Medication Side Effects: What You Need to Know About Risks and How to Stay Safe
When you take a medication side effect, an unintended reaction to a drug that can range from mild discomfort to serious harm. Also known as adverse drug reactions, these are not rare mistakes—they’re predictable outcomes tied to how your body processes chemicals. Every pill, injection, or patch you use has the potential to trigger something your doctor didn’t plan for. That’s not because the drug is broken. It’s because your body is unique. What’s harmless to one person might cause dizziness, bleeding, or even organ damage in another.
Some adverse drug reactions, harmful responses to medications that require medical attention show up fast—like a rash after an antibiotic. Others creep in slowly, like memory loss from a sleep aid taken for months. Older adults are especially vulnerable. Drugs like benzodiazepines, blood pressure meds, and antidepressants can increase fall risk, confusion, or even hospital stays. The high-risk medications, drugs with known dangers for specific groups, especially seniors aren’t always obvious. Many are prescribed legally, taken as directed, and still cause harm because the risks weren’t clearly explained.
It’s not just about what’s in the bottle. generic drug risks, safety issues linked to manufacturing flaws in non-brand medications are real. Tablets that crumble, capsules with uneven doses, or contamination from poor production lines can turn a safe drug into a danger. The FDA tracks these problems, and patients are reporting them through systems like MedWatch. You don’t need to be a doctor to spot a problem. If your pill looks different, or you feel worse after switching brands, that’s not in your head. It’s data.
And it’s not just about single drugs. Interactions matter. Rifampin can make birth control useless. Carbamazepine can knock out the effect of blood thinners. NSAIDs can flood your body with fluid if you have heart failure. These aren’t theoretical risks—they’re documented, preventable, and often missed because no one connected the dots.
You’re not powerless here. You can learn to read the fine print. You can ask about alternatives. You can track your symptoms and report them. You can check your medicine cabinet for expired drugs that might be doing more harm than good. The posts below cover exactly these kinds of real-world situations: how to spot dangerous side effects, what drugs to question, how to use naloxone in an emergency, why some generics fail, and how to talk to your doctor without sounding paranoid. These aren’t theoretical guides. They’re tools built from actual patient reports, FDA data, and clinical warnings. What you find here could keep you—or someone you love—out of the hospital.
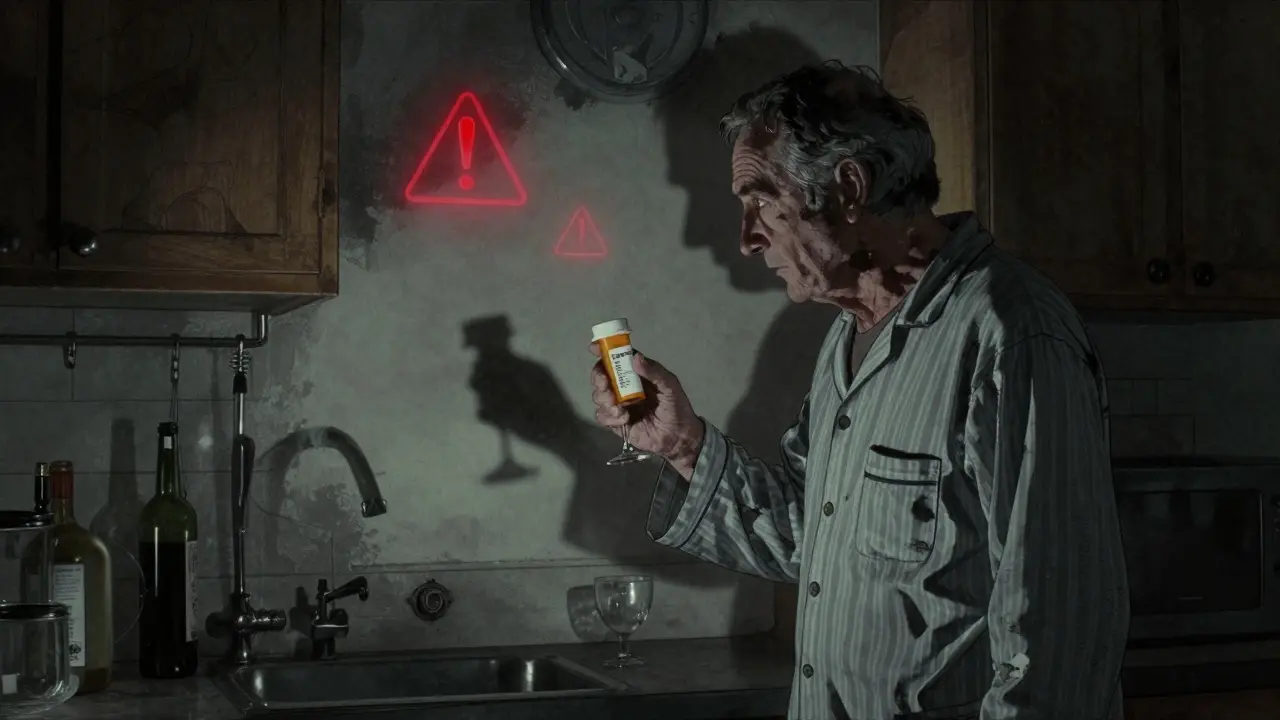
Alcohol and Prescription Drugs: Dangerous Interaction Effects
Alcohol and prescription drugs can interact dangerously, leading to overdose, liver damage, or death. Learn which medications are most risky, who’s most vulnerable, and how to stay safe.
Read More
Deprescribing Frameworks: How to Safely Reduce Medications and Cut Side Effects
Deprescribing frameworks help safely reduce unnecessary medications in older adults, cutting side effects, falls, and hospitalizations. Evidence shows it’s safe, effective, and urgently needed as polypharmacy rises.
Read More
Questions to Ask Your Doctor About Medication Side Effects
Learn the essential questions to ask your doctor about medication side effects to avoid dangerous reactions, reduce ER visits, and take control of your health. Based on FDA, CDC, and clinical guidelines.
Read More
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: Recognizing Medication-Related Emergencies
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis are rare but deadly skin reactions caused by medications. Learn the warning signs, high-risk drugs, and why immediate hospital care is critical to survival.
Read More