Hepatitis C Alcohol Risk Calculator
Understand Your Alcohol Impact
This tool estimates how your alcohol consumption affects liver damage progression and treatment success rates for chronic hepatitis C.
When you hear about chronic hepatitis C, the first thing that often comes to mind is a virus that attacks the liver. Add alcohol to the mix, and the picture becomes a lot more complicated. This guide breaks down exactly how drinking changes the course of hepatitis C, what it means for treatment, and the steps you can take to protect your liver.
Quick Takeaways
- Alcohol accelerates liver damage in people with hepatitis C, leading to faster fibrosis and higher cirrhosis risk.
- Even moderate drinking can lower the success rate of modern direct‑acting antiviral (DAA) therapies.
- Complete abstinence offers the best chance for viral cure and long‑term liver health.
- Regular monitoring of liver enzymes and HCV viral load is essential if you continue to drink.
- Support programs for alcohol use disorder improve treatment adherence and outcomes.
What Is Chronic Hepatitis C?
Chronic Hepatitis C is a long‑lasting infection caused by the hepatitis C virus (HCV) that primarily targets the liver. If left untreated, the virus can cause inflammation, scarring (fibrosis), and eventually cirrhosis or liver cancer. Worldwide, about 71 million people live with chronic HCV, and many are unaware of their status until liver complications appear.
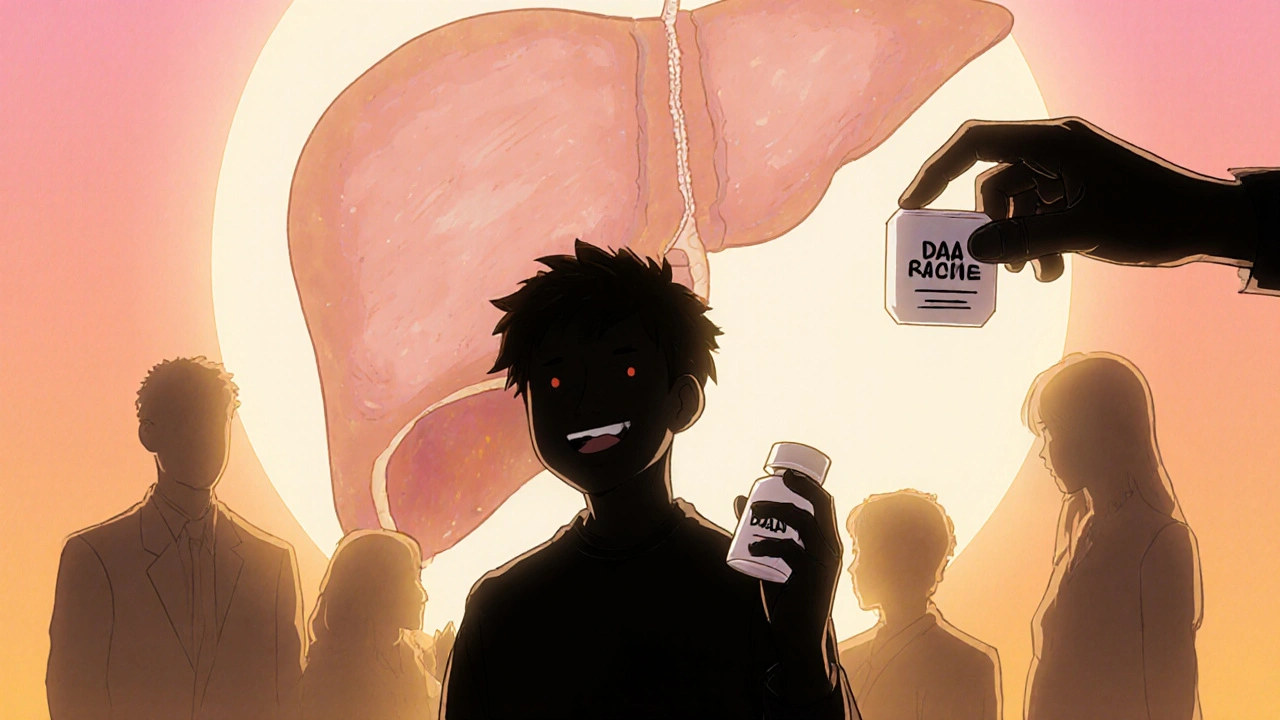
How Alcohol Affects the Liver
Alcohol is a toxin that the liver works hard to break down. When you drink, the liver converts ethanol into acetaldehyde, a highly reactive compound that damages liver cells and triggers inflammation. Repeated exposure leads to fatty liver, then to fibrosis, and finally to cirrhosis-a stage where healthy liver tissue is replaced by scar tissue.

The Interplay Between Hepatitis C and Alcohol
Both HCV and alcohol attack the same organ, but they do so in slightly different ways. When combined, the damage isn’t just additive-it’s synergistic.
- Increased inflammation: Alcohol magnifies the immune response already provoked by HCV, causing more liver cell death.
- Accelerated fibrosis: Studies show that patients who drink heavily develop advanced fibrosis up to three years sooner than abstainers.
- Higher risk of cirrhosis: Even moderate drinkers (2‑3 drinks per day) have a 2‑fold increase in cirrhosis risk compared with non‑drinkers.
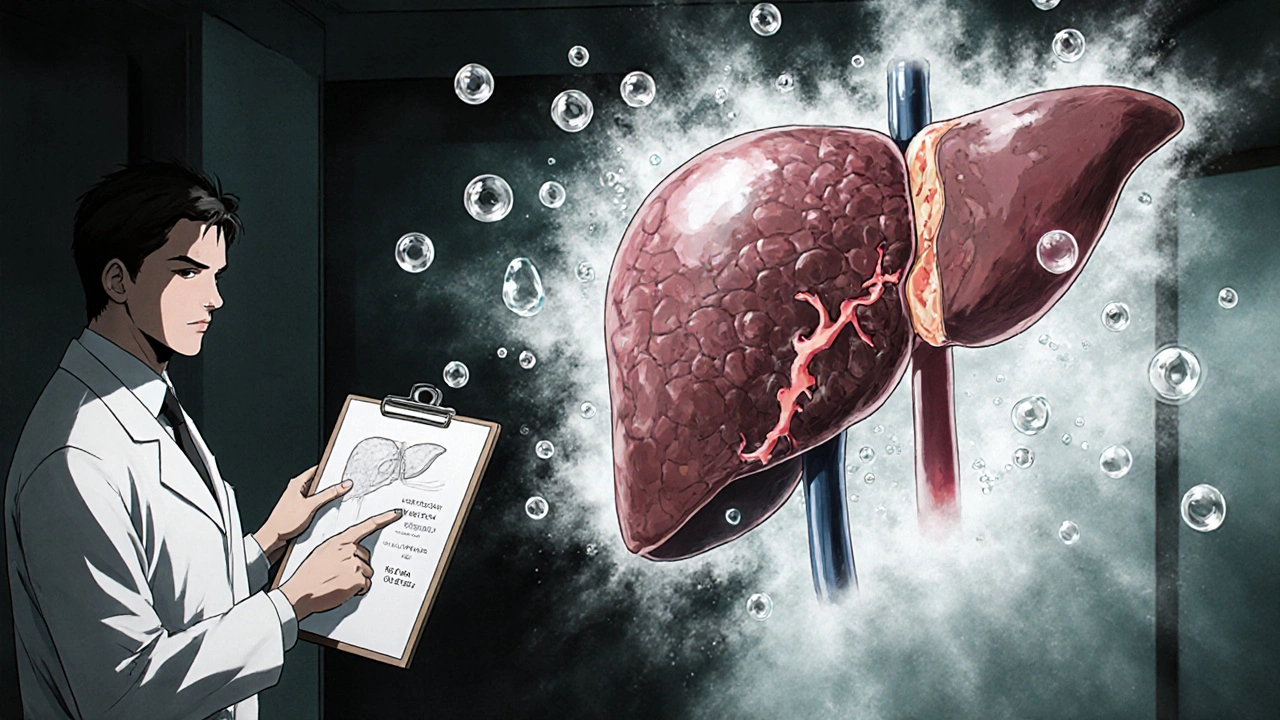
Impact on Disease Progression
Understanding the stages helps you see why alcohol matters.
- Liver fibrosis is the buildup of scar tissue that stiffens the liver. Alcohol speeds up this process, pushing patients from mild (F1) to severe (F3‑F4) stages faster.
- Cirrhosis marks irreversible scarring and loss of liver function. When HCV and alcohol coexist, the odds of reaching cirrhosis before age 50 double.
- Hepatocellular carcinoma (liver cancer) becomes more likely once cirrhosis is established. Alcohol‑related oxidative stress adds another cancer‑promoting pathway.
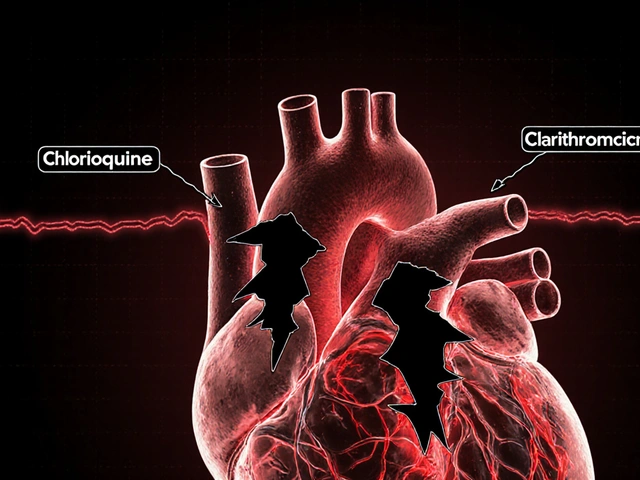
Effects on Treatment Success
Modern therapy for hepatitis C relies on direct‑acting antivirals (DAAs), which target specific steps in the viral life‑cycle. These drugs boast cure rates above 95 % in clinical trials, but real‑world success can dip when alcohol is in the picture.
- Adherence issues: Alcohol use disorder often leads to missed doses, undermining the 8‑week regimen.
- Reduced viral clearance: Heavy drinkers show a modest drop in sustained virologic response (SVR) rates, from 98 % to about 90 %.
- Liver function impact: Ongoing alcohol damage can keep liver enzymes elevated, making it harder for clinicians to gauge treatment response.
Regular HCV RNA test monitoring before, during, and after therapy is crucial to catch any setbacks early.
Practical Recommendations
- Aim for total abstinence: The safest route is to stop drinking completely. Even low‑level consumption can impede healing.
- Seek support for alcohol use disorder: Counseling, medication‑assisted therapy (e.g., naltrexone), and peer groups improve quit rates.
- Get regular liver assessments: FibroScan, ultrasound, and blood panels every 6‑12 months help track fibrosis progression.
- Stay on schedule with DAAs: Use pillboxes, phone reminders, or a caregiver’s help to keep doses consistent.
- Adopt a liver‑friendly lifestyle: Balanced diet, weight control, and avoiding other hepatotoxins (like high‑dose acetaminophen) support recovery.
Alcohol Consumption Levels vs. Expected Impact on HCV Progression
| Drinking Level | Weekly Units | Effect on Fibrosis | Effect on DAA Success |
|---|---|---|---|
| Abstinent | 0 | Baseline progression (slowest) | ≥ 98 % SVR |
| Moderate | 1-7 | 2‑fold increase in fibrosis rate | ~95 % SVR |
| Heavy | ≥ 8 | Accelerated to cirrhosis in 3‑5 years | ~90 % SVR, higher relapse risk |
Frequently Asked Questions
Can I cure hepatitis C if I keep drinking?
You can still achieve a cure, but the chance drops the more you drink. Heavy consumption can lower cure rates by up to 8 % and increase the risk of liver complications during treatment.
Is moderate drinking safe after I finish DAA therapy?
Even after viral clearance, any alcohol still stresses a liver that may already be scarred. Experts recommend staying alcohol‑free to prevent new damage, especially if fibrosis remains advanced.
What tests show if alcohol is hurting my liver?
Blood tests for ALT, AST, and GGT, plus imaging like FibroScan, reveal ongoing injury. Elevated GGT often signals alcohol‑related stress.
How quickly does fibrosis improve after I quit drinking?
If you stop alcohol and achieve a viral cure, mild fibrosis can regress over 2‑3 years. Advanced fibrosis may stabilize but rarely reverses completely.
Do I need a specialist to manage both HCV and alcohol use?
A hepatologist or liver‑focused infectious‑disease doctor can coordinate antiviral treatment, while a counselor or addiction specialist handles alcohol dependence. A collaborative approach yields the best outcomes.



Nhasala Joshi
18 October 2025 - 21:33 PM
Ever wonder why the big pharma lobby never talks about the deadly cocktail of HCV and booze? 🧐 They push glamorous DAA ads while silently counting how many lives they can burn out with accelerated fibrogenesis 🤯 Alcohol acts like a silent saboteur, cranking up ALT, AST and throwing the immune system into overdrive. The virus already manipulates cytokine pathways; add ethanol and you get a perfect storm of oxidative stress and collagen deposition. If you want a real cure, you’ve got to cut the liquor pipe before the hidden agenda finishes the job. 🍸🚫
Emma Williams
18 October 2025 - 21:35 PM
Totally agree we should all aim for zero drinks
Alex Lineses
18 October 2025 - 21:36 PM
First off, congratulations on taking the step to learn about the HCV‑alcohol interaction, that’s the kind of awareness that saves lives. The most important takeaway is that even moderate drinking can derail the impressive >95 % cure rates we see with DAAs. When you keep a drink in your system, the liver has to split its attention between detoxifying ethanol and supporting the antiviral pharmacokinetics. That split often translates into higher GGT levels, which can mask true treatment response and make dose‑adjustments trickier for the clinician. One practical strategy is to set up a daily pillbox and pair it with a phone alarm; missed doses are the single biggest predictor of reduced SVR. If you’re battling an alcohol use disorder, don’t try to go it alone-enroll in a medication‑assisted program like naltrexone or acamprosate, which can blunt cravings while you stay on your DAA schedule. Peer support groups, whether in‑person AA meetings or online forums, provide accountability and reduce the isolation that often fuels relapse. From a monitoring standpoint, schedule a FibroScan every six months; seeing your liver stiffness numbers improve can be a huge motivational boost. Blood work should include ALT, AST, and GGT panels before, during, and after therapy so you and your provider can spot any alcohol‑related spikes early. If you notice persistent elevation, discuss with your hepatologist whether a brief treatment pause or a supplemental antioxidant regimen might be warranted. Nutritionally, lean proteins, omega‑3 fatty acids, and a Mediterranean‑style diet can help the liver regenerate the extracellular matrix it lost to fibrosis. Avoid over‑the‑counter painkillers like high‑dose acetaminophen, because the added hepatic load can compound ethanol’s toxicity. Remember that the virus itself isn’t the only enemy; the inflammatory cascade triggered by drinking is what accelerates cirrhosis. In the long run, total abstinence gives you the best odds of not just clearing the virus but also halting any further scar tissue formation. Even if you’ve already reached advanced fibrosis, quitting alcohol can stabilize the disease and, in some cases, even allow modest regression over a few years. Bottom line: combine strict adherence to your DAA regimen with a solid, alcohol‑free lifestyle, and you’ll maximize the chance of a full, lasting cure.
kendra mukhia
18 October 2025 - 21:38 PM
Honestly Alex, your “one‑size‑fits‑all” pep talk glosses over the harsh reality that many patients can’t just snap their fingers and quit drinking. The socioeconomic pressures, mental health comorbidities, and sheer addiction physiology mean your neat checklist often falls flat. You sound like a textbook copy‑paste when real‑world adherence is riddled with setbacks. A more nuanced plan would acknowledge relapse risk and incorporate harm‑reduction steps, not just blind abstinence.
Bethany Torkelson
18 October 2025 - 21:40 PM
Stop sugar‑coating the struggle, Kendra. If patients want concrete tools, we give them medication‑assisted therapy, not just moralizing about “hard work”. The data doesn’t lie-targeted pharmacology plus counseling beats vague optimism every time.
Grace Hada
18 October 2025 - 21:41 PM
Spare us the lecture; the facts speak louder than your feel‑good nonsense.
alex montana
18 October 2025 - 21:43 PM
Wow!!! You think you can just ignore the liver‑toxicity!!! Alcohol + HCV = disaster!!! Stop pretending it’s a minor issue!!!
Wyatt Schwindt
18 October 2025 - 21:45 PM
I hear you, and it helps to keep monitoring liver enzymes while working on a realistic drinking plan.
Lyle Mills
18 October 2025 - 21:46 PM
From a hepatology perspective, the synergistic effect of ethanol metabolism and HCV replication accelerates collagen deposition, so cutting alcohol is a pharmacodynamic lever you can control.