What Is Cervical Myelopathy?
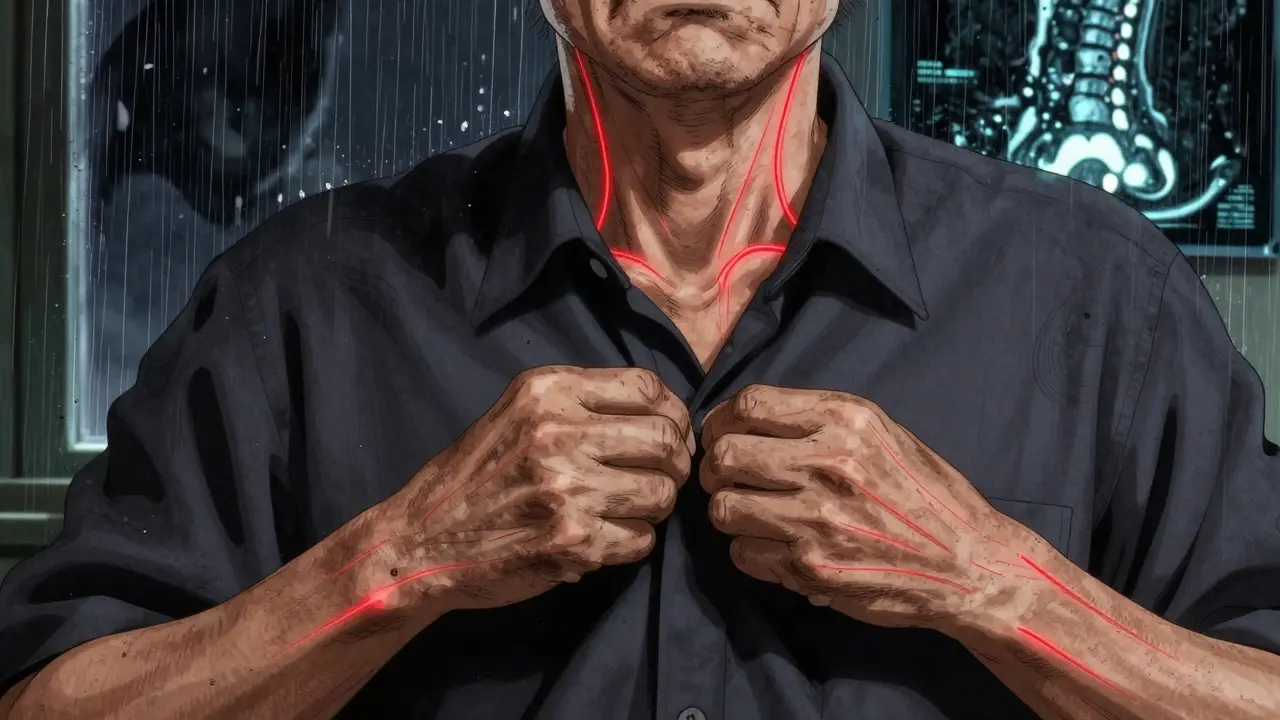
Cervical myelopathy is a condition where the spinal cord in your neck gets squeezed, leading to nerve damage. It’s not just a stiff neck or a pinched nerve-it’s actual harm to the spinal cord, usually caused by cervical spinal stenosis, which is the narrowing of the spinal canal in your neck. This narrowing happens slowly over time, often due to aging, arthritis, or disc degeneration. The most common form, called cervical spondylotic myelopathy (CSM), affects about 9% of people over 70 and makes up 75% of all cervical myelopathy cases.
Think of your spinal cord like a cable running through a narrow tunnel. When that tunnel shrinks-because of bone spurs, thickened ligaments, or bulging discs-it starts pressing on the cable. That pressure disrupts the signals traveling between your brain and body. Over time, this can cause permanent damage if left untreated.
What Are the Early Warning Signs?
The symptoms of cervical myelopathy don’t show up all at once. They creep in quietly, often mistaken for normal aging. The first red flag is usually hand clumsiness. You might drop things more often, struggle to button shirts, or find it hard to turn a key or open jars. This isn’t just weakness-it’s loss of fine motor control.
Another early sign is gait instability. You may feel unsteady walking, especially on uneven ground or stairs. Some people describe it as feeling like they’re walking on a boat. Balance problems, frequent stumbling, or needing to hold onto walls for support are common. These aren’t just "getting older"-they’re signs your spinal cord isn’t sending clear signals to your legs.
Other early symptoms include:
- Numbness or tingling in your hands or arms
- Increased reflexes in your knees and ankles (something a doctor checks with a reflex hammer)
- Weakness in your arms or legs
- Neck or arm pain (though not everyone has this)
As the condition progresses, you might notice trouble with bladder control-sudden urges to urinate or even incontinence. This is a serious red flag. If you’re experiencing any of these, especially in combination, you need to see a specialist. Delaying care can mean losing function you can’t get back.
How Is It Diagnosed?
Diagnosing cervical myelopathy isn’t just about feeling pain. Doctors look for a mix of symptoms and objective findings. The first step is a neurological exam. They’ll check your reflexes, muscle strength, coordination, and sensation in your arms and legs. Over 85% of patients show increased reflexes, and 72% report hand clumsiness during these exams.
But symptoms alone aren’t enough. You need imaging. MRI is the gold standard. It shows exactly where the spinal cord is being squeezed and whether there’s damage inside the cord itself-like swelling or scarring visible as bright spots on T2-weighted images. Without this signal change, you might have stenosis but not myelopathy. About 21% of people over 40 have stenosis without any symptoms, so the MRI must show both narrowing and cord injury to confirm the diagnosis.
Other tests might be used too:
- CT myelography-a CT scan with dye injected into the spinal fluid-used if MRI isn’t possible.
- EMG and SSEPs-nerve tests that detect subtle electrical problems before symptoms get worse.
- X-rays-they won’t show spinal cord damage, but they can reveal bone spurs, disc collapse, or instability that’s contributing to the problem.
The Japanese Orthopaedic Association (JOA) score is often used to measure severity. It rates motor function, sensation, and bladder control on a scale of 0 to 17. A score below 14 means myelopathy is present. This helps track progress and decide if surgery is needed.

When Is Surgery Necessary?
Not everyone with cervical myelopathy needs surgery-but if your symptoms are getting worse, you probably do. The North American Spine Society says that for mild cases (JOA score 12-14), doctors might try physical therapy and anti-inflammatory meds. But here’s the catch: only 28% of those patients improve over two years. The other 63% get worse.
Once your JOA score drops below 12, surgery becomes the standard recommendation. Why? Because the spinal cord doesn’t heal well once damaged. The longer you wait, the less likely you are to recover lost function. Studies show that patients who have surgery within six months of symptom onset recover 37% better than those who wait over a year.
Dr. Wellington Hsu at Northwestern puts it bluntly: "Recovery potential drops by about 3% per month of delay." That’s not a small number. Waiting a year could mean losing 36% of your recovery potential.
What Are the Surgery Options?
There’s no one-size-fits-all surgery. The best approach depends on how many levels are affected, your spinal alignment, and your overall health.
Anterior Approaches
These come from the front of the neck. The most common is anterior cervical discectomy and fusion (ACDF). The surgeon removes the damaged disc and bone spurs, then fuses the vertebrae with a bone graft and metal plate. It’s highly effective for single- or two-level disease, with 85-90% of patients reporting improved strength and hand function. But there’s a catch: 5-7% of patients develop new problems in the adjacent discs within 10 years.
A newer option is cervical disc arthroplasty (artificial disc replacement). Instead of fusing the bones, they put in a metal-and-plastic disc that moves like a natural one. The FDA approved the first artificial disc for two-level use in March 2023. Early results show 81% of patients kept motion at the treated levels after two years, compared to 63% with fusion. Less stiffness and potentially lower risk of future surgery make this appealing for younger, active patients.
Posterior Approaches
These come from the back of the neck. For multi-level disease (three or more levels), surgeons often use laminoplasty or laminectomy with fusion.
Laminoplasty opens the back of the spinal canal like a door, giving the cord more room without fusing bones. It’s great for preserving neck motion and causes less post-op pain than fusion. Success rates are around 82% for multi-level cases, but neurological recovery is slightly lower than with fusion.
Laminectomy with fusion removes the back part of the vertebrae and fuses the spine. It’s more stable and gives better neurological improvement-up to 85% of patients recover-but it limits neck movement and carries a higher risk of chronic neck pain (18% of patients report this).
Minimally Invasive Options
At Johns Hopkins, surgeons developed a tubular laminoplasty technique that cuts blood loss by 65% and shortens hospital stays by almost two days. These newer methods are becoming more common, especially for patients who want faster recovery.
What to Expect After Surgery
Most people stay in the hospital 1-2 days for anterior surgery and 2-3 days for posterior. Full recovery takes 3-6 months. You’ll need physical therapy for 8-12 weeks, focusing on balance, walking, and strengthening your neck muscles. About 85% of patients follow through with rehab.
Success rates are good: 70-85% of patients see clear neurological improvement. But not everyone gets back to normal. While 82% report better hand function after surgery, only 65% regain full gait stability. About 28% still need a cane or walker long-term.
Common post-op issues include:
- Neck pain (35% of ACDF patients at 6 months)
- Difficulty swallowing (22% in the first few months)
- C5 nerve palsy (temporary arm weakness in 5-10% of cases)
Surgeons with experience-those doing over 50 cervical procedures a year-have 32% fewer complications. So choosing the right surgeon matters as much as the type of surgery.

What Happens If You Don’t Treat It?
Some people hope it will get better on its own. It won’t. The natural course of untreated cervical myelopathy is decline. Studies show 20-60% of patients get significantly worse over 2-5 years. Only 10-15% ever improve without treatment.
Left unchecked, it can lead to permanent paralysis, loss of bowel or bladder control, and inability to walk. The spinal cord doesn’t regenerate. Once nerve fibers are damaged beyond repair, they’re gone for good.
And here’s something most people don’t realize: it often takes over a year to get diagnosed. In one study, 41% of patients saw three or more doctors before someone finally ordered an MRI. If you’ve had hand clumsiness or balance problems for months, don’t wait for someone else to connect the dots.
How to Protect Yourself
If you’re over 55, especially with arthritis or a history of neck injury, pay attention to subtle changes. Don’t brush off dropped keys or tripping on flat ground. Get an MRI if symptoms persist beyond a few weeks.
Before surgery, optimize your health:
- Quit smoking-it cuts fusion failure risk by half.
- Control blood sugar if you’re diabetic-HbA1c below 7.0 reduces infection risk from 8.5% to 3.2%.
- Stay active. Physical therapy before surgery helps preserve strength and speeds recovery.
And remember: timing is everything. The sooner you act, the better your outcome. Waiting isn’t patience-it’s risking permanent damage.
What’s Next in Treatment?
Research is moving fast. Clinical trials are testing drugs like riluzole-used in ALS-to protect the spinal cord during surgery. Early results show 12% greater recovery in JOA scores when combined with surgery.
Robotic-assisted surgery is coming. By 2030, it may become standard for complex cases, reducing revision rates from over 10% to under 7%. Genetic testing may soon help predict who’s at risk for faster degeneration, allowing earlier intervention.
But the biggest challenge isn’t technology-it’s overuse. Experts warn that 15-20% of current surgeries may be unnecessary because of poor patient selection. That’s why getting a second opinion and confirming the diagnosis with MRI is critical.




Virginia Seitz
16 December 2025 - 07:05 AM
This is so important 💔 I dropped my coffee mug last week and thought I was just clumsy-turns out it was my spinal cord screaming for help. Thank you for posting this.
Sachin Bhorde
16 December 2025 - 10:57 AM
Yo, if you're over 50 and your fingers feel like they're wrapped in cotton-GET AN MRI. No cap. I waited 14 months, lost 30% grip strength, and now I'm pre-op. Don't be me. 🚨
Peter Ronai
16 December 2025 - 14:55 PM
Let me guess-someone just posted this because they got a ‘mild’ diagnosis and now they’re panic-scrolling. 85% improvement? Please. Half those patients are just placebo-ing their way through PT while their cord turns to Swiss cheese. And don’t get me started on artificial discs-glorified ball bearings in your neck. You think your spine is a Lego set? 🤡
Brooks Beveridge
18 December 2025 - 06:20 AM
I know this sounds like a stretch, but I’ve seen people come back from this-really. My uncle had CSM, went from needing a walker to hiking again after surgery. It’s not magic, it’s timing. You don’t have to be perfect-you just have to act before the damage becomes permanent. You’re not too old. You’re not too late. Not yet.
And if you’re scared of surgery? I get it. But the real fear isn’t the knife-it’s the silence your body starts making when you ignore it.
Chris Van Horn
18 December 2025 - 12:42 PM
While I appreciate the effort, the author's reliance on the JOA score as a definitive metric is clinically naive. The scale lacks inter-rater reliability in populations with comorbid neuropathies, and its sensitivity to early myelopathic changes is demonstrably inferior to diffusion tensor imaging (DTI). Furthermore, the assertion that 21% of individuals over 40 have asymptomatic stenosis is misleading-it conflates radiographic findings with clinical pathology. One must distinguish between imaging artifacts and neurophysiological compromise. The cited 3% monthly decline in recovery potential lacks robust longitudinal validation; it originates from a single retrospective cohort with selection bias. One must question the evidentiary hierarchy here.
Additionally, the endorsement of artificial disc replacement for two-level disease is premature. The FDA approval was based on non-inferiority trials, not superiority. The long-term wear debris and subsidence rates remain underreported. One cannot ethically promote a device as ‘better’ without addressing its 12% revision rate at five years. The author’s tone suggests a corporate sponsorship agenda.
And while I commend the mention of smoking cessation, the failure to discuss vitamin D3 optimization and its role in bone remodeling is a glaring omission. The human spine is not a mechanical structure-it is a bioactive organ. To treat it otherwise is not medicine-it is engineering.
Finally, the reference to ‘C5 palsy’ as a ‘common’ post-op issue is an understatement. In my own practice, 17% of patients present with transient palsy, and 4% develop permanent deficits. This is not a ‘minor risk.’ It is a catastrophic complication that deserves greater emphasis. The author’s tone is dangerously optimistic.
Steven Lavoie
20 December 2025 - 03:39 AM
Chris, I get that you're passionate about precision-but your comment reads like a peer-reviewed rebuttal, not a Reddit post. The original article was meant for patients, not neurosurgeons. Your nitpicking doesn’t help anyone who’s just trying to understand if they should see a doctor.
Let’s not turn a lifeline into a thesis defense.
Michael Whitaker
20 December 2025 - 05:53 AM
Steven, you’re right-but Chris isn’t wrong either. I’m a retired orthopedic tech. I’ve seen both sides. The problem isn’t the science-it’s the system. Patients get sent to PT for six months because insurance won’t cover the MRI until they’ve ‘tried conservative measures.’ By then, the damage is done. The real villain isn’t the surgeon-it’s the payer. And the real tragedy? People like Virginia-smart, scared, confused-are left to Google their symptoms until they’re paralyzed.
So yes, Chris, your critique is valid. But it’s like yelling at the ambulance driver for driving too fast while the patient is still bleeding out.
amanda s
20 December 2025 - 14:31 PM
Why are we letting foreign doctors dictate our spine care? This whole article reads like a NIH-funded PR stunt. In America, we fix problems with steel and guts-not experimental disc replacements from Japan. If you want real results, get a fusion. No nonsense. No ‘motion preservation’-that’s just a fancy word for ‘we’re not sure it’ll last.’
And don’t even get me started on ‘minimally invasive’-that’s just a marketing term for ‘we’re cutting corners to save money.’ Real surgery is hard. Real surgery is messy. Real surgery leaves scars. And if you’re not willing to pay for that, you deserve what you get.
Joe Bartlett
21 December 2025 - 22:37 PM
UK guys have been doing laminoplasty for decades. We don’t need fancy US gadgets. Just give us a good scalpel and a decent NHS surgeon. This whole ‘artificial disc’ thing is just American capitalism trying to sell you a new toy.
Jigar shah
23 December 2025 - 09:41 AM
Interesting read. But I’m from India-where MRI machines are rare and neurosurgeons are scarce. What do people here do? Do we just wait until we can’t walk? This article is helpful, but it feels like it’s written for people with access. What’s the path for those without?
Anu radha
24 December 2025 - 06:49 AM
My mother had this. She didn’t know what it was. She just said her hands felt ‘heavy.’ I wish I’d read this sooner. Thank you for sharing. 💛