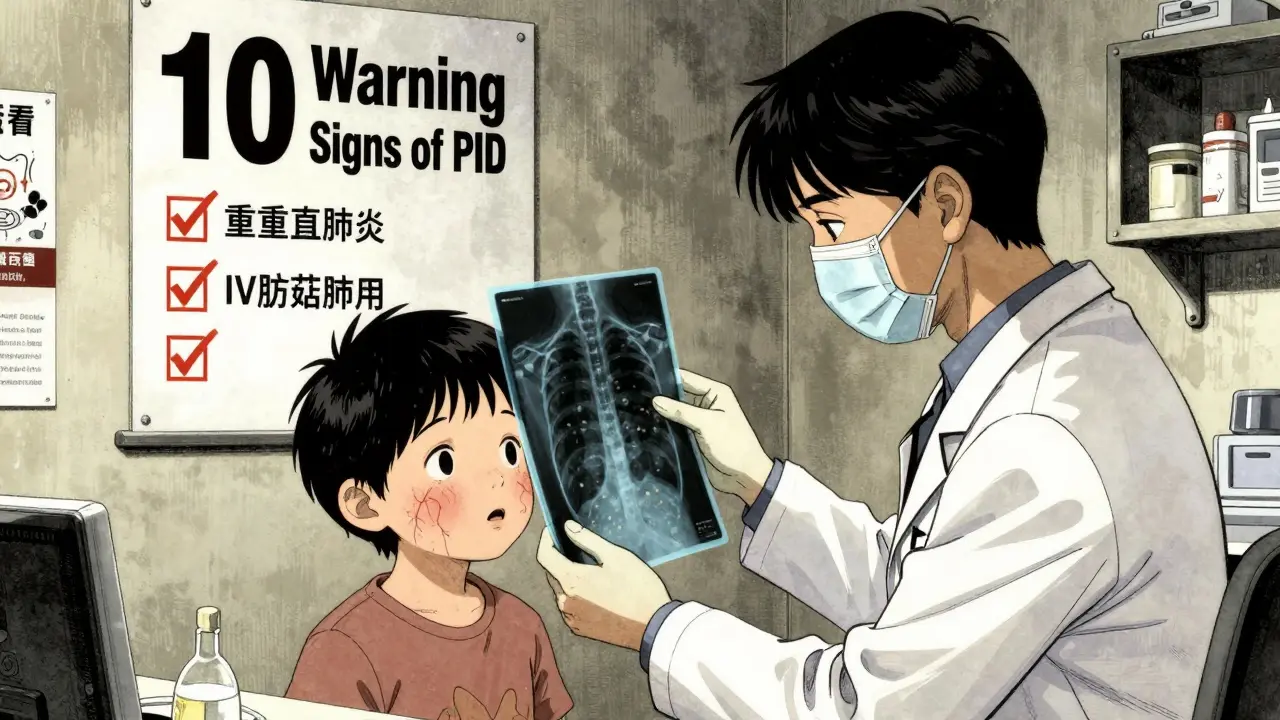
When your child keeps getting sick-ear infections, pneumonia, sinusitis-it’s easy to blame daycare, bad luck, or a weak immune system. But if the infections are too frequent, too severe, or don’t respond to standard treatment, it might not be luck at all. It could be a primary immunodeficiency (PID), a hidden condition where the immune system doesn’t work the way it should. The good news? Recognizing the red flags early can change everything. The bad news? Most doctors miss them. On average, it takes over nine years to diagnose a PID. That’s nine years of antibiotics, hospital visits, and sometimes permanent lung damage. Here’s what you need to know about the real signs that something deeper is going on-and what to ask your doctor next.
What Counts as "Too Many" Infections?
Every kid gets sick. A preschooler can have up to 12 colds a year. That’s normal. But when infections start crossing into dangerous territory, it’s time to look closer. The American Academy of Allergy, Asthma & Immunology (AAAAI) and the Immune Deficiency Foundation have laid out clear red flags. If your child or even an adult has:- Four or more ear infections in one year
- Two or more serious sinus infections in 12 months
- Two or more pneumonias in one year
- Deep skin abscesses or infections in organs like the liver or brain
- Oral thrush that lasts past age one
- Infections that don’t clear up after two months of antibiotics
- Need for IV antibiotics to treat routine infections
- Failure to gain weight or grow normally
- A family history of early deaths from infections
These aren’t just "concerning" signs-they’re diagnostic criteria. A 2017 study in the Journal of Allergy and Clinical Immunology found that kids diagnosed with severe combined immunodeficiency (SCID) before 3.5 months of age had a 94% survival rate. Those diagnosed later? Only 69%. That’s not a small difference. That’s life or death.
Physical Clues Beyond Infections
Infections aren’t the only clue. The body often leaves behind visible markers. A pediatrician examining a child with PID might notice:- Absent or very small tonsils and lymph nodes-this happens in nearly 80% of SCID cases
- Spider veins on the skin (telangiectasias), which are present in over 95% of children with ataxia-telangiectasia
- Chronic fungal infections in the mouth or skin that don’t respond to antifungal creams
- Weight and height below the 5th percentile, even if the child eats well
These aren’t random symptoms. They’re part of the fingerprint of specific immune disorders. For example, persistent oral thrush after age one has an 89% specificity for antibody deficiency. That means if a 4-year-old has thrush and no other explanation, there’s a very high chance their immune system isn’t making enough antibodies to fight fungi. That’s not normal. That’s a signal.
The Workup: What Tests Actually Matter
You can’t diagnose immunodeficiency with a guess. You need tests. But not all tests are equal. Many doctors order a basic CBC and call it a day. That’s not enough.The first step is a complete blood count (CBC) with manual differential. In children over one year, a lymphocyte count under 1,500 cells/μL is a red flag. In infants under one, it’s under 3,000. That tells you if the body is even making enough immune cells.
Next, quantitative immunoglobulins: IgG, IgA, IgM. But here’s the catch-normal levels change with age. A 3-month-old’s IgG level of 243 mg/dL is normal. An 8-year-old with the same number? That’s dangerously low. The average adult level is 700-1,600 mg/dL. If a child’s IgG is 420 mg/dL, some doctors might say "it’s fine" because it’s above 400. But for an 8-year-old? That’s below the 1st percentile. This mistake is why 41% of pediatricians in a 2021 survey started unnecessary IVIG therapy on kids who just had transient hypogammaglobulinemia of infancy-a harmless, temporary condition that fixes itself.
Then comes the real test: functional antibody response. You can’t just measure numbers-you have to see if the immune system can respond. This means giving a vaccine and checking antibody levels 4-6 weeks later. For tetanus and diphtheria, a protective level is 0.1 IU/mL. For pneumococcal vaccines, it’s 1.3 μg/mL. If the body doesn’t make enough antibodies after the shot, you have a real antibody deficiency. This is the gold standard. Without it, you’re guessing.
What’s Not Immunodeficiency? (The Misdiagnosis Trap)
Not every recurrent infection is immune-related. In fact, up to 43% of kids with frequent infections have anatomical problems. Cystic fibrosis causes thick mucus that traps bacteria. Chronic sinusitis from a deviated septum or nasal polyps creates the same pattern as immune failure. A foreign object stuck in a child’s airway can cause repeated pneumonia. In 18% of cases, that’s the real culprit.And then there’s secondary causes. Up to 30% of patients diagnosed with Common Variable Immunodeficiency (CVID) actually have something else: autoimmune disease, cancer, or medication side effects. A 2020 study in Annals of Internal Medicine found that 22% of patients got IVIG therapy without proof of antibody failure. That’s not just wasteful-it’s risky. IVIG can cause headaches, kidney damage, and allergic reactions. Giving it to someone who doesn’t need it does more harm than good.
When to Push for More
If your child has multiple red flags, don’t accept "they’ll outgrow it" or "it’s just allergies." Ask for:- A CBC with differential
- Quantitative IgG, IgA, IgM (with age-adjusted reference ranges)
- Lymphocyte subset analysis (CD3, CD4, CD19, CD56)
- Pre- and post-vaccination antibody titers (tetanus, diphtheria, pneumococcus)
- Consider genetic testing if there’s a family history or unusual infection patterns
And if your doctor says, "We don’t have access to those tests," ask for a referral to an immunologist. The American Academy of Pediatrics says every child with recurrent, severe, or unusual infections deserves specialist evaluation. You don’t need to wait for a miracle. You just need to ask the right questions.
New Tools, Faster Answers
The field is changing fast. In 2023, the FDA approved a next-generation genetic panel called StrataID Immune that tests 484 immune-related genes. It finds the cause in 35% of suspected cases-twice as many as older methods. The NIH is now running a study to build AI tools that predict PID from routine lab results with 92% accuracy. In five years, whole exome sequencing may become the first test for kids with recurrent infections, cutting diagnosis time from years to weeks.But here’s the hard truth: 78% of low- and middle-income countries still can’t test for basic immunoglobulin levels. That’s why awareness matters. The Jeffrey Modell Foundation’s "10 Warning Signs" campaign has helped increase PID diagnoses by 37% since 2015. It’s not about fancy machines. It’s about knowing the signs.
What to Do Next
If you’re worried:- Write down every infection your child has had in the last year-type, duration, treatment, response
- Check growth charts: are they falling below the 5th percentile?
- Look for physical signs: thrush after age one, absent tonsils, skin changes
- Ask your doctor: "Could this be a primary immunodeficiency? Can we check immunoglobulins and vaccine response?"
- If the answer is no, ask for a referral to an immunologist. Don’t wait for a crisis.
Early diagnosis doesn’t just prevent death. It prevents lung damage, hearing loss from chronic ear infections, and years of missed school and work. It turns a slow, painful journey into a clear path forward. You don’t need to be a doctor to spot the signs. You just need to pay attention.
What’s the difference between a common cold and a sign of immunodeficiency?
A common cold lasts 7-10 days, responds to rest and fluids, and doesn’t lead to complications like pneumonia or abscesses. In immunodeficiency, infections are more severe, last longer than two weeks, don’t respond to standard antibiotics, or recur frequently-especially if they involve the lungs, sinuses, or deep tissues. The key is pattern: multiple serious infections in a short time aren’t normal.
Can adults have primary immunodeficiency too?
Yes. Many people aren’t diagnosed until adulthood. Common Variable Immunodeficiency (CVID) often appears between ages 20 and 50. Symptoms include chronic sinusitis, pneumonia, diarrhea, and autoimmune conditions like lupus or rheumatoid arthritis. If you’ve had repeated infections throughout your life and no clear cause, it’s worth asking an immunologist.
Is IVIG therapy always needed for immunodeficiency?
No. IVIG is only recommended if there’s documented antibody deficiency and poor response to vaccines. Many people with low IgG levels don’t need it if they aren’t getting serious infections. Giving IVIG without proof of functional failure can cause side effects and is often unnecessary. Always confirm with vaccine response testing before starting treatment.
Why do some kids have low IgG but never get sick?
Some children have transient hypogammaglobulinemia of infancy-a temporary dip in IgG that resolves by age 2-3. If they aren’t having severe or recurrent infections, they don’t need treatment. The problem arises when doctors treat low numbers without considering clinical symptoms. Always look at the whole picture: infections, growth, physical signs-not just a lab value.
Can immunodeficiency be cured?
Some can. Severe Combined Immunodeficiency (SCID) can be cured with bone marrow transplant if caught early. Others, like CVID, can’t be cured but can be managed with immunoglobulin replacement, antibiotics, and monitoring. The goal isn’t always cure-it’s preventing damage so the person can live a full life.