiazepines with opioids increases overdose risk. Alcohol to “soothe” symptoms? It worsens dehydration and depression. Herbal remedies like kratom? Unregulated, unpredictable, and can lead to dependence of their own. The truth is simple: there’s no shortcut. Recovery isn’t about getting through withdrawal. It’s about building a life after it.
Why Most People Relapse After Withdrawal
Detox alone fixes the body. It doesn’t fix the mind. Studies show only 20 to 25% of people stay off opioids after detox without ongoing treatment. But when they continue with medication-assisted treatment-like buprenorphine or methadone-for at least 6 to 12 months, success rates jump to 40 to 60%. Relapse isn’t failure. It’s a sign the treatment didn’t go far enough. Withdrawal is just the first step. Real recovery needs counseling, support groups, housing help, job training-things that rebuild a life beyond the drug.Where to Get Help Now
Access is improving. The 2021 MAT Act let any licensed doctor prescribe buprenorphine-no special waiver needed. That opened the door for 1 million more providers. Community health centers now receive federal funding to expand services. The Biden administration has invested $30 million to bring withdrawal care to places that need it most. If you or someone you know is ready to stop opioids, don’t wait. Call a local clinic. Talk to your doctor. Use SAMHSA’s helpline (1-800-662-HELP). You don’t have to do this alone. And you don’t have to suffer to earn help.Is opioid withdrawal life-threatening?
For most healthy adults, opioid withdrawal is not life-threatening. But complications like severe dehydration, electrolyte imbalances, or heart rhythm issues can become dangerous without medical care. The biggest risk isn’t the withdrawal itself-it’s the increased chance of fatal overdose after detox, when tolerance drops.
How long does it take to feel better after quitting opioids?
Physical symptoms usually peak within 3 days and begin to fade after a week. Most people feel significantly better by day 7 to 10. But emotional symptoms like anxiety, depression, and trouble sleeping can last for weeks or months. This is normal. Support and ongoing treatment help manage these longer-term effects.
Can I detox from opioids at home?
It’s possible, but risky. Without medical supervision, you could develop dangerous dehydration, heart problems, or relapse due to unbearable symptoms. Medical detox improves success rates from under 50% to over 85%. If you’re considering home detox, talk to a doctor first. Tapering and medications can make it safer.
What’s the best medication for opioid withdrawal?
Buprenorphine (like Suboxone) is the most commonly used and effective option. It reduces withdrawal symptoms by 60-70%, has a lower risk of misuse than methadone, and can be prescribed by most doctors. Methadone is also effective but requires daily clinic visits. Naltrexone blocks opioids but can’t be used until you’re fully detoxed.
Why do people relapse after opioid withdrawal?
Withdrawal clears the body of opioids, but it doesn’t fix the brain’s cravings or emotional pain. Without ongoing treatment-like counseling, support groups, or continued medication-most people return to use because the underlying issues remain. Studies show that continuing medication-assisted treatment for 6 to 12 months after detox doubles the chance of long-term recovery.
Can I use marijuana or kratom to ease opioid withdrawal?
Marijuana may help with sleep or appetite, but it doesn’t address the core neurological changes of opioid withdrawal. Kratom is unregulated, can cause its own dependence, and may interact dangerously with other medications. Neither is a safe or proven substitute for medically supervised treatment. Stick to evidence-based options.
How do I know if I need medical detox?
If you’ve been using opioids daily for more than a few weeks, if you’re taking high doses, or if you have other health conditions like heart disease, liver problems, or mental illness-you need medical detox. Even if you think you can handle it, professional care reduces risks and increases your chances of success.



Gavin Boyne
2 December 2025 - 01:04 AM
Let’s be real-withdrawal isn’t some Hollywood drama. It’s a brutal neurological reset. The body doesn’t ‘get over’ opioids like a cold. It rewires. And if you think willpower alone fixes that, you’ve never sat through day three without moving. The science here is solid: buprenorphine isn’t a crutch, it’s a bridge. And anyone who calls it ‘substituting one drug for another’ hasn’t read a single clinical trial in the last decade.
Medication-assisted treatment isn’t about convenience. It’s about survival. Your brain needs time to stop screaming for a chemical that no longer exists. You don’t heal from addiction by suffering. You heal by stabilizing.
And yes, the emotional fog lasts longer than the cramps. That’s not weakness. That’s neurochemistry. Stop glorifying cold turkey. It’s not bravery. It’s ignorance dressed up as grit.
shalini vaishnav
3 December 2025 - 12:11 PM
India has been dealing with this for decades and still no real policy. Westerners act like they discovered harm reduction. We’ve had community-led detox centers in rural Maharashtra since the 90s. No fancy clinics. Just people helping people. You don’t need a doctor to hydrate someone. You need compassion. And yet, the world still treats this like a Western invention.
Stop romanticizing American medicine. We’ve been managing this without insurance or FDA approval. Your ‘gold standard’ is just a luxury most of the world can’t afford.
Joykrishna Banerjee
5 December 2025 - 09:37 AM
Let me correct the semantic misdirection in the original post: ‘withdrawal isn’t a choice’ is a misleading anthropomorphization. The body doesn’t ‘react’-it responds biochemically. And ‘uncomfortable’ is a gross understatement. It’s autonomic dysregulation on a systemic level.
Furthermore, the COWS scale is flawed. It ignores somatic symptom clustering and overweights psychological indicators. A score of 37 doesn’t equal ‘severe’-it equals ‘clinically significant.’ Precision matters. And no, kratom isn’t a ‘dependence of its own’-it’s a partial mu-agonist with a ceiling effect. The demonization is politically motivated.
Also, why is naltrexone mentioned as a withdrawal tool? It’s contraindicated until detox is complete. This post is riddled with clinical inaccuracies masked as authority.
Rashi Taliyan
6 December 2025 - 01:51 AM
I lost my brother to this. Not from overdose. From despair after detox. He made it through the physical hell-vomiting, shaking, sleepless nights-but when the silence came… he couldn’t bear it. No one talked to him. No one asked how he felt. Just ‘you’re clean now, good job.’
That silence killed him.
If you’re reading this and you’re thinking about quitting-please, don’t do it alone. Find a group. Call someone. Text a stranger on a recovery subreddit. You don’t have to be strong. You just have to stay present.
I’m still here. And I’m still fighting. Every day.
Kara Bysterbusch
7 December 2025 - 18:27 PM
Thank you for this meticulously researched and empathetically framed exposition. The integration of neurobiological data with psychosocial context is exemplary. Particularly illuminating is the delineation between acute withdrawal and PAWS-too often conflated in popular discourse.
I would respectfully suggest augmenting the section on home management with a brief note on circadian rhythm regulation: exposure to natural light within 30 minutes of waking has been shown in randomized trials to reduce insomnia severity by up to 40% during early recovery. A simple, non-pharmacological intervention with profound downstream effects on mood stabilization.
This is precisely the kind of public health communication we need: accurate, accessible, and devoid of moralizing.
Rashmin Patel
8 December 2025 - 11:14 AM
Okay, real talk: if you're reading this and you're still thinking about quitting cold turkey, stop. Just stop. I've seen too many people think they're tough enough, and then they end up in the ER because they passed out from dehydration or tried to self-medicate with benzos and ended up in a coma.
And yes, buprenorphine works. I was on 12mg a day for six months. Didn't feel high. Didn't feel numb. Just… human again. The cravings didn't vanish, but they became manageable. Like a storm you can see coming-you don't have to run into it.
Also, acupuncture? YES. I did it twice a week. Felt like my body was finally listening to me again. And walking? 10 minutes a day. Just outside. Sunlight. Fresh air. Doesn't sound like much, but it’s the first time in years I didn't feel like I was inside a cage.
You don't have to be perfect. You just have to show up. One day. One hour. One breath.
sagar bhute
9 December 2025 - 07:49 AM
Everyone here is acting like this is some noble struggle. It’s not. It’s a failure. A personal collapse. You chose the drug. You chose the lifestyle. Now you want a medal for not dying?
People don’t relapse because of ‘emotional emptiness.’ They relapse because they’re weak. They’re lazy. They don’t want to work. Recovery isn’t about ‘building a life’-it’s about choosing to live like an adult.
And don’t give me this ‘medication-assisted treatment’ nonsense. You’re just trading one addiction for another. Methadone clinics are just opioid factories with better lighting.
Stop coddling addicts. Start holding them accountable. No one owes you a second chance. You earn it by getting up and going to work. Not by sitting in a group circle crying about trauma.
Cindy Lopez
9 December 2025 - 11:04 AM
Grammar error in the third paragraph: ‘You might feel restless, anxious, or start yawning nonstop. Your nose runs. Your eyes water. You can’t sleep.’
‘Your nose runs’ is not a complete sentence. It’s a fragment. And ‘nonstop’ should be hyphenated as ‘non-stop’ when used adverbially.
Also, ‘3 to 5 times higher’-what’s the baseline? Unclear. Needs citation.
This article reads like a well-meaning draft. Not a final product. Tone is inconsistent. One moment clinical, the next poetic. It’s not professional. It’s amateurish.
James Kerr
9 December 2025 - 14:35 PM
Just wanted to say-this post saved me. I was about to try cold turkey tomorrow. Now I’m calling my doctor. No shame in that. I’m not weak. I’m smart.
And if you’re reading this and you’re scared? You’re not alone. I was too. But I’m 14 days in on Suboxone. Still tired. Still emotional. But I’m here. And that’s enough.
❤️
bobby chandra
10 December 2025 - 04:00 AM
Let me tell you something no one else will: the real epidemic isn’t opioids. It’s loneliness. People don’t use because they’re weak. They use because they’re starving for connection. The drug is just the only thing that made them feel seen.
That’s why rehab fails. It’s not about the pills. It’s about the silence after. No one calls. No one visits. No one remembers your name.
So yeah-meds help. Therapy helps. But what really works? Someone showing up with a pizza at 2 a.m. and saying, ‘I’m not here to fix you. I’m here because you matter.’
That’s recovery. Not clinics. Not scales. Not protocols. Just presence.
Archie singh
11 December 2025 - 16:17 PM
PAWS is a scam. A pharmaceutical marketing ploy. There’s no such thing as ‘prolonged withdrawal’-it’s just ongoing addiction disguised as a syndrome. You don’t have a disease. You have a habit. And habits are broken with discipline, not pharmaceutical crutches.
And why is Suboxone promoted like a miracle? It’s still an opioid. You’re still dependent. You’re just not high. Big deal.
Real men don’t need medication to quit. They grit their teeth. They sweat it out. They suffer. And then they get back to work.
This whole article is a surrender narrative. And I won’t celebrate surrender.
Gene Linetsky
11 December 2025 - 23:33 PM
Did you know the FDA approved buprenorphine because Big Pharma wanted to lock people into lifelong prescriptions? Same with methadone. They don’t want you cured. They want you addicted to the cure.
And the ‘SAMHSA helpline’? It’s a government front. They track your data. They report you to your employer if you’re on a federal contract. They’re not helping you-they’re controlling you.
And why is there no mention of the real solution? Ketamine therapy. Psychedelics. The FDA is suppressing them because they can’t patent them. This whole system is rigged. You’re being sold a lie.
Go to Thailand. Get ibogaine. It’s legal there. One dose. One reset. No more cravings. No more meds. No more lies.
Albert Essel
13 December 2025 - 07:42 AM
Shalini’s point about India’s community-based models is vital-and underappreciated. The West often mistakes access for innovation. But in places with limited infrastructure, human connection becomes the primary therapeutic agent.
And to Archie: calling PAWS a ‘scam’ ignores decades of peer-reviewed neuroimaging studies showing persistent changes in dopamine receptor density and prefrontal cortex function long after last use.
Recovery isn’t binary. It’s not ‘you’re either cured or you’re weak.’ It’s a slow recalibration. And yes, medication helps. Not because it’s a crutch, but because it reduces the noise so the brain can heal.
Let’s stop fighting over semantics. Let’s start fighting for access.
Gavin Boyne
14 December 2025 - 12:40 PM
James-thank you. That’s the whole point. No one needs a lecture. They need someone to say, ‘I’m here.’
And to Gene: ibogaine isn’t a ‘real solution.’ It’s a cardiac risk with a 1 in 30 mortality rate in unmonitored settings. And yes, it’s illegal in the U.S. for a reason. You’re not a rebel. You’re reckless.
And to Archie: you’re not ‘real men.’ You’re just angry. And your anger is the reason people stay silent. Not because they’re weak. Because they’re afraid of you.