Heatwaves Don’t Just Make You Sweat-They Can Kill You Faster If You Use Drugs
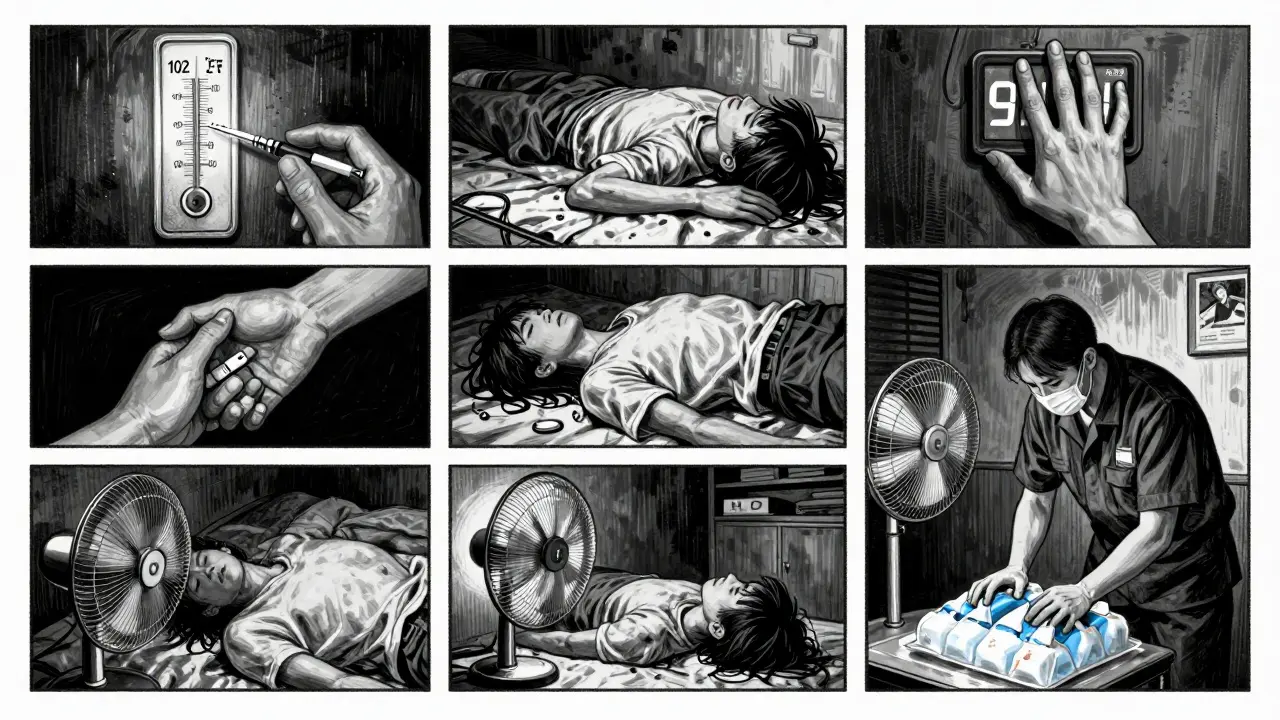
When the temperature hits 90°F and stays there for days, most people think about drinking more water, staying indoors, and turning up the AC. But for someone using drugs-especially stimulants like cocaine or meth, or opioids like heroin or fentanyl-heat isn’t just uncomfortable. It’s deadly. Studies show overdose deaths spike during heatwaves, and not because people are using more. It’s because their bodies can’t handle the combo of heat and drugs anymore.
In New York City, researchers found that when temperatures climbed above 75°F, accidental overdose deaths rose sharply. That’s not a coincidence. Heat forces your heart to work harder. Drugs like cocaine already push your heart rate up by 30-50%. Add heat, and you’re doubling the strain. Your body starts to shut down before you even realize something’s wrong.
Why Heat Makes Drugs More Dangerous
It’s not just about feeling hotter. Your body changes in ways you can’t see. When you’re dehydrated-even just 2% of your body weight in fluid loss-your blood gets thicker. That means drugs stay concentrated in your system longer. A normal dose can suddenly feel like double. A pill you’ve taken safely before? Now it could stop your breathing.
For opioid users, heat reduces your body’s ability to compensate for slowed breathing. Normally, when your oxygen drops, your brain tells you to breathe faster. Heat weakens that signal by 12-18%. That tiny margin between safety and overdose? Gone.
Stimulants like cocaine and meth make things worse. They raise your core body temperature. Heat does the same. When they meet, your body can’t cool itself. You start overheating, your heart races, your blood pressure spikes-and you collapse. Many people don’t even make it to the hospital.
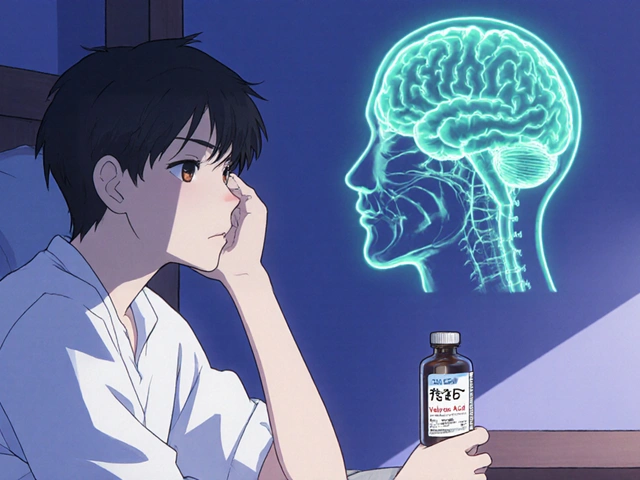
Even medications for mental health can play a role. About 70% of antipsychotics and 45% of antidepressants lose effectiveness or cause worse side effects in high heat. If you’re on one of these and using drugs, your risk isn’t just higher-it’s layered.
Who’s Most at Risk?
It’s not just people who use drugs. It’s people who use drugs and have nowhere to cool down. Over half a million Americans are homeless on any given night. Nearly 40% of them have a substance use disorder. They don’t have AC. They don’t have fans. They might be sleeping on concrete that radiates heat all night.
People in cities are hit harder than those in rural areas. Urban heat islands-areas where pavement, buildings, and cars trap heat-can be 3-5°F hotter than nearby neighborhoods. That’s enough to push someone over the edge.
And it’s not just the homeless. People in apartments without air conditioning, people who work outdoors, people recovering from illness, people on multiple medications-they’re all at higher risk. Heat doesn’t care if you’re ‘clean’ or ‘active.’ It only cares if your body can handle the stress.

What You Can Do Right Now
If you or someone you know uses drugs, here’s what actually works:
- Reduce your dose by 25-30% during heatwaves. Your body isn’t processing drugs the same way. What was safe last week could be lethal today.
- Hydrate constantly. Drink one cup (8 oz) of cool water every 20 minutes-even if you’re not thirsty. Don’t wait until you’re dizzy. Don’t rely on sports drinks-they’re loaded with sugar and sodium. Plain water is best.
- Avoid using alone. If you’re using, have someone nearby who knows how to use naloxone. If you’re using opioids, keep naloxone with you at all times. It’s free at most harm reduction centers.
- Find shade or air conditioning. Libraries, community centers, and public transit stations often have AC. Even sitting in a shaded park for 20 minutes can lower your risk.
- Don’t use drugs if you’re sick. Fever, infection, or even the flu makes your body less able to handle stress. Add drugs to that mix, and you’re playing Russian roulette with your life.
What Communities Are Doing That Works
Some places are getting smart about this. In Philadelphia, public health workers hand out cooling kits during heat alerts. Each one has electrolyte packets, misting towels, water bottles, and a card with overdose prevention info. Since they started in 2020, heat-related overdose calls dropped by 17%.
In Vancouver, they opened seven air-conditioned respite centers next to supervised injection sites. People could rest, drink water, get cooled down, and still access clean supplies and medical help. During the 2021 Pacific Northwest heat dome-when temperatures hit 121°F-those centers cut heat-related overdose deaths by 34%.
In Maricopa County, Arizona, volunteers trained in naloxone and heat safety knocked on doors of people who use drugs. They made over 12,000 wellness checks during one summer. They found people passed out in cars, in alleys, on rooftops. They saved 287 lives.
These aren’t miracles. They’re simple, low-cost, human-centered actions. And they work.
What’s Still Broken
Only 12 out of 50 U.S. states have official heat emergency plans that include people who use drugs. Most don’t even mention them. Shelters still turn people away if they’re using. Police sometimes confiscate water or cooling supplies from outreach workers.
And yet, the data is clear: people who use drugs are 18-22% of all heat-related ER visits during extreme weather. That’s not a small group. That’s a public health emergency.
The Biden administration just allocated $50 million to fix this. By December 2025, every state health department must include overdose risk in their heat action plans. That’s a start. But it won’t help anyone if it stays on paper.
What You Can Do Today
You don’t need to be a policymaker to save a life.
- If you know someone who uses drugs, ask them: ‘Are you staying cool?’
- Carry an extra bottle of water and give it to someone on the street.
- Learn where your local harm reduction center is. They give out naloxone, water, and advice for free.
- If you’re in a position to help-church, community group, workplace-push to open cooling spaces during heat alerts.
- Don’t assume someone’s ‘just being careless.’ Heat and drugs are a silent killer. Most people don’t realize how fast it happens.
When the heat rises, so does the risk. But so can our response. We don’t need more slogans. We need more water. More shade. More people who care enough to check in.
Frequently Asked Questions
Can drinking water really prevent an overdose during a heatwave?
Yes, but not alone. Drinking water helps prevent dehydration, which concentrates drugs in your blood and raises overdose risk. Staying hydrated lowers that risk significantly-studies show a 17% drop in heat-related overdose calls when hydration is part of outreach. But water doesn’t replace naloxone, reducing dose, or avoiding use in extreme heat. It’s one layer of protection.
Is it safe to use drugs if I’m only taking a small amount during a heatwave?
No. Even small amounts become dangerous in heat. Your body’s ability to process drugs drops as your core temperature rises. A dose you’ve taken safely before could now be lethal because your metabolism is slower, your blood is thicker, and your breathing is weaker. The rule of thumb: cut your dose by at least 25-30% during heatwaves. Better yet, delay use until temperatures drop.
Why do some people die from heat and drugs but others don’t?
It’s not luck. It’s about your body’s limits. People with heart conditions, diabetes, or who take medications like antipsychotics are at higher risk. So are people who are dehydrated, elderly, or homeless. Those who survive often had access to water, shade, or someone who noticed they were in trouble. The difference isn’t willpower-it’s support, environment, and timing.
Does naloxone work during heat-related overdoses?
Yes-if the overdose is from opioids. Naloxone reverses opioid overdoses regardless of heat. But if the person is overdosing from cocaine, meth, or a mix of drugs, naloxone won’t help. Heat can also cause non-opioid overdoses through heart failure or heatstroke. That’s why hydration, cooling, and calling 911 are just as important as having naloxone.
Are there places I can go to cool down if I’m using drugs and don’t have AC?
Yes. Many cities now have cooling centers open during heat advisories, and some are located next to harm reduction services. Libraries, community centers, malls, and public transit stations are often air-conditioned and open to everyone-even if you’re using drugs. In places like Vancouver and Philadelphia, these centers provide water, snacks, and medical help. Call your local health department or search for ‘cooling center near me’ during a heat warning.
What if I’m on medication for mental health and use drugs-am I at higher risk?
Yes. About 70% of antipsychotics and 45% of antidepressants become less effective or cause worse side effects in extreme heat. This can lead to increased drug use to feel normal, or sudden crashes when the meds stop working. If you’re on these meds and use drugs, talk to your provider before a heatwave. Adjustments may be needed. Never stop meds without medical advice.
What Comes Next
By 2050, the number of days above 75°F could increase by 20-30 per year. That means more heatwaves. More overdoses. More deaths-unless we act now.
This isn’t just about individual choices. It’s about systems failing people who are already struggling. Cooling centers aren’t luxury. Naloxone isn’t optional. Water isn’t a privilege. These are basic survival tools.
If you’re reading this, you’re already part of the solution. Share it. Talk to someone. Carry water. Know where the nearest harm reduction center is. You don’t need to fix everything. Just help one person stay alive today.




Sheila Garfield
29 January 2026 - 19:36 PM
Man, I never thought about how heat messes with drug metabolism like that. I’ve seen people pass out on the sidewalk in July and assumed they were just wasted. Turns out their bodies were literally shutting down. We need more cooling centers-like, immediately.
Shawn Peck
31 January 2026 - 16:47 PM
Stop coddling junkies. If you can’t handle the heat, don’t do drugs. Simple. No one’s forcing you to be a dumbass. You want to live? Stop being lazy and get a job with AC.
April Allen
2 February 2026 - 08:09 AM
The neurophysiological interplay here is profound. Hyperthermia induces vasoconstriction in peripheral vasculature while simultaneously increasing cardiac output-a perfect storm when combined with dopaminergic agonists like meth. The thermoregulatory feedback loop is suppressed by both exogenous substances and environmental stressors, effectively decoupling homeostatic control. Add to that reduced renal clearance due to dehydration, and you’ve got a pharmacokinetic cascade that turns therapeutic doses into lethal ones. This isn’t just harm reduction-it’s clinical epidemiology in real time.
And yet, public health infrastructure still treats this as a moral failure rather than a systems collapse. The data is unequivocal. We’re not talking about outliers. We’re talking about predictable, preventable mortality curves tied directly to ambient temperature thresholds.
Philadelphia’s cooling kits? Brilliant. Low-cost, high-yield. Why aren’t we scaling this nationally? Because we’d rather criminalize than care. Again.
Diana Dougan
2 February 2026 - 14:05 PM
lol so now we’re giving out water bottles to drug addicts like they’re toddlers? next they’ll hand out pacifiers and bedtime stories. if you’re dumb enough to use drugs in 90 degree heat, you deserve what you get. also, ‘naloxone is free’? yeah right, at the same place that gives out free glitter tattoos and vegan donuts.
Melissa Cogswell
4 February 2026 - 04:08 AM
I work at a harm reduction center in Chicago. We’ve been handing out cooling packs and electrolyte tabs since last summer. One guy came in last week, said he’d been sleeping on a fire escape for three nights straight. We gave him water, a fan, and a ride to a shelter. He cried. Didn’t use that day. Just sat there breathing. That’s the real win-not stats, not policy. One person staying alive.
Beth Cooper
5 February 2026 - 16:38 PM
Wait… so you’re telling me the government is giving out water and AC to drug users but not to ‘real’ Americans? Sounds like a deep state plot to normalize addiction. Also, did you know 70% of antipsychotics are laced with microchips? They’re tracking us through our meds. That’s why the heat ‘affects’ them more-because the chips overload in high temps. And don’t get me started on the 5G towers that make your blood thicker. It’s all connected.
Kathleen Riley
7 February 2026 - 15:16 PM
It is an incontrovertible empirical observation that the confluence of environmental hyperthermia and exogenous psychoactive pharmacological agents precipitates a profound dysregulation of autonomic homeostasis. One is compelled to interrogate the ethical imperative of societal infrastructure to mitigate such preventable morbidity, particularly in populations rendered vulnerable by structural disenfranchisement. The moral calculus, therefore, is not one of individual agency, but of collective responsibility.
Yanaton Whittaker
9 February 2026 - 08:29 AM
AMERICA IS WEAK. We’re giving out WATER to people who CHOOSE to destroy their lives? That’s not compassion, that’s surrender. We need more cops, not cooling centers. Build more prisons, not AC rooms. If you’re too weak to handle heat, go live in Canada. 🇺🇸🔥
P.S. Naloxone is for weaklings. Real men ride it out.
Holly Robin
10 February 2026 - 13:08 PM
Let me get this straight-people who use drugs are getting free water and AC, but my elderly neighbor has to pay $300 for her electric bill? And you wonder why people are angry? This isn’t public health-it’s reverse discrimination. The system is rigged. They’re rewarding bad behavior and punishing the hardworking. And don’t even get me started on how the CDC is hiding the truth about ‘heat-induced overdose’-it’s all a cover for vaccine side effects. You think this is about heat? It’s about control.
Sarah Blevins
10 February 2026 - 21:20 PM
While the empirical correlation between ambient temperature and overdose mortality is statistically significant (p < 0.01), the causal attribution remains confounded by socioeconomic variables, including housing instability, access to healthcare, and polypharmacy. The proposed interventions, while well-intentioned, lack a robust cost-benefit analysis and risk reinforcing dependency narratives. A more rigorous approach would involve longitudinal cohort studies before institutionalizing policy changes.
April Allen
12 February 2026 - 06:06 AM
Interesting. You’re right-correlation isn’t causation. But when 18-22% of heat-related ER visits are people who use drugs, and you’ve got a 34% drop in deaths when you add cooling centers next to injection sites? That’s not noise. That’s a controlled intervention with measurable outcomes. You want ‘rigorous’? Look at Vancouver’s data. It’s not theory. It’s lives saved. And yes, housing instability is a confounder. That’s why we need housing. Not just water. Not just naloxone. All of it.