Rifampin Contraceptive Effectiveness Checker
Check Your Contraceptive Safety
Rifampin can reduce the effectiveness of hormonal birth control, potentially leading to unintended pregnancy. Select your contraceptive method to see if it's affected and what to do.
When you're taking rifampin for tuberculosis or another infection, you might not think twice about your birth control pill. But here’s the hard truth: rifampin can make your hormonal contraception fail-even if you take it perfectly every day. This isn’t a myth, a rumor, or a rare outlier. It’s a well-documented, clinically proven interaction that has led to real pregnancies in women who followed all the rules.
How Rifampin Breaks Down Your Birth Control
Rifampin doesn’t just kill bacteria-it rewires your liver. It turns on enzymes, specifically the CYP3A4 family, that are meant to break down toxins. But here’s the problem: those same enzymes also break down the hormones in your birth control pill-ethinyl estradiol and progestin. Studies show that when rifampin is taken alongside combined oral contraceptives, estrogen levels drop by 42% to 66%. Progestin levels? They can plunge by up to 83%. That’s not a small tweak. That’s enough to stop ovulation suppression.What does that mean for you? Your body may start ovulating again, even while you’re taking your pill. And if you’re having sex, that means pregnancy is possible. This isn’t theoretical. A 2024 review of clinical data from the National Institutes of Health found that in two out of four studies, women taking rifampin experienced breakthrough ovulation. In all five studies, hormone exposure dropped significantly.
Why This Isn’t Like Other Antibiotics
You’ve probably heard that antibiotics can mess with birth control. Maybe your doctor warned you about amoxicillin or azithromycin. But here’s the key difference: rifampin is the only antibiotic with solid, repeated proof of reducing contraceptive effectiveness. Other antibiotics? The evidence doesn’t hold up. A 2018 review of 23 studies found no link between non-rifamycin antibiotics and reduced hormone levels or increased ovulation.That’s why experts are so clear about this. The Journal of the Society of Obstetricians and Gynaecologists of Canada states bluntly: “Rifampin is the only antibiotic that has been reported to reduce plasma estrogen concentrations. When taking rifampin, oral contraceptives cannot be relied upon for contraception.” The CDC, WHO, and American Academy of Family Physicians all agree. Rifampin is in a class of its own.
What About Rifabutin? Is It Safer?
Rifabutin is a cousin of rifampin, used sometimes for TB or MAC infections. It’s less potent at inducing liver enzymes. Studies show it doesn’t trigger the same level of hormone breakdown. One study even found no ovulation in women taking rifabutin and birth control together. But that doesn’t mean it’s safe. The NIH review says the interaction is still “to a lesser extent.” So if you’re on rifabutin, don’t assume you’re in the clear. Play it safe-use backup protection.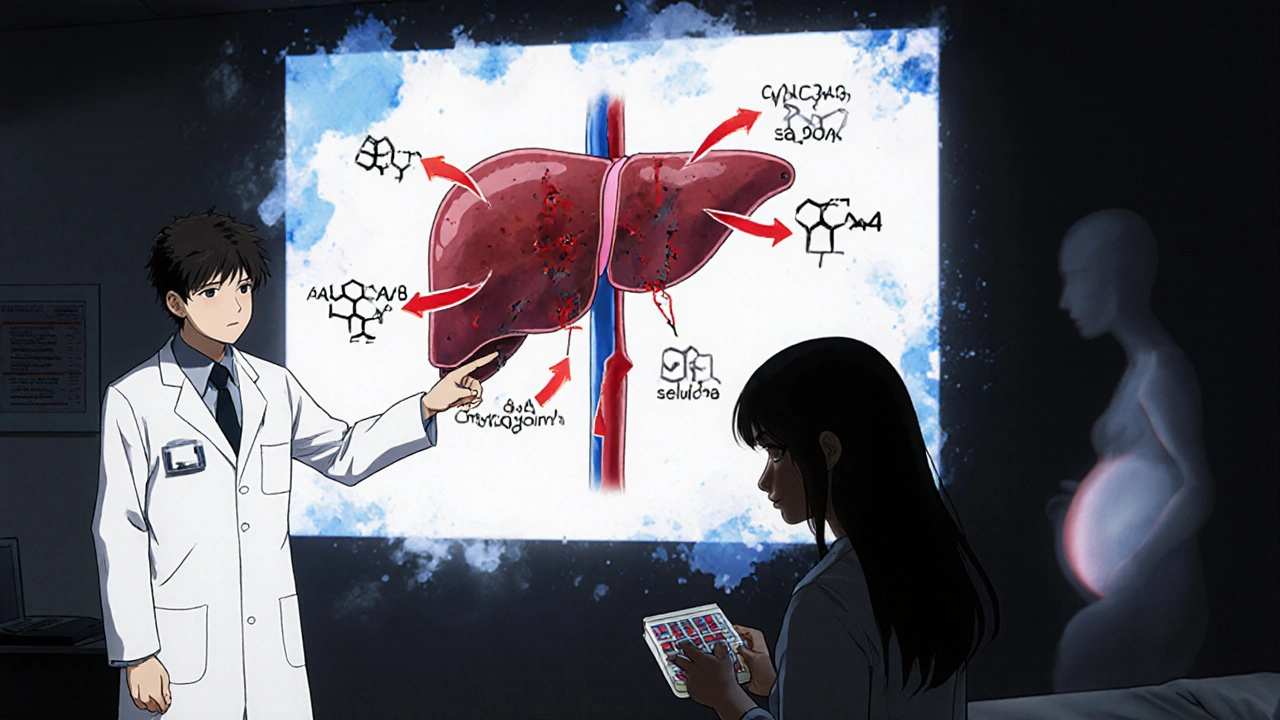
Real Stories, Real Risk
Behind the numbers are real people. On a women’s health forum, one user wrote: “I was on Ortho Tri-Cyclen while taking rifampin for TB and got pregnant despite perfect pill adherence.” Her OB/GYN confirmed it was the drug interaction. Another user on Reddit shared: “My professor who specializes in infectious diseases said he’s seen at least three pregnancies in his 20-year career specifically from the rifampin-contraceptive interaction, but never from other antibiotics.”These aren’t isolated cases. Between 1970 and 1999, the UK’s Committee on Safety of Medicines recorded 150 cases of contraceptive failure linked to antibiotics. Rifampin was the common thread in many of them. And while modern reporting is better, the risk hasn’t gone away. The FDA’s own label for rifampin warns: “Decreased effectiveness of oral or other steroid contraceptives.”
What Should You Do?
If you’re prescribed rifampin and use hormonal birth control, here’s what you need to do:- Use a backup method-like condoms-during the entire time you’re taking rifampin.
- Keep using backup contraception for 28 days after you stop rifampin. Why? The enzyme-inducing effect doesn’t vanish the day you finish the last pill. Your liver needs time to reset.
- Consider switching to a non-hormonal method while on rifampin. A copper IUD works perfectly. So does a progestin implant. Neither is affected by liver enzymes.
- Don’t rely on higher-dose pills. Some doctors suggest switching to a pill with 50 mcg of ethinyl estradiol, but there’s no solid proof it works. Don’t gamble your fertility on unproven fixes.
What About Other Contraceptive Options?
Not all birth control is created equal when it comes to rifampin. Here’s what’s safe:- Copper IUD: No hormones. No interaction. 99% effective for up to 12 years.
- Progestin-only implant: Placed under the skin. Lasts 3-5 years. Not affected by liver enzymes.
- Progestin-only pill (POP): Also called the mini-pill. Less reliable than combined pills even without rifampin, and still affected by enzyme inducers. Not recommended as a standalone option.
- Depo-Provera shot: Injected every 3 months. Evidence is mixed, but it’s not metabolized the same way as oral pills. Some experts consider it safer, but backup is still advised.
- Barrier methods: Condoms, diaphragms, cervical caps. They work if used correctly every time.
And if you’re thinking about getting an IUD or implant while on rifampin? Go ahead. There’s no interaction. In fact, many providers recommend it as the best option during TB treatment.
Why Don’t Pharmacies Warn You Better?
You’d think pharmacies would flag this interaction every time rifampin is dispensed with birth control. But they don’t always. The FDA requires the warning on rifampin’s label, but pharmacy software doesn’t always catch it unless the system is finely tuned. And many women don’t even realize their pill is hormonal contraception-some think it’s just for acne or periods.That’s why it’s on you to ask. When your doctor prescribes rifampin, say: “Will this affect my birth control?” If they say no, push back. Cite the CDC or WHO guidelines. Bring this article. You’re not being difficult-you’re protecting your health.
What’s Next?
Researchers are looking into whether genetic testing can predict who’s most at risk. Some women naturally produce more CYP3A4 enzymes-so rifampin hits them harder. If that testing becomes routine, we might one day personalize birth control advice. But for now? No test. No shortcut. Just one simple rule: use backup contraception.And if you’re planning to get pregnant after rifampin? You don’t need to wait. Once you stop the drug, your hormones will return to normal within a few weeks. No lingering damage. Just a reminder: if you’re not ready for pregnancy, don’t skip the backup.
Bottom Line
Rifampin and hormonal birth control don’t mix. Not even a little. It’s not about missing a pill. It’s not about timing. It’s about your liver turning on a chemical factory that destroys the hormones keeping you protected. The risk is real. The data is clear. And the solution? Simple: use condoms or switch to a non-hormonal method while you’re on rifampin-and for a full month after.Don’t wait for a surprise pregnancy to learn this lesson. If you’re on rifampin, act now. Your body-and your future-depend on it.
Can rifampin cause pregnancy even if I take my birth control perfectly?
Yes. Rifampin doesn’t make you miss pills-it changes how your body processes the hormones. Even perfect adherence won’t stop your liver from breaking down estrogen and progestin faster than normal. This can lead to ovulation and pregnancy, regardless of how carefully you take your pill.
Is the birth control pill still effective if I take rifampin at a different time of day?
No. Timing your pill differently won’t help. Rifampin triggers enzyme induction in your liver, which is a systemic effect. Whether you take rifampin in the morning and your pill at night, your body still breaks down the hormones at a higher rate. The only solution is backup contraception.
Are all types of birth control affected by rifampin?
Only hormonal methods are affected-especially those with estrogen and/or progestin, like the pill, patch, or ring. Non-hormonal options like the copper IUD and condoms are completely safe. Progestin-only implants are also unaffected and are a recommended alternative during rifampin treatment.
How long after stopping rifampin should I keep using backup birth control?
Use backup contraception for 28 days after your last dose of rifampin. The enzyme-inducing effect lingers in your liver for several weeks. Stopping the drug doesn’t instantly reset your metabolism. Waiting a full month ensures your hormone levels have returned to normal before relying on your birth control again.
Can I switch to a higher-dose birth control pill to counteract rifampin?
Some doctors suggest pills with 50 mcg of ethinyl estradiol, but there’s no strong evidence this works reliably. The hormone reduction caused by rifampin is so significant that even higher doses may not be enough. The CDC and WHO do not recommend this approach. Backup contraception is the only proven safety net.
What if I’m on rifampin for TB and I’m pregnant? Will it harm the baby?
Rifampin is considered safe during pregnancy and is part of standard TB treatment for pregnant women. The concern isn’t that rifampin causes birth defects-it’s that it can cause unintended pregnancy in the first place. If you become pregnant while on rifampin, continue your TB treatment as prescribed. Talk to your OB/GYN about managing both conditions safely.
Why don’t more doctors know about this interaction?
Many providers still believe all antibiotics affect birth control, which is incorrect. The confusion has led to complacency. But the data is clear: only rifampin and rifabutin have proven effects. If your doctor dismisses your concern, bring the CDC guidelines or the 2024 NIH review. You’re not wrong-you’re informed.




jobin joshua
30 November 2025 - 04:30 AM
Bro, I just got prescribed rifampin for TB and was on the pill 😳 I had no idea. Thanks for this post. Just grabbed condoms and a copper IUD consult. 🙏
Sue Barnes
1 December 2025 - 21:25 PM
People still don't get it. You think your doctor knows this? Half of them still say 'just take it at a different time.' I've seen three pregnancies from this. It's not a suggestion. It's a warning label on your life.
King Property
2 December 2025 - 20:33 PM
This is why you don't trust the medical system. They'll let you take a drug that nukes your birth control and then act like it's your fault when you get pregnant. The FDA label is there. The CDC says it. But your pharmacist? Still silent. It's systemic negligence.
Yash Hemrajani
4 December 2025 - 16:59 PM
Oh wow, another person who thinks rifampin is just another antibiotic. Let me guess - you also think vitamin C cures COVID? The liver enzyme induction isn't magic, it's biochemistry. If you're on rifampin and still using the pill, you're not 'careful,' you're just lucky so far.
Diana Askew
5 December 2025 - 14:02 PM
I bet Big Pharma knows about this and hides it. Why else would they let millions of women take this combo? They profit off both the TB drugs AND the abortions/pregnancies. It's not an accident - it's a business model.
Pawittar Singh
6 December 2025 - 14:08 PM
Hey, I'm a med student and this is SO important. I used to think all antibiotics messed with birth control too - until I saw the data. Seriously, if you're on rifampin, go get a copper IUD. It's a one-time thing, lasts 12 years, and you never have to think about it again. You're worth the safety net 💪❤️
Josh Evans
8 December 2025 - 07:02 AM
I'm on rifampin right now and switched to the implant last week. Best decision ever. No more stressing about timing or condoms. Just... done. Thanks for the clarity, OP.
Allison Reed
9 December 2025 - 09:31 AM
The fact that this interaction is so well-documented yet still overlooked by so many providers is terrifying. Women deserve accurate, consistent information - not guesswork. This post should be required reading for every OB-GYN and pharmacist in the country.
Jacob Keil
9 December 2025 - 11:56 AM
like... is it really the liver? or is it some kind of quantum entanglement between drugs and hormones? i mean, we dont even know what consciousness is but we trust pills to work? maybe its all a simulation and the pill never worked anyway 😶🌫️
Sachin Agnihotri
10 December 2025 - 22:03 PM
I appreciate the depth here, but let’s not panic. Rifampin is serious, yes - but so is TB. The key is awareness, not fear. I’ve seen patients on rifampin for 6 months and they all used IUDs. It’s not complicated. Just talk to your provider, bring this info, and choose safety. No drama needed. 🙏