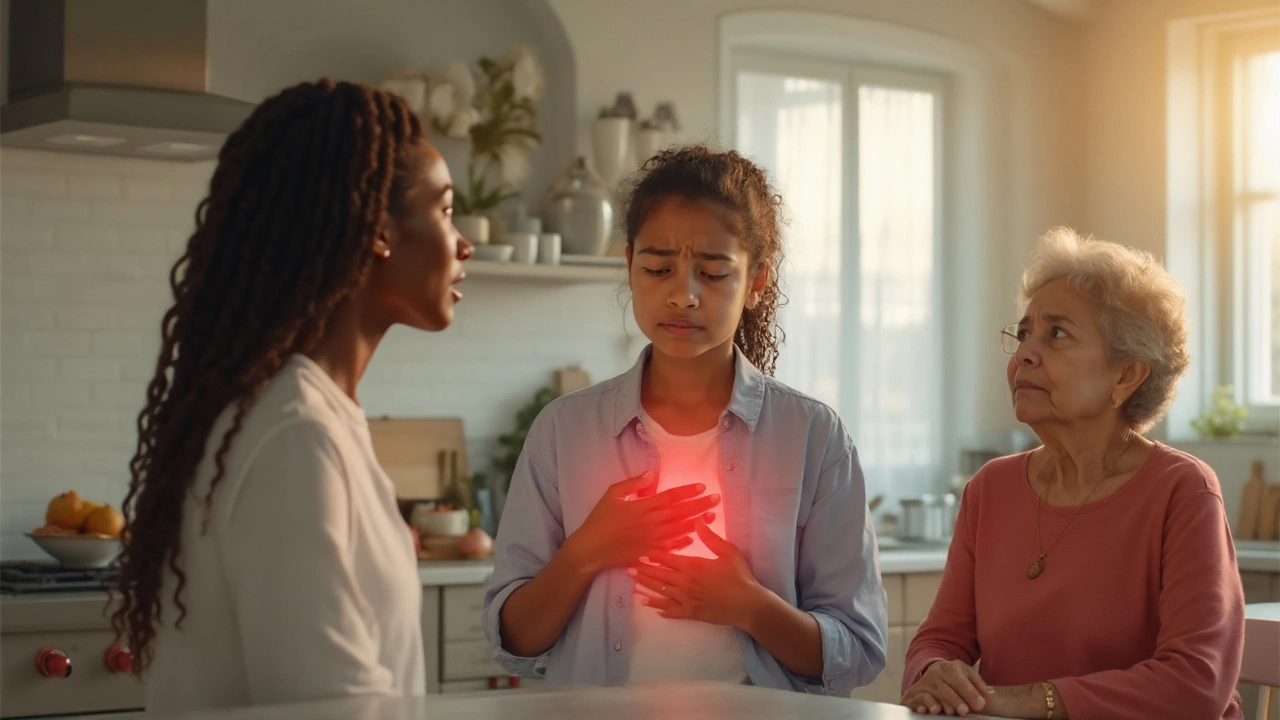
Chest Pain in Women is a clinical presentation where females experience discomfort, pressure, or pain in the chest area caused by a range of cardiac and non‑cardiac conditions. Unlike typical male patterns, women often report radiating pain to the back, jaw, or shoulder blades, and may describe symptoms as indigestion, fatigue, or shortness of breath. Recognizing these nuances saves lives, because studies show women are 30% more likely to delay seeking care for heart‑related chest pain.
Why Women Experience Different Chest Pain Patterns
Hormonal fluctuations, smaller coronary vessels, and higher prevalence of microvascular disease all reshape how pain feels. Estrogen influences the lining of blood vessels, making them more prone to spasm during menopause. At the same time, the Microvascular Angina affects the tiny arteries that supply the heart muscle, often without visible blockages on standard angiograms. Because these vessels are less than 200 microns, classic "clogged artery" pain is rare, leading to subtle, diffuse symptoms.
Common Cardiac Causes Unique to Women
- Myocardial Infarction (heart attack) in women frequently presents as pressure, nausea, or sudden weakness rather than crushing chest pain
- Microvascular Angina (see above)
- Coronary Artery Spasm temporary narrowing of a coronary artery that can trigger transient chest discomfort
- Pulmonary Embolism blockage in a lung artery that often causes sharp chest pain, rapid breathing, and faintness, especially in postpartum women
Non‑Cardiac Sources Frequently Mistaken for Heart Issues
Only about half of chest pain in women is heart‑related. The other half stems from gastrointestinal, musculoskeletal, or psychological origins.
- Gastroesophageal Reflux Disease (GERD) acid reflux that mimics heart pain, often worsening after meals or when lying flat
- Esophageal Spasm irregular contractions of the esophagus that cause choking‑like chest pressure
- Costochondritis inflammation of rib‑stomach cartilage that produces localized, reproducible pain when pressing on the chest wall
- Panic Attack sudden surge of anxiety that can generate tightness, rapid heartbeat, and a feeling of impending doom
Key Points to Spot Dangerous Chest Pain
- Sudden, unexplained shortness of breath or fainting
- Chest pressure accompanied by jaw, back, or arm pain
- Nausea, cold sweats, or severe fatigue without a clear cause
- Symptoms that appear during physical exertion, emotional stress, or after a heavy meal
Comparison Table: Typical Male vs Female Chest Pain Presentation
| Feature | Men | Women |
|---|---|---|
| Dominant sensation | Heavy pressure or crushing pain | Pressure, squeezing, or vague discomfort |
| Radiation | Left arm, jaw, neck | Back, upper abdomen, shoulder blades |
| Associated symptoms | Sweating, nausea | Nausea, indigestion‑like feeling, fatigue |
| Typical triggers | Physical exertion | Emotional stress, hormonal changes |
| Delay in seeking care | ~2 hours avg. | ~4 hours avg. |

Diagnostic Approach Tailored for Women
When a woman reports chest discomfort, clinicians should follow a stepwise algorithm that respects the higher likelihood of atypical presentations.
- Immediate ECG and cardiac enzymes to rule out acute myocardial infarction.
- If ECG is normal but suspicion remains, order a coronary CT angiography to detect microvascular disease. \n
- Consider esophageal pH monitoring or endoscopy when GERD or esophageal spasm is suspected.
- Use D‑dimer testing and CT pulmonary angiography if pulmonary embolism is a concern, especially postpartum.
- Evaluate mental health history; a validated anxiety screen can uncover panic‑related chest pain.
Management Strategies for Common Causes
Treatment must address both the root cause and the gender‑specific risk profile.
- Heart‑related pain: Low‑dose aspirin, statins, and beta‑blockers are standard, but women benefit from higher awareness of side‑effects like fatigue. For microvascular angina, nitrates and calcium‑channel blockers provide relief.
- GERD: Lifestyle changes (elevated head of bed, avoiding late meals) plus a proton‑pump inhibitor. Women often report that symptom relief improves overall chest discomfort.
- Panic attacks: Cognitive‑behavioral therapy combined with short‑acting benzodiazepines for acute episodes; SSRIs for long‑term control.
- Pulmonary embolism: Anticoagulation with low‑molecular‑weight heparin, transitioning to oral anticoagulants. Post‑partum women require careful dosing.
Related Topics to Explore
Understanding chest pain in women opens doors to broader health conversations. Readers may also want to learn about:
- Hormonal impact on cardiovascular health
- Women‑specific risk assessment tools (e.g., the Reynolds Risk Score)
- Lifestyle modifications that reduce heart disease risk in females
- How pregnancy and menopause reshape heart health
Next Steps for Readers
If you’ve experienced any of the red‑flag symptoms listed above, call emergency services right away. For recurring, non‑emergent discomfort, schedule a primary‑care or cardiology visit and bring this guide to discuss potential tests. Keep a symptom diary noting time, activity, and associated feelings - it helps clinicians pinpoint patterns unique to your body.
Frequently Asked Questions
Why do women often feel chest pain as indigestion?
Hormonal shifts can cause the esophagus to become hypersensitive, and the smaller coronary vessels may not generate the classic crushing pain. As a result, many women describe the sensation as heartburn or an upset stomach.
Can a normal ECG rule out a heart attack in women?
Not always. Women can have a heart attack with a non‑diagnostic ECG, especially when microvascular disease is involved. Blood tests for cardiac enzymes and advanced imaging are essential if suspicion remains high.
What lifestyle changes reduce the risk of atypical chest pain?
Regular aerobic exercise, a Mediterranean‑style diet, stress‑management techniques (yoga, mindfulness), and maintaining a healthy weight are proven to lower both traditional and microvascular heart disease risk in women.
Is chest pain during pregnancy a sign of a heart problem?
Pregnancy increases blood volume and clotting risk, so shortness of breath or sharp chest pain should be evaluated promptly. While many cases are musculoskeletal, conditions like pulmonary embolism are more common in late pregnancy and require urgent care.
How does menopause affect chest pain symptoms?
Declining estrogen leads to stiffening of arterial walls and increased likelihood of coronary spasm. Women often notice new onset of pressure‑type chest pain or fatigue during menopause, even without classic risk factors.




Jennifer Pavlik
23 September 2025 - 06:00 AM
Thanks for sharing this info-it's easy to overlook how different chest pain can feel for women. Keeping a symptom diary, as you suggested, really helps doctors spot patterns that might otherwise be missed. Also, remember that even mild‑looking symptoms like indigestion could signal something more serious. If you notice any sudden shortness of breath or fainting, treat it like an emergency. Stay proactive and encourage other women to get checked early.
Jacob Miller
23 September 2025 - 07:00 AM
Sure, because everyone just ignores their own symptoms.
Anshul Gandhi
23 September 2025 - 08:00 AM
Let me break this down for everyone who thinks the medical establishment is being completely transparent. First, the whole idea that "microvascular disease" is a new discovery is a classic re‑branding of old data that never made it to the headlines. Second, you’re told to get a CT scan, but who’s paying for that? Insurance companies love to hide the cost behind vague “pre‑authorization.” Third, the emphasis on "hormonal fluctuations" is a convenient way to blame women’s bodies rather than look at environmental toxins hidden in our food supply. Fourth, the pharma industry pushes aspirin and statins as the frontline without disclosing the massive side‑effects data they keep in secret. Fifth, when you read about “advanced imaging,” remember that many of those machines are funded by the same corporations that profit from the diagnoses they claim to detect. Sixth, the article mentions anxiety and panic attacks-classic mind‑body shortcuts that shift blame away from systemic health neglect. Seventh, the recommendation to monitor cardiac enzymes assumes you have immediate lab access, which many rural clinics lack. Eighth, D‑dimer tests are often over‑used to flag possible clots, leading to unnecessary anticoagulation and even bleeding. Ninth, the suggested lifestyle changes, like “Mediterranean diet,” ignore that processed foods infiltrate even the healthiest menu options. Tenth, stress‑management techniques such as yoga are great, but they’re sold as a cure‑all while the real stressors-job insecurity, healthcare costs-remain untouched. Eleventh, the “symptom diary” can be a useful tool, but it also becomes a data point for big‑data companies that mine health trends for profit. Twelfth, the article’s tone is reassuring, which is fine, but it downplays the urgency of seeking second opinions when tests come back “normal.” Thirteenth, the claim that women are "30% more likely to delay seeking care" is based on outdated surveys that didn’t account for tele‑medicine uptake. Fourteenth, the reassurance that a normal ECG doesn't rule out a heart attack is true, but it also subtly encourages reliance on expensive follow‑up tests. Fifteenth, let’s not forget that postpartum pulmonary embolism is a real threat, yet many hospitals lack specific protocols for it. Finally, the whole narrative fits the classic pattern: present a problem, offer a commercial solution, and leave you with a checklist that looks like a subscription form. Stay skeptical and do your own research.
Emily Wang
23 September 2025 - 09:00 AM
Great points! This information can actually empower women to listen to their bodies and act fast. Remember, staying active, eating whole foods, and managing stress aren’t just buzzwords-they truly lower risk. If something feels off, trust that gut feeling and get checked out. Keep sharing these resources so more people can benefit.
Hayden Kuhtze
23 September 2025 - 10:00 AM
Oh sure, because a simple symptom diary magically fixes everything.