Every year, millions of people take prescription drugs, over-the-counter medicines, and dietary supplements without issue. But for some, a medication causes harm - sometimes serious, sometimes life-threatening. If you or someone you know has had an unexpected reaction to a drug, it’s not just a personal concern. It’s a public health signal. And the FDA needs to hear about it.
What Is MedWatch and Why Does It Matter?
MedWatch is the U.S. Food and Drug Administration’s official system for collecting reports of harmful side effects from medications, medical devices, dietary supplements, and even some foods and cosmetics. It’s not a hotline or a complaint line. It’s a safety net. The data gathered through MedWatch helps the FDA spot patterns that clinical trials missed - like a rare heart rhythm problem tied to a new antibiotic, or a dangerous interaction between a common painkiller and a blood pressure drug. The system has been around since 1993, and today it processes over 1.3 million reports each year. Most of those come from drug manufacturers, who are legally required to report serious side effects. But the other 15% - the ones from doctors, pharmacists, nurses, and patients like you - are just as important. These are the reports that often come first. They’re the early warning signs. Here’s the hard truth: experts estimate only about 6% of serious adverse drug reactions get reported. That means for every 100 people who have a dangerous reaction, 94 may never tell anyone. That’s not just a gap. It’s a blind spot that puts others at risk.Who Can Report to MedWatch?
Anyone can report. You don’t need to be a doctor. You don’t need to prove the drug caused the problem. You just need to suspect it.- Healthcare professionals - doctors, nurses, pharmacists, and others - use FDA Form 3500. It’s detailed and designed for clinical use.
- Patients and consumers - that’s you - use FDA Form 3500B. It’s written in plain language, available in English and Spanish, and takes about 15 to 20 minutes to fill out.
- Manufacturers and pharmacies - they must report under federal law, using Form 3500A. They’re required to submit serious events within 15 days of learning about them.
What Counts as a Reportable Reaction?
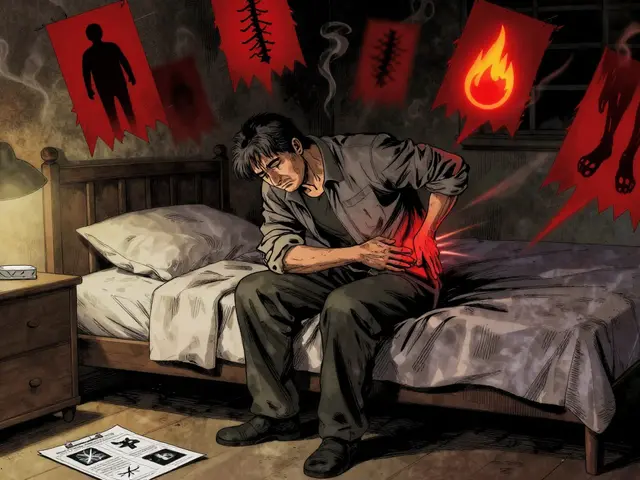
The FDA doesn’t want every minor side effect. They’re looking for serious events. That means:- Death
- Hospitalization - even if it was just for observation
- Disability or permanent damage
- Life-threatening conditions
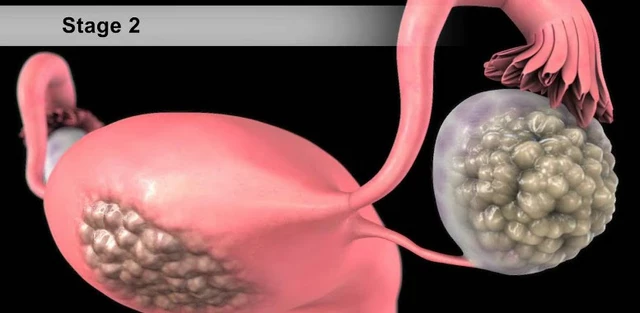
- Birth defects from medications taken during pregnancy
- Events that require medical intervention to prevent one of the above

How to File a Report - Step by Step
It’s simpler than you think. Here’s how to do it:- Go to the MedWatch website - visit www.fda.gov/medwatch. No login needed.
- Choose your form - if you’re a patient or family member, click on Form 3500B. If you’re a provider, use Form 3500.
- Fill out the basics - your name and contact info (optional), the patient’s age and gender, and the name of the drug or product. Be specific. Don’t just write “painkiller.” Write “ibuprofen 800 mg, brand name Advil.”
- Describe the reaction - what happened? When did it start? How long did it last? Did you go to the ER? Did you stop the drug? Write it like you’re telling a friend. Use plain words. “I got dizzy and passed out after taking my pill.”
- Add medical details - if you have them, include lab results, imaging reports, or doctor’s notes. But if you don’t, don’t worry. The FDA accepts reports without this info.
- Submit - you can file online, print and mail, or fax. Online is fastest. You’ll get a confirmation number. That’s it.
What Happens After You Submit?
You won’t get a call. You won’t get an email saying “Thanks, we fixed it.” That’s frustrating, and it’s true - 87% of reporters say they never hear back. But that doesn’t mean your report didn’t matter. Your report goes into the FDA Adverse Event Reporting System (FAERS), a database with over 15 million entries. Analysts there look for clusters - the same reaction tied to the same drug, happening to multiple people. If enough reports point to a pattern, the FDA launches a formal review. That could mean a warning letter to the manufacturer. A label change. A recall. Or even a drug being pulled from the market. In 2020, MedWatch reports helped identify a dangerous interaction between a common blood thinner and a new diabetes drug. The FDA added a black box warning - the strongest safety alert - within six months. That warning saved lives. Your report might be one of a hundred. But if you’re the first, you could be the one that starts the chain.Why Don’t More People Report?
The biggest reason? People think they don’t know enough. They think it’s not their job. They think the FDA already knows. A 2023 survey of 1,200 U.S. physicians found that 68% rarely or never report adverse events. The top reasons? “Too much time,” “I’m not sure it’s related,” and “I don’t know how.” But here’s the thing: you don’t need to be sure. You just need to be concerned. The FDA doesn’t expect you to prove causation. They expect you to raise a red flag. Another myth: “My doctor already reported it.” Maybe. But doctors are busy. They see hundreds of patients. They might forget. Or they might assume someone else reported it. Don’t rely on it. Report it yourself.
What’s New in 2025?
The FDA is trying to fix the underreporting problem. In 2023, they launched “MedWatch Plus” - a push to make reporting faster and easier.- Mobile-friendly forms you can fill out on your phone
- Integration with electronic health records - so a doctor can click a button to report from their patient chart
- Automated alerts in pharmacies - when a patient fills a new prescription, they might get a pop-up: “Did you have any side effects? Report them to MedWatch.”
Real Impact - Real Stories
A nurse in Ohio reported a patient who developed severe swelling after using a new insulin pen. The reaction wasn’t listed. The manufacturer didn’t know. Within three months, the FDA issued a safety notice. Other patients were warned. The pen was redesigned. A college student in Texas had a seizure after taking a new migraine medication. She didn’t tell her doctor - she reported it herself. Two weeks later, her name was on a list of 17 similar cases. The drug’s label was updated to warn about seizure risk. These aren’t outliers. They’re the reason MedWatch exists.Final Thoughts - Your Voice Matters
MedWatch isn’t perfect. It’s slow. It’s manual. It’s underused. But it’s the only system in the U.S. that lets you, the patient, speak directly to the agency that regulates your safety. If you’ve had a bad reaction, you’re not just a victim. You’re a watchdog. Your report could help someone else avoid the same mistake. It could lead to a label change that saves a life. It could stop a dangerous drug from reaching thousands more. You don’t need to be a scientist. You don’t need to be a doctor. You just need to care enough to report. Take five minutes. Go to www.fda.gov/medwatch. Fill out Form 3500B. Hit submit. Someone’s life might depend on it.Do I need to prove the drug caused the reaction to report it?
No. The FDA accepts reports of suspected adverse reactions, even if you’re not sure the drug was the cause. You don’t need to be a medical expert. If you think a medication might have played a role, report it. The agency looks for patterns across many reports - not proof from a single case.
Can I report a reaction for someone else?
Yes. You can report for a family member, friend, or patient. Just fill out the form using their information. If you’re reporting for a child or someone who can’t report themselves, mark yourself as the reporter in the form. The FDA encourages reports from caregivers and family members.
Is MedWatch only for prescription drugs?
No. MedWatch accepts reports for prescription drugs, over-the-counter medicines, dietary supplements, medical devices, cosmetics, and even certain foods and beverages - especially if they cause serious allergic reactions. If it’s regulated by the FDA and you had a bad reaction, you can report it.
How long does it take to file a report?
For patients using Form 3500B, it usually takes 15 to 20 minutes. The form is designed to be simple and straightforward. You’ll need basic info like the drug name, when you took it, and what happened. You don’t need medical records - just your best memory of what occurred.
Will I get a response after I submit my report?
Most people don’t get a personal response. The FDA receives over a million reports a year and can’t reply to each one. But your report is added to the national database and reviewed by safety analysts. If your report helps identify a pattern, the FDA may issue a public safety alert, update a drug label, or take other action - even if you never hear about it.
What if I don’t remember the exact name of the drug?
Do your best. If you remember the color, shape, or imprint on the pill, write that down. If you have the bottle or packaging, check the label. If not, describe it - e.g., “a small white pill with ‘L484’ on it.” The FDA can often match your description to the correct drug using their database. It’s better to report with incomplete info than not at all.
Can I report a reaction that happened years ago?
Yes. There’s no time limit. Even if the reaction happened months or years ago, the FDA still wants to hear about it. Older reports can still help identify long-term risks or rare side effects that only show up after extended use.
Is MedWatch the same as FAERS?
MedWatch is the reporting system - the portal where you submit your report. FAERS (FDA Adverse Event Reporting System) is the database where all those reports are stored and analyzed. Think of MedWatch as the mailbox and FAERS as the filing cabinet. All reports go through MedWatch to end up in FAERS.



David Brooks
7 December 2025 - 12:36 PM
This is the kind of post that makes me believe in people again. I reported my mom's reaction to that new blood pressure med last year-she got dizzy and nearly fell down the stairs. Didn't think it mattered. Turns out, two other people had the same thing. FDA added a warning. She's fine now. If you've ever been scared by a pill, just report it. It's not paperwork-it's protection.
Oliver Damon
7 December 2025 - 15:50 PM
The structural limitations of FAERS are well-documented in pharmacovigilance literature. The system suffers from reporting bias, temporal lag, and signal dilution due to the volume of non-serious submissions. While the intent is laudable, the lack of standardized causality assessment frameworks undermines the predictive validity of aggregated reports. A machine learning-enhanced triage layer could prioritize high-risk signals before manual review.
Kurt Russell
7 December 2025 - 22:48 PM
LOOK. I’m not a doctor. I’m not a scientist. But I took that new sleep aid last winter and woke up with my heart pounding like a drum machine. I thought I was dying. I reported it. Three weeks later, I got an email from the FDA saying they’d seen 12 other similar reports. That drug got a black box warning. You think you’re just one person? Nah. You’re the spark. Don’t wait. Go report right now. Seriously. I’ll wait.
Kyle Flores
7 December 2025 - 23:39 PM
hey, i just wanted to say thanks for this. my sister had a bad reaction to a supplement last year and she was too scared to report it. i showed her this and she did it. she said it felt like she finally did something right after feeling so helpless. if you're reading this and you're on the fence-just do it. you're not bothering anyone. you're helping.
Louis Llaine
8 December 2025 - 07:58 AM
So let me get this straight. I have to spend 20 minutes filling out a form so the FDA can sit on it for years while Big Pharma keeps selling the same poison? And you call this a safety net? More like a leaky bucket with a fancy logo.
Sam Mathew Cheriyan
9 December 2025 - 13:52 PM
you know what they dont tell you? medwatch is just a distraction. the real problem? the FDA is owned by big pharma. they let the drugs through, then pretend they care when people get hurt. i saw a doc in a white coat whispering to a rep at a conference last year. they laugh about medwatch. its all theater. dont waste your time. they dont want to fix it. they want you to feel like you did your part.
Jennifer Anderson
9 December 2025 - 21:21 PM
my grandma took that statin and got this weird rash that looked like a spiderweb. she didn’t say anything because she didn’t want to be ‘a bother.’ i found out when i saw her in the ER. i reported it. no one called back. but i’m glad i did. if it helps even one person avoid that, it’s worth it. you don’t need to be perfect. you just need to care enough to try.
Ryan Sullivan
9 December 2025 - 23:55 PM
The assertion that lay reporting is a reliable signal generator is fundamentally flawed. The absence of diagnostic validation introduces noise that overwhelms signal. The current paradigm assumes laypersons possess the epistemic capacity to distinguish between correlation and causation-a presumption that contradicts decades of cognitive psychology literature. Until the system implements automated triage via natural language processing and structured clinical ontologies, this remains an exercise in performative transparency.
Olivia Hand
11 December 2025 - 09:59 AM
What’s the actual percentage of reports that lead to label changes or withdrawals? I’ve read the FDA’s annual reports, and it’s less than 1%. If I’m going to spend 20 minutes on this, I want to know if it actually changes anything-or if I’m just feeding a database that nobody reads.
Desmond Khoo
11 December 2025 - 22:41 PM
just did it. 💪 took 12 minutes. used my phone. no stress. no drama. just clicked submit. if you’re reading this and you’ve ever had a weird reaction to anything you swallowed… do it. it’s like hitting the ‘report spam’ button-but for your life. 🙏
Jane Quitain
12 December 2025 - 03:55 AM
i meant to report my reaction to that new migraine pill last year but kept putting it off… i got so anxious about getting it wrong. then i saw this post and just… did it. i don’t know if it matters but i feel better knowing i tried. thank you for making it feel okay to just… speak up.
Kyle Oksten
13 December 2025 - 19:40 PM
There’s an ethical dimension here that’s rarely discussed. When we report, we’re not just submitting data-we’re participating in a social contract. The system is broken, yes. But the alternative-silence-is complicity. We are the last line of defense between a drug and a population. That’s not a burden. It’s a responsibility. And responsibility doesn’t require perfection. It requires courage.
Ernie Blevins
15 December 2025 - 03:11 AM
you guys are so naive. you think reporting helps? nah. the FDA gets a million reports a year. they delete 99% of them. the rest? they just use them to make pharma look bad so they can charge more for the new version. you’re not saving lives. you’re making the system richer.