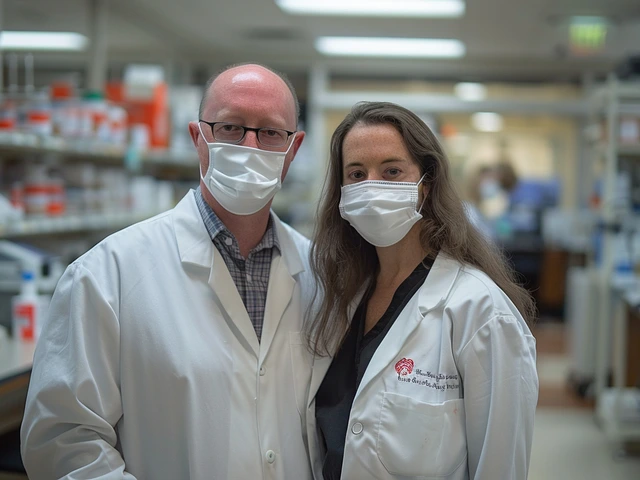
Generic drugs save patients and the healthcare system billions each year. In the U.S., 90.7% of all prescriptions are filled with generics - but not all generics are created equal. While the FDA requires them to match brand-name drugs in active ingredients, strength, and dosage, there are real, documented cases where patients experience unexpected side effects, therapeutic failure, or even harm after switching to a different generic manufacturer. Pharmacists are on the front lines of this issue. They’re the ones who see the patient who says, "This new pill doesn’t work like the last one," or whose lab results suddenly go off track. Knowing when to flag these problems isn’t optional - it’s part of the job.
Why Some Generics Just Don’t Work the Same
The FDA’s approval process for generics hinges on bioequivalence: the generic must deliver the same amount of active ingredient into the bloodstream as the brand, within a range of 80% to 125%. That sounds precise, but a 20% variation on either side means two different generics of the same drug could deliver significantly different doses. For most medications, that’s fine. For others, it’s dangerous. Take levothyroxine, used to treat hypothyroidism. A 2021 study in the Journal of the American Pharmacists Association found that switching between generic manufacturers led to therapeutic failure in over twice as many patients compared to staying on one version. One patient’s TSH level jumped from 2.1 to 8.7 after a switch - a clear sign their thyroid wasn’t getting enough hormone. That’s not a fluke. The FDA has flagged 18 drugs as having a narrow therapeutic index (NTI), meaning even small changes in blood levels can cause toxicity or treatment failure. Others include warfarin, phenytoin, lithium, and digoxin. For these, a 10% difference in absorption can mean the difference between a seizure and stability. Extended-release formulations are another weak spot. A 2020 FDA analysis found that 7.2% of generic extended-release opioids failed dissolution testing - meaning the drug didn’t release properly over time. Patients got a spike of medication all at once, then nothing. That’s not just ineffective - it’s risky. The FDA issued a warning in 2023 about certain generic versions of diltiazem CD after 47 cases of therapeutic failure were reported. These aren’t rare anomalies. They’re patterns.The Look-Alike, Sound-Alike Trap
Another silent killer in pharmacy is confusion between similarly named drugs. The Institute for Safe Medication Practices reports that 14.3% of all generic medication errors come from look-alike or sound-alike names. Consider these pairs:- Oxycodone/acetaminophen vs. hydrocodone/acetaminophen
- Clonazepam vs. clonidine
- Epinephrine vs. ephedrine
When to Flag a Problem - The Pharmacist’s Checklist
Not every patient complaint means a bad generic. But there are clear red flags. Here’s what pharmacists should watch for:- Therapeutic failure within 2-4 weeks after switching to a new generic - especially with NTI drugs. If a diabetic’s HbA1c climbs or a seizure patient starts having breakthrough episodes, don’t assume non-adherence. Check the manufacturer.
- Unexplained side effects that weren’t present before the switch. New dizziness, nausea, or fatigue could signal a different inactive ingredient or inconsistent release profile.
- Lab value shifts. For drugs like warfarin, lithium, or tacrolimus, a change in blood level of more than 15-20% after a generic switch is a red flag. Therapeutic drug monitoring exists for a reason.
- Patient reports of different pill appearance. If a patient says, "This one is smaller, paler, or has a different imprint," it’s worth verifying the manufacturer. Sometimes, a change in pill shape or color leads to patient confusion or non-adherence.
- Multiple switches. Patients who’ve been switched back and forth between generics - especially for NTI drugs - are at higher risk. Document every manufacturer change.
What Happens When Pharmacists Speak Up
When a pharmacist flags an issue, it triggers a chain reaction. They can:- Switch the patient back to the original generic or brand
- Report the issue to the FDA’s MedWatch system - average submission time is under 5 minutes
- Notify the prescriber with lab data and manufacturer details
- Document the manufacturer name on the prescription label for future reference
The Bigger Picture: Why This Matters
Generics make healthcare affordable. But affordability shouldn’t mean compromising safety. The FDA inspected over 2,100 manufacturing facilities in 2022 and found 187 data integrity issues and 243 quality control failures. Most of these were at overseas plants - in India and China, where 88% of U.S. generic ingredients come from. The FDA is now ramping up inspections and testing, with plans to increase sampling of generics by 40% over the next three years. Meanwhile, states are starting to act. Four states - Massachusetts, New York, Texas, and Virginia - require pharmacists to get explicit consent before substituting NTI generics. Other states are considering similar rules. Pharmacists who understand the science behind these issues aren’t just following protocols - they’re preventing harm.
What Patients Don’t Tell You
A 2023 Consumer Reports survey found that while 78% of patients were happy with generics because of cost, 22% reported different side effects after switching manufacturers. Most never told their pharmacist. They just stopped taking the pills. Or they assumed it was "all in their head." That’s why pharmacists need to proactively ask: "Has anything changed since your last refill?" Even small changes matter.What You Can Do Today
If you’re a pharmacist:- Check the FDA’s Orange Book before dispensing NTI drugs
- Record the manufacturer name on every generic prescription
- Use the FDA’s MedWatcher app to report suspected problematic generics
- Educate technicians on look-alike/sound-alike risks
- Ask patients: "Do you feel any different since your last refill?"
- Write "Dispense as Written" or "Do Not Substitute" on prescriptions for NTI drugs
- Ask your pharmacist if they’ve seen any issues with the generic you’re prescribing
Are all generic drugs safe?
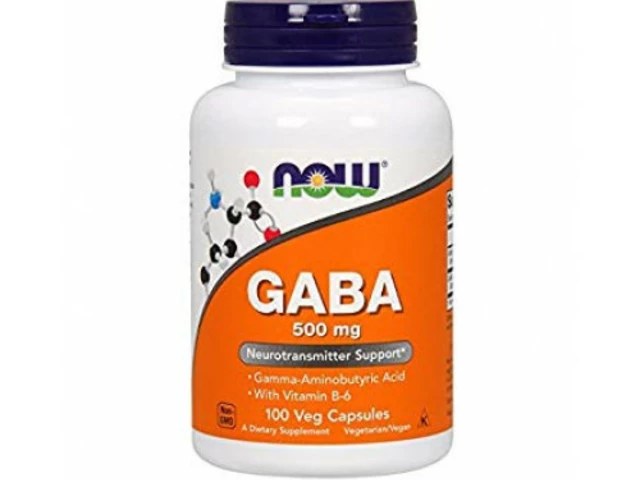
Most are - over 90% of generics work just as well as brand-name drugs. But safety isn’t guaranteed for every manufacturer or every drug. Certain types - like narrow therapeutic index drugs (e.g., levothyroxine, warfarin) and extended-release formulations - have higher rates of issues. The FDA approves generics based on bioequivalence, but that allows for up to 20% variation in how the drug is absorbed. For some patients, that’s enough to cause problems.
What is a narrow therapeutic index (NTI) drug?
An NTI drug has a very small range between an effective dose and a toxic dose. Even small changes in blood levels can lead to treatment failure or serious side effects. Examples include levothyroxine, warfarin, phenytoin, lithium, digoxin, and tacrolimus. For these drugs, switching between generic manufacturers can be risky. Pharmacists should avoid unnecessary switches and monitor patients closely if a switch occurs.
How can I tell if a generic drug is problematic?
Watch for three signs: 1) The patient reports a change in how the drug works or new side effects after switching manufacturers; 2) Lab results show a significant shift (e.g., TSH, INR, or drug levels outside the therapeutic range); 3) The generic has an "BX" rating in the FDA’s Orange Book, meaning it’s not considered therapeutically equivalent. Document the manufacturer, check the pill’s appearance, and talk to the patient.
Can pharmacists refuse to substitute a generic?
Yes - in many cases. Federal law allows pharmacists to substitute generics unless the prescriber writes "Dispense as Written" or "Do Not Substitute." But even when substitution is allowed, pharmacists have a professional obligation to refuse if they believe the switch could harm the patient. For NTI drugs, many states now require patient consent before substitution. Pharmacists who flag unsafe generics are acting within their scope of practice - and often preventing harm.
Why do some generics have different effects if they have the same active ingredient?
The active ingredient is the same, but the inactive ingredients - like fillers, binders, and coatings - can differ. These affect how quickly the drug dissolves and is absorbed. For extended-release pills, a different coating might cause the drug to release too fast or too slow. A 2020 FDA study found 7.2% of generic extended-release opioids failed dissolution testing. Also, manufacturing quality varies. Some plants have data integrity or quality control issues, which the FDA has documented in over 400 facilities since 2020.