Fall Risk Medication Checker
This tool helps identify medications that may increase your fall risk based on CDC guidelines. Enter your current medications to get personalized recommendations.
Your Results
Recommended Actions:
Important Note
This tool is for informational purposes only. Always consult your doctor or pharmacist before making changes to your medications.
Every year, about one in three adults over 65 falls. Many of these falls aren’t accidents-they’re side effects of medications. For older adults, a simple slip can mean a broken hip, a long hospital stay, or even death. And the truth is, most of these falls are linked to drugs that doctors prescribe without realizing how dangerous they can be for aging bodies.
Why Medications Turn Into Fall Triggers
As we age, our bodies process drugs differently. Liver and kidney function slow down. Muscle strength declines. Balance becomes more fragile. A medication that’s safe for a 40-year-old can be risky for a 75-year-old. The problem isn’t just one drug-it’s the combination. Nearly half of older adults take five or more prescriptions daily. That’s called polypharmacy, and it’s a major driver of falls.Many of these drugs don’t cause obvious side effects like nausea or rash. Instead, they quietly zap your balance, slow your reactions, or make you dizzy when you stand up. You might not even notice until you’re on the floor.
The Top 9 Medication Classes That Raise Fall Risk
Research from the American Geriatrics Society and the CDC has identified nine main drug classes that significantly increase fall risk in seniors. Here’s what you need to know about each:- Antidepressants - Both tricyclics (like amitriptyline) and SSRIs (like sertraline) can cause dizziness, low blood pressure, and slowed movement. Studies show they have the strongest link to falls among all drug classes. Even when taken as prescribed, they can make walking feel unstable.
- Benzodiazepines - Drugs like diazepam (Valium), lorazepam (Ativan), and alprazolam (Xanax) are often prescribed for anxiety or insomnia. But they cause deep sedation, memory fog, and poor coordination. Long-term use (beyond 2 weeks) doubles the risk of falling. The risk doesn’t go away the next day-you can still feel groggy.
- Sedative-Hypnotics - Sleep aids like zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata) are especially dangerous. They can cause sleepwalking, confusion, and sudden dizziness upon waking. One woman in Texas fell three times in two months after starting Ambien-her third fall broke her hip.
- Antipsychotics - Used for dementia-related agitation, drugs like haloperidol and risperidone can cause muscle stiffness, tremors, and sudden drops in blood pressure. First-generation antipsychotics are riskier than newer ones, but all carry significant danger.
- Opioids - Painkillers like oxycodone and hydrocodone cause drowsiness, dizziness, and confusion. The higher the dose, the higher the risk. High-dose opioids can increase fall risk by 80% compared to low-dose versions.
- Diuretics - Water pills like furosemide (Lasix) help with swelling and high blood pressure, but they can cause dehydration and sudden drops in blood pressure when standing. This is called orthostatic hypotension. One minute you’re fine; the next, you’re on the ground.
- Antihypertensives - Blood pressure meds like beta-blockers and ACE inhibitors are essential for heart health-but if the dose is too high, they can drop pressure too much when standing. Many seniors don’t realize their meds are making them lightheaded.
- NSAIDs - Common pain relievers like ibuprofen and naproxen can interfere with blood pressure control and cause fluid retention. They increase fall risk by about 25%, especially when taken daily.
- Anticholinergics - Found in many over-the-counter allergy and bladder meds (like diphenhydramine/Benadryl or oxybutynin), these drugs cause dry mouth, blurred vision, and mental confusion. Many seniors don’t know Benadryl is an anticholinergic-and that it’s one of the most common culprits behind unexplained falls.
Who’s Most at Risk?
It’s not just about the drugs-it’s about who’s taking them. Seniors with these factors are at highest risk:- Taking four or more medications daily
- Using more than one drug from the high-risk list above
- Already having balance problems or a history of falls
- Living alone or with limited support
- Using over-the-counter sleep aids or allergy meds regularly
Here’s a sobering stat: 65% to 93% of older adults who fall and get injured were taking at least one of these high-risk drugs at the time. And 63% had no idea their meds could cause falls.
What You Can Do: The STOP, SWITCH, REDUCE Plan
The CDC’s STEADI program gives a clear, practical approach: STOP unnecessary drugs, SWITCH to safer options, and REDUCE doses to the lowest effective level.STOP - Ask your doctor: “Is this drug still necessary?” Many seniors stay on medications long after they’re needed-like benzodiazepines prescribed for a short anxiety episode five years ago.
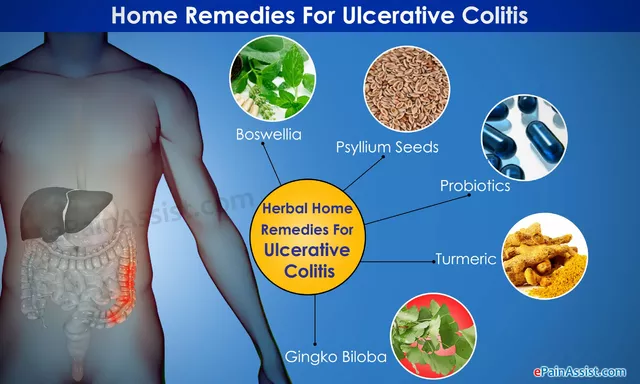
SWITCH - For insomnia, try cognitive behavioral therapy for insomnia (CBT-I). It’s as effective as sleep meds, without the fall risk. For anxiety, non-benzodiazepine options like buspirone may be safer. For overactive bladder, mirabegron has fewer cognitive side effects than oxybutynin.
REDUCE - Never stop a drug cold turkey. Work with your doctor to taper slowly. For benzodiazepines, a 10% dose reduction every 2-4 weeks is common. It takes 8-12 weeks to safely withdraw, but the payoff is better balance and fewer falls.
How to Have the Conversation With Your Doctor
Most seniors don’t bring up medication side effects unless asked. Here’s how to start the conversation:- Bring your “brown bag” to every appointment-every pill, supplement, and OTC drug you take.
- Ask: “Could any of these be making me dizzy or unsteady?”
- Say: “I’ve noticed I’m more unsteady lately. Could this be related to my meds?”
- Request a medication review at least once a year. Ask if your pharmacist can help.
Pharmacists are trained to spot dangerous combinations. A CDC study found that pharmacist-led reviews cut fall risk by 22%. They can flag hidden anticholinergics in allergy meds or warn about mixing NSAIDs with blood pressure drugs.

What’s Changing in 2025
Things are shifting. Medicare now tracks inappropriate prescribing in seniors and may reduce payments to doctors with high rates of fall-risk drug use. The American Geriatrics Society just updated its Beers Criteria in early 2024 to include newer drugs and their fall risk profiles. And AI tools are now being tested in clinics to scan medication lists and flag dangerous combinations with 89% accuracy.More importantly, research is proving that deprescribing works. A 2024 study found that when seniors safely stopped one or two high-risk drugs, their fall rate dropped by nearly 30% within six months. That’s not just saving money-it’s saving independence.
Real Stories, Real Consequences
One 72-year-old man in Ohio had been taking Xanax for anxiety for six years. He didn’t think it was a problem-until he fell down his basement stairs and fractured his spine. He didn’t realize the dizziness he felt every morning was from the drug. After stopping it under medical supervision, his balance improved in weeks.Another woman in Florida started taking Benadryl for allergies every night. She didn’t know it was an anticholinergic. She began forgetting where she put her keys, then started stumbling. After switching to a non-drowsy antihistamine, her falls stopped.
These aren’t rare cases. The CDC says 28% of older adults who fall blame their meds. But only 15% ever told their doctor.
What You Should Do Right Now
1. Take inventory. Gather every pill, patch, capsule, and supplement you take. Include OTC meds and herbal products. 2. Ask your doctor. “Which of these could be making me unsteady?” 3. Ask your pharmacist. Schedule a free medication review. Most pharmacies offer this. 4. Track your balance. If you’ve fallen once, you’re at high risk for another. Talk to your doctor about physical therapy or balance training. 5. Don’t wait. If you feel dizzy, foggy, or unsteady after starting a new drug, don’t assume it’s normal. Call your provider.Falls aren’t inevitable. They’re often preventable. The right conversation with your doctor can mean the difference between staying independent and losing your freedom. Your meds are meant to help you live better-not to put you at risk.

Saketh Sai Rachapudi
7 December 2025 - 02:58 AM
India has 150 million elderly and zero proper geriatric care-yet we’re still prescribing Xanax like candy. Who’s to blame? The doctors? The pharma reps? Or just our collective denial that aging isn’t a disease to be medicated away? This post is right-our elders are falling because we treat them like broken machines instead of human beings with dignity.
Nigel ntini
8 December 2025 - 19:16 PM
Brilliant breakdown. I’ve seen this first-hand with my dad-he was on 7 meds, including Benadryl for ‘allergies’ and Ambien for sleep. We cut two, switched one to CBT-I, and within weeks he stopped stumbling in the hallway. It’s not about removing meds-it’s about restoring function. Thank you for sharing this.
Kay Jolie
10 December 2025 - 03:37 AM
Oh. My. GOD. I just realized my 78-year-old aunt has been taking diphenhydramine EVERY NIGHT for 12 years. Like, literally. She calls it her ‘nightly reset.’ And now she’s forgetting her own birthday. This is a public health catastrophe wrapped in a 10mg capsule. We need a national campaign. Like, ‘Don’t Be a Benadryl Zombie.’
Max Manoles
10 December 2025 - 15:41 PM
My grandfather was on a beta-blocker and a diuretic. He’d get dizzy standing up, but he never said anything-he thought it was just ‘getting old.’ After his fall, his cardiologist did a full med review and stopped the diuretic. He’s been walking without a cane for 18 months now. It’s not always about adding drugs-it’s about removing the ones that steal your balance.
Myles White
11 December 2025 - 07:44 AM
It’s fascinating how polypharmacy is the silent epidemic nobody talks about until someone ends up in the ER with a hip fracture. The real issue isn’t just the drugs themselves-it’s the lack of coordination between specialists. Cardiologist adds a beta-blocker, neurologist prescribes an SSRI, psychiatrist throws in a benzodiazepine, and the primary care physician is left holding the bag with a 78-year-old who can’t stand up without grabbing the wall. We need a single point of accountability-like a geriatric pharmacist embedded in every Medicare clinic-and we need it yesterday. The data is clear: deprescribing reduces falls, hospitalizations, and mortality. So why are we still treating elderly patients like a pharmacological buffet?
Brooke Evers
13 December 2025 - 01:18 AM
I’m a nurse who works in geriatrics, and I can tell you-this is happening every single day. Families come in panicked because Grandma fell, but they don’t realize the new sleep aid she started last month is the culprit. And the worst part? The doctor says, ‘It’s fine, she’s just getting older.’ No. She’s getting poisoned by outdated prescribing habits. I’ve had patients cry because they lost their independence because no one asked if their meds were helping-or hurting. Please, if you’re reading this and you have an older loved one-go through their pill bottles with them. Ask the questions. Be their advocate. It could save their life.
joanne humphreys
14 December 2025 - 01:24 AM
I’m 64 and take three prescriptions. I’ve never thought about whether any of them could make me unsteady. I’ve had a few close calls on the stairs, but I assumed it was the rug. Maybe I should bring my brown bag to my next appointment. I didn’t even know pharmacists could review meds for free. That’s actually kind of amazing.
Mansi Bansal
15 December 2025 - 12:55 PM
It is with profound consternation and clinical alarm that I must assert, with the utmost formality, that the pharmacological mismanagement of geriatric populations constitutes a systemic dereliction of ethical duty by the modern medical-industrial complex. The normalization of anticholinergic burden, the casual prescription of sedative-hypnotics, and the pathological overreliance on polypharmacy as a panacea for age-related decline are not merely medical errors-they are sociocultural failures of epic proportion. One must ask: Is this medicine-or custodial chemical restraint?
Shayne Smith
16 December 2025 - 22:08 PM
My grandma took Benadryl for years. She’d zone out during dinner, forget her glasses, then say, ‘Oh, I’m just tired.’ Then she fell in the shower. We switched her to Claritin and she’s been her old self again. So simple. So overlooked.
Clare Fox
18 December 2025 - 07:52 AM
we’re all just trying to sleep, you know? and if a little white pill helps you not scream into the night… who are we to say no? but then you wake up and your legs don’t work right and you don’t remember why you walked to the kitchen… and suddenly you’re on the floor. it’s not the medicine’s fault. it’s the silence around it.
Akash Takyar
18 December 2025 - 21:08 PM
Dear Readers: I commend the author for this timely, meticulously researched exposition on the perilous nexus between polypharmacy and geriatric falls. It is imperative that we, as a society, institutionalize annual medication reconciliation protocols under the supervision of certified geriatric pharmacists. Furthermore, I urge all caregivers to engage in proactive, compassionate dialogue with healthcare providers, and to document all pharmaceutical intake with scrupulous accuracy. Let us not permit negligence to become the norm in elder care. Thank you for your diligence.