SJS/TEN Symptom Checker
This tool helps identify potential signs of Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN) based on symptoms and medication history. THIS IS NOT A DIAGNOSTIC TOOL. If you experience symptoms described below, stop the medication immediately and seek emergency medical care.
Includes anticonvulsants, sulfonamide antibiotics, allopurinol, or NSAIDs.
What You Need to Know About Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) aren’t just rare skin rashes. They’re life-threatening emergencies triggered by medications, and they can turn deadly within days if missed. The first sign? A fever, sore throat, or flu-like feeling that doesn’t go away. Then comes the rash-red, painful, spreading fast. Blisters form. Skin starts peeling off. Eyes, mouth, and genitals burn. This isn’t an allergic reaction you can treat with antihistamines. This is a full-thickness skin death. And it demands immediate hospitalization.
Doctors see SJS and TEN as points on the same spectrum. SJS affects less than 10% of your body surface. TEN? More than 30%. Between 10% and 30%, it’s called SJS/TEN overlap. The bigger the area of skin lost, the higher the chance of death. Mortality jumps from 5% in mild SJS to over 30% in severe TEN. Most deaths come from sepsis, organ failure, or internal bleeding-not the rash itself. But the rash is the warning sign.
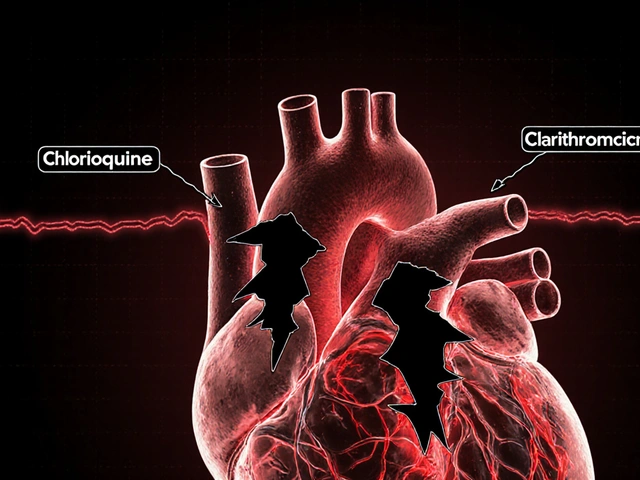
Which Medications Cause These Reactions?
It’s not random. Certain drugs carry a known, documented risk. The biggest culprits? Anticonvulsants like lamotrigine, carbamazepine, phenytoin, and phenobarbital. Antibiotics like sulfamethoxazole (part of Bactrim) and penicillin derivatives. NSAIDs like piroxicam and meloxicam. And allopurinol, the common gout drug. These aren’t obscure drugs-they’re prescribed millions of times a year.
Here’s the catch: you don’t have to be on the drug for long. Most reactions start within the first 8 weeks. Sometimes, they appear even after you’ve stopped taking it-up to two weeks later. That’s why people think they’re safe once they’ve switched medications. They’re not. And if you’ve had SJS or TEN from one drug, you’re at high risk if you take another drug in the same class. Cross-reactivity is real. If lamotrigine caused it, avoid carbamazepine and phenytoin. If sulfamethoxazole triggered it, steer clear of other sulfonamides.
Who’s at Higher Risk?
It’s not just about the drug. Genetics and health history matter. People with HIV or those on chemotherapy have weaker immune systems and face higher risk. So do those who’ve had a previous rash from epilepsy meds-even if it was mild. Taking sodium valproate with lamotrigine increases the chance of a bad reaction. And if someone in your family had SJS or TEN, your risk may be higher. Certain genes, like HLA-B*15:02 in people of Asian descent, are linked to carbamazepine-induced SJS. That’s why some doctors test for it before prescribing.
Children are more likely to get SJS than adults, but adults are more likely to die from it. Why? Because adults often have other health problems-diabetes, kidney disease, heart conditions-that make recovery harder. And older adults are more likely to be on multiple medications, increasing the chance of a dangerous interaction.

What Does It Look Like? Recognizing the Early Signs
Don’t wait for skin to peel. By then, it’s too late. Watch for these early signs:
- High fever (over 101°F)
- Sore throat, burning eyes, or mouth ulcers
- Flu-like fatigue that doesn’t improve
- A red or purplish rash that spreads quickly
- Blisters on skin, lips, or inside the mouth
- Painful skin that feels like it’s burning
The rash doesn’t itch like hives. It hurts. It feels like a bad sunburn that’s turning into raw meat. Blisters burst easily. Skin sloughs off in sheets. Mucous membranes-eyes, mouth, throat, genitals-are almost always involved. If you have blisters in your mouth and a rash on your chest? That’s not a virus. That’s SJS.
Doctors confirm it with a skin biopsy. Under the microscope, they see full-thickness epidermal necrosis-dead skin layers peeling away from the body. No inflammation. No infection. Just death of the outer skin layer. That’s the hallmark.
What Happens in the Hospital?
There’s no magic pill. Treatment is supportive care-like treating a major burn. You’ll be moved to a burn unit or ICU. IV fluids, pain control, and wound care are critical. Your skin is exposed. Infection is the biggest threat. Antibiotics aren’t used unless there’s clear infection-they don’t prevent it. Steroids and immunoglobulins are sometimes tried, but studies show mixed results. The most important step? Stop the drug immediately. No exceptions.
Eye care is urgent. The cornea can scar permanently. You’ll need daily eye drops, sometimes surgery. Mouth sores make eating impossible. Nutrition often comes through a feeding tube. Genital ulcers can cause scarring and narrowing-leading to lifelong problems with urination or intercourse. Nail loss is common. Hair may thin out. Recovery takes weeks to months. And even after healing, complications can last years.
Long-Term Damage: It Doesn’t End When You Leave the Hospital
Survivors aren’t just lucky-they’re burdened. Up to half of people who survive SJS/TEN develop serious eye problems: dry eyes, light sensitivity, scarring, even blindness. Oral complications mean chronic dry mouth, gum disease, and difficulty swallowing. Some develop esophageal strictures-narrowing that makes eating solid food painful. Women may face vaginal stenosis. Men may get phimosis. Nails grow back slowly, if at all. Skin can be permanently scarred or discolored.
These aren’t rare side effects. They’re expected outcomes. That’s why survivors need long-term follow-up: dermatologists, ophthalmologists, dentists, and gynecologists or urologists. One study found that 30-50% of survivors had lasting vision damage. That’s not a small number. That’s nearly half.

How to Prevent It
Prevention starts with awareness. If you’re prescribed lamotrigine, carbamazepine, allopurinol, or sulfamethoxazole, know the signs. Don’t ignore a rash. Don’t wait to see if it gets better. If you get a fever and rash within the first 8 weeks of starting a new drug, go to the ER. Don’t call your doctor. Don’t wait for an appointment. Go now.
For lamotrigine users: never restart the drug after stopping it-even for a few days-without slowly increasing the dose again. Rapid dose increases are a known trigger. Avoid new foods or supplements in the first 3 months. They can confuse symptoms. If you’ve had a rash from any epilepsy drug before, tell your doctor before taking any new one.
Genetic testing isn’t routine, but if you’re of Asian descent and your doctor plans to prescribe carbamazepine, ask about HLA-B*15:02 screening. It’s simple, cheap, and can prevent death.
What to Do If You Suspect SJS or TEN
Stop the medication. Immediately. Then get to the nearest emergency room. Tell them: “I think I have Stevens-Johnson Syndrome.” Don’t say “I have a rash.” Say the name. It matters. Emergency staff need to recognize this fast. The sooner you’re in a burn unit, the better your chance of survival.
Bring a list of all your medications-prescription, over-the-counter, supplements. Even one pill you took a week ago could be the trigger. Don’t assume it’s harmless. Write down when you started each drug and when symptoms began. That timeline helps doctors pinpoint the cause.
And if you survive? Never take the drug again. Or any similar one. Keep a medical alert bracelet. Tell every doctor you see. SJS/TEN is a lifelong warning sign.
Final Reality Check
Yes, SJS and TEN are rare. The risk is less than five cases per million users per week. But rarity doesn’t mean safety. It means unpredictability. One person out of a million might react. But if it’s you? It’s 100%. And the consequences are devastating. There’s no second chance. No do-over. No waiting to see if it clears up.
Medications save lives. But they can also kill-quietly, fast, and without warning. The key isn’t avoiding all drugs. It’s knowing which ones carry this hidden risk. Recognizing the early signs. Acting immediately. And never underestimating a rash that won’t go away.




Maria Elisha
8 December 2025 - 11:51 AM
I took lamotrigine for a year and never had an issue, but now I’m terrified to even look at a pill bottle. Like, seriously, one rash and you’re done? 😩
Angela R. Cartes
9 December 2025 - 09:44 AM
Honestly, if you’re on anticonvulsants and you didn’t get HLA-B*15:02 tested, you’re just gambling with your skin. 🤷♀️ Like, come on. This isn’t 2005 anymore.
Andrea Beilstein
9 December 2025 - 12:00 PM
We treat medicine like it’s a magic spell you cast once and forget about... but the body remembers. Skin isn’t just a covering-it’s a map of our internal state. When it peels... it’s screaming. We ignore the scream until it’s too late. And then we blame the drug. Not the system. Not the rush to prescribe. Not the lack of education. Just the pill.
Lisa Whitesel
9 December 2025 - 19:17 PM
People think they’re safe because they’re ‘only taking it for a week.’ No. You’re not. You’re playing Russian roulette with your epidermis. If you’re not willing to learn the signs, don’t take the meds. Simple. No sympathy for the careless.
Larry Lieberman
10 December 2025 - 16:18 PM
I had a cousin who got TEN from allopurinol. She was 34. Lost 60% of her skin. Spent 3 months in ICU. Now she can’t open her eyes without drops. And her doc never warned her. 🥲
Sabrina Thurn
10 December 2025 - 18:53 PM
The clinical distinction between SJS and TEN is useful for prognostication, but from a patient experience standpoint, it’s all a catastrophic immune-mediated keratinocyte apoptosis cascade. The key intervention is immediate withdrawal of the inciting agent and transfer to a burn center with multidisciplinary support-dermatology, ophthalmology, critical care. Delay = higher mortality. Period.
Courtney Black
11 December 2025 - 00:21 AM
I used to think allergies were just sneezing and itchy eyes. Then I saw a friend’s face melt. Not literally. But close enough. Skin falling off like wet paper. Mouth full of blood. No one told her it could happen. No one told her to go to the ER. She just thought it was a bad reaction. And then she was in a coma. And now she can’t smile right. I don’t take anything without checking.
iswarya bala
12 December 2025 - 11:13 AM
i took sulfamethoxazole for a UTI and got a rash... i thought it was just heat... i didnt know it could be this bad... thank u for sharing this... i will never ignore a rash again
Ryan Brady
13 December 2025 - 01:03 AM
Why do we let big pharma push these death pills? They know. They’ve known for decades. They just don’t care until someone dies. Then they slap a black box on it and keep selling. America’s healthcare system is a death factory.
Raja Herbal
14 December 2025 - 15:14 PM
So… you’re telling me the same drug that cures gout can also turn your skin into confetti? And the only warning is ‘maybe don’t take it if you’re Asian’? 😏 Guess I’ll just stop taking all meds and eat turmeric instead.
Lola Bchoudi
14 December 2025 - 20:14 PM
If you’re prescribed lamotrigine or allopurinol, please do not skip the education session. Ask for the handout. Watch the video. Print the symptoms list. Stick it on your fridge. Your life depends on noticing the difference between ‘a little red’ and ‘burning, spreading, blistering.’ You’ve got this.
Morgan Tait
16 December 2025 - 08:20 AM
Did you know the FDA has been quietly pressured by drug manufacturers to delay black box warnings? The real cause of SJS isn’t the drug-it’s the corporate cover-up. And the HLA-B*15:02 test? It’s not offered in 80% of US clinics because insurance won’t pay. This isn’t medicine. It’s profit-driven negligence.
Darcie Streeter-Oxland
17 December 2025 - 14:05 PM
It is imperative that healthcare professionals ensure that patients are adequately informed of the potential for severe cutaneous adverse reactions when initiating therapy with agents such as anticonvulsants, sulfonamides, and allopurinol. The absence of documented patient education constitutes a significant clinical oversight.
Steve Sullivan
18 December 2025 - 17:49 PM
i got the hla test before my doc gave me carbamazepine. i’m south asian. test came back positive. he switched me to valproate. i’m alive. my sister died from TEN from the same drug. don’t wait. ask. test. live. 🙏