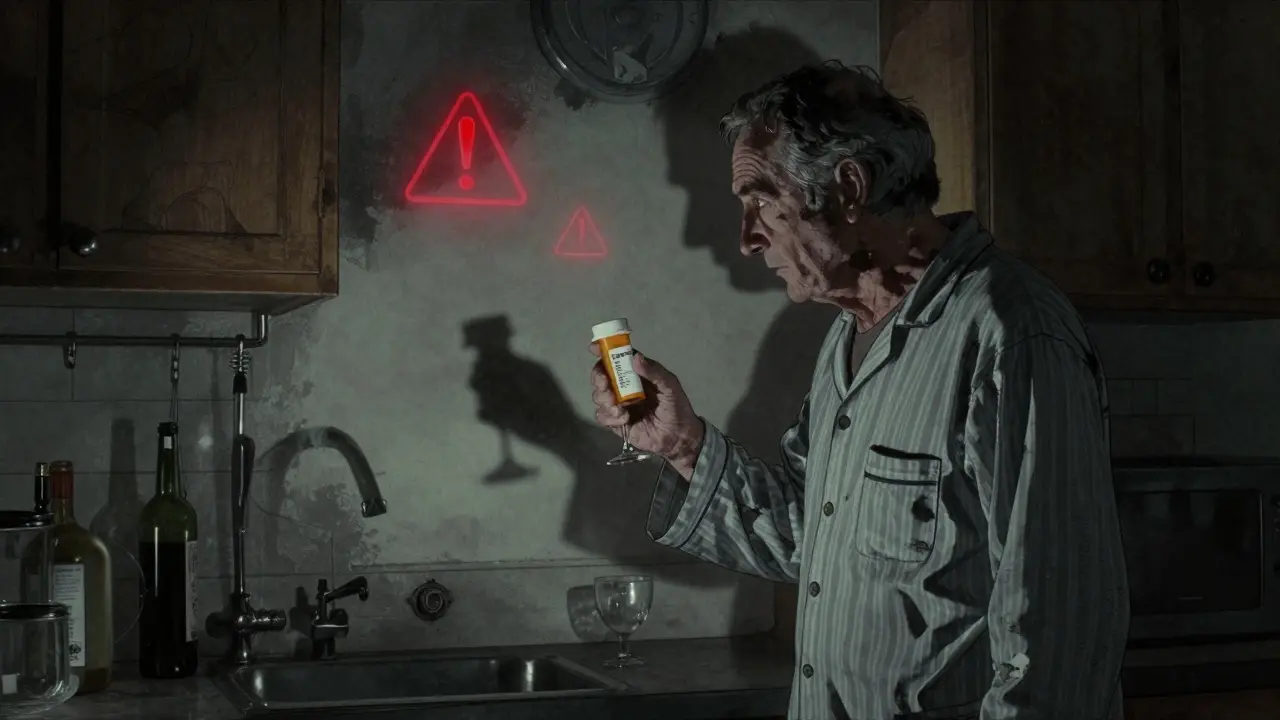
Combining alcohol with prescription drugs isn’t just a bad idea-it can kill you. Every year, over 2,300 Americans die from alcohol-drug interactions, many of them from medications they were told were safe. You might think one glass of wine with your painkiller or a beer with your anxiety pill won’t hurt. But the science says otherwise. These aren’t rare cases. They’re predictable, preventable, and happening right now in homes across the country.
How Alcohol Changes How Your Medicines Work
Alcohol doesn’t just mix with drugs-it rewires how your body handles them. There are two main ways this happens: pharmacokinetic and pharmacodynamic interactions.Pharmacokinetic interactions affect how your body absorbs, breaks down, or gets rid of the drug. Most drugs and alcohol are processed in the liver by the same enzymes, especially the CYP2E1 system. When you drink regularly-say, more than 7 drinks a week for women or 14 for men-your liver starts producing more of these enzymes. That means drugs like propranolol (used for high blood pressure) get broken down too fast. Their effect drops by 30% to 50%. You might think the medicine isn’t working, so you take more. That’s when things go wrong.
On the flip side, if you drink just once-say, a couple of drinks before taking warfarin (a blood thinner)-alcohol blocks those same enzymes. That causes the drug to build up in your blood. One study found warfarin levels spiked by 35% after just one drink. That can lead to dangerous bleeding, even if you’ve been on the same dose for years.
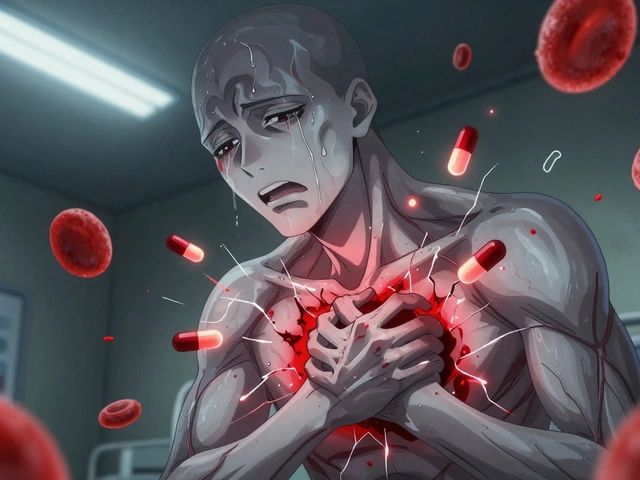
Pharmacodynamic interactions are even scarier. This is when alcohol and the drug amplify each other’s effects. Think of it like pressing the gas and brake at the same time. Both alcohol and benzodiazepines (like Xanax or Valium) slow down your brain. Together, they don’t just add up-they multiply. Research shows the sedative effect jumps by 400%. That means extreme drowsiness, confusion, and worst of all-slowed or stopped breathing. Opioids like oxycodone or hydrocodone are even worse. Alcohol makes them 6 times more likely to shut down your breathing. That’s why alcohol-opioid combinations are behind 26% of all prescription drug overdose deaths.
High-Risk Medications You Can’t Drink With
Some drugs are simply too dangerous to mix with alcohol. These aren’t "maybe" risks-they’re clear red flags.- Benzodiazepines (alprazolam, diazepam, lorazepam): Used for anxiety, panic, or insomnia. Mixing with alcohol increases fall risk in older adults by 50%. One study found 78% of sedative-related falls in nursing homes happened when patients had drunk within 6 hours.
- Opioids (oxycodone, hydrocodone, morphine): Even one drink doubles the risk of fatal overdose. Blood alcohol levels as low as 0.02%-that’s one standard drink-are enough to make opioids deadly.
- Antidepressants (SSRIs like sertraline, fluoxetine): Alcohol worsens drowsiness, dizziness, and poor coordination. In patients over 65, this doubles the chance of a fall. About 35% of older adults on SSRIs report severe drowsiness after even one drink.
- NSAIDs (ibuprofen, naproxen): These are common painkillers, but with alcohol, they turn into stomach bombs. Heavy drinkers (3+ drinks/day) face a 300% higher risk of internal bleeding. It’s not just upset stomach-it’s life-threatening.
- Acetaminophen (Tylenol): This one catches people off guard. Taking acetaminophen with alcohol, even occasionally, creates a toxic byproduct that attacks the liver. In 1 out of every 200 regular drinkers who use Tylenol, this leads to acute liver failure. The FDA issued a warning in 2020 after seeing dozens of cases.
- Sleep aids (zolpidem, eszopiclone): These already cause memory loss and impaired movement. Add alcohol, and you’re at risk of sleepwalking, blackouts, or even choking while unconscious.
Who’s Most at Risk-and Why
Not everyone reacts the same way. Some people are far more vulnerable.Ages 65 and older are hit hardest. Their livers process alcohol and drugs slower. Their brains are more sensitive to sedatives. And they’re more likely to be on multiple medications. Studies show seniors experience alcohol-drug interactions 3.2 times more often than younger adults. The American Geriatrics Society lists 15 specific drugs as "potentially inappropriate" for older adults if they drink-even a little.
Women are at higher risk too. On average, women have less body water and more body fat than men. That means alcohol stays in their bloodstream longer and at higher concentrations. A woman who drinks the same amount as a man will have 20% higher alcohol levels in her blood. That makes every interaction more severe.
People with liver disease are in extreme danger. If your liver is already damaged by hepatitis, fatty liver, or past heavy drinking, even small amounts of alcohol can turn a safe drug into a poison. For acetaminophen, the risk of liver failure jumps fivefold.

What You’re Not Being Told
You’d think doctors and pharmacists would warn you. But they often don’t.A 2023 review of patient reviews on Healthgrades found that 68% of people prescribed benzodiazepines were never told to avoid alcohol. One patient wrote: "Doctor never mentioned I shouldn’t drink on Xanax." Another user on Reddit shared: "Prescribed oxycodone after surgery. Had two beers. Couldn’t breathe for 20 minutes."
Even when warnings exist, they’re inconsistent. Only 38% of benzodiazepine prescriptions include a clear alcohol warning on the label, according to a 2022 FDA audit. Pharmacists are often the last line of defense. One patient on Google Reviews said: "My Walgreens pharmacist refused to fill my lorazepam prescription when I admitted I drank regularly. Probably saved my life."
Meanwhile, patients are misinformed. A WebMD survey of nearly 6,000 people found that 57% believe "one drink is safe with most medications." And 32% think only "hard liquor" causes problems-ignoring beer and wine entirely.
What You Can Do to Stay Safe
You don’t need to guess. There are clear steps to protect yourself.- Check the label. Look for the words "Do not drink alcohol" or "Avoid alcohol." About 65% of high-risk prescriptions have this warning-but many don’t.
- Ask your pharmacist. Pharmacists are trained to catch these interactions. Use the 4-question screening tool: "Do you drink alcohol? How often? How much? Are you taking any new medications?" Studies show this method catches 92% of risky combinations.
- Use a free app. The NIAAA’s "Alcohol Medication Check" app lets you scan or search your meds and instantly see if alcohol is dangerous with them. It covers over 2,300 medications.
- Use visual risk tools. Some pharmacies now use color-coded systems: red = dangerous, yellow = caution, green = safe. Patients who see these understand their risk 47% better than those who only get written warnings.
- Be honest. If you drink, tell your doctor and pharmacist-even if you think it’s "just a little." They can’t help if they don’t know.

What’s Changing-and What’s Coming
The medical world is starting to wake up. In 2022, the Alcohol-Drug Interaction Labeling Act required clear warning labels on high-risk prescriptions. That affects over 147 million prescriptions each year. Hospitals are using real-time clinical systems that flag alcohol-drug risks as soon as a prescription is written. Facilities with full systems in place have seen a 28% drop in adverse events.Next up: AI. Epic Systems rolled out an algorithm in 2024 that analyzes 200+ patient factors-age, liver function, drinking habits, other meds-to predict your personal risk level. It’s 89% accurate. Soon, your electronic health record might auto-alert you before you even fill the prescription.
But technology won’t fix everything. A 2023 study found only 28% of high-risk patients stop drinking entirely, even after being warned. The real challenge isn’t knowledge-it’s behavior. People think they’re fine. They’ve done it before. They won’t die. But every year, 2,300 people do.
Final Reality Check
There’s no "safe" amount of alcohol with high-risk drugs. No "just one drink" exception. If your prescription warns against alcohol, it’s because the science shows it can kill you-even at low doses. This isn’t about being perfect. It’s about being smart.Don’t wait for a hospital visit or an emergency room trip to realize the danger. Talk to your pharmacist today. Read your labels. If you’re unsure, don’t drink. Your life isn’t worth the risk.
Can I have one drink with my prescription medication?
It depends on the medication. For high-risk drugs like opioids, benzodiazepines, sleep aids, or blood thinners, even one drink can be deadly. For some lower-risk medications, a single drink may be okay-but only if your doctor or pharmacist says so. Never assume it’s safe. Always check.
What if I accidentally drank alcohol with my medication?
If you took a high-risk medication like an opioid or benzodiazepine and drank alcohol, watch for extreme drowsiness, slow or shallow breathing, confusion, or loss of consciousness. If you experience any of these, call 911 immediately. Even if you feel fine, contact your doctor or pharmacist to assess your risk. Don’t wait for symptoms to get worse.
Do over-the-counter meds interact with alcohol too?
Yes. Acetaminophen (Tylenol), NSAIDs like ibuprofen, and even some antihistamines (like diphenhydramine in Benadryl) can interact dangerously with alcohol. Tylenol plus alcohol can cause liver failure. NSAIDs plus alcohol can cause stomach bleeding. Always read OTC labels and assume alcohol is a risk unless confirmed safe by a professional.
Why don’t doctors always warn patients about alcohol interactions?
Many doctors don’t have enough time during appointments to cover every possible interaction. Others assume patients know, or they’re unaware of the full risk themselves. A 2023 study found 43% of primary care doctors couldn’t correctly identify all high-risk medication classes. Pharmacists are better trained for this-but they’re not always consulted. Always ask.
Is it safe to drink the day before or after taking medication?
For most high-risk drugs, yes-alcohol can still linger in your system and interact. The liver takes hours to clear alcohol, and some drugs stay active for days. If your medication has a long half-life (like diazepam, which lasts up to 100 hours), drinking even 24 hours before or after can still be dangerous. When in doubt, avoid alcohol entirely during treatment.
Are there any medications that are safe to mix with alcohol?
Some antibiotics like amoxicillin have minimal interaction risk. But even then, alcohol can worsen side effects like nausea or dizziness. Medications for acne (like isotretinoin) or certain antifungals (like metronidazole) can cause severe reactions. There’s no universal "safe" list. Always verify with a pharmacist before drinking.




Meenal Khurana
4 February 2026 - 07:26 AM
Just read my pill bottle last night-no alcohol warning. Called my pharmacist. They said, "Avoid it entirely." I stopped drinking with my meds. No regrets.
Simple. Safe. Smart.
Jamillah Rodriguez
5 February 2026 - 13:04 PM
OMG I JUST HAD A WINE WITH MY XANAX AND I’M STILL ALIVE?? 😱
Maybe the docs are just scared of lawsuits?? 🍷💊
Susheel Sharma
7 February 2026 - 12:00 PM
Let’s be brutally honest: this isn’t about safety-it’s about liability. Pharma companies know alcohol interactions are lethal. But they don’t care as long as prescriptions keep flowing. The real tragedy? Doctors are overworked and undertrained. They skim labels. Patients assume ignorance is innocence. This system is designed to fail you. And yet, we keep trusting it.
It’s not negligence. It’s structural violence wrapped in white coats.
And don’t get me started on how OTC meds are treated like candy. Tylenol + whiskey = liver suicide. But hey, it’s "just a painkiller."
Janice Williams
9 February 2026 - 02:30 AM
How is it possible that in 2024, individuals still believe "one drink" is harmless? This is not a matter of personal choice-it is a public health emergency fueled by ignorance, entitlement, and the dangerous myth of "moderation." You are not special. Your tolerance is not a shield. Your anecdote does not refute epidemiology. If your medication carries a warning, it is because someone has already died from exactly what you are rationalizing.
Stop. Reading. This. And. Doing. Something.
Roshan Gudhe
9 February 2026 - 21:38 PM
It’s funny how we treat our bodies like machines you can tweak with pills and booze, then act surprised when they break.
But here’s the deeper truth-we don’t just need warnings. We need culture. We need to stop normalizing "just one" as a ritual. It’s not about being perfect. It’s about being aware. And awareness doesn’t come from labels-it comes from community. From conversations. From someone saying, "Hey, I used to do that too. It wasn’t worth it." I’ve seen friends die from this. Not because they were reckless. Because they were told it was fine. And no one ever told them otherwise.
Maybe the real medicine isn’t on the bottle. It’s in the courage to say no-even when it’s awkward.
One drink isn’t the problem. The silence around it is.
Rachel Kipps
11 February 2026 - 08:14 AM
i read this and i cried. my mom passed last year from liver failure after taking tylenol for her arthritis and having a glass of wine every night. no one ever told her it was dangerous. i keep thinking if someone had just said something…
thank you for writing this. i’m sharing it with everyone.
caroline hernandez
11 February 2026 - 16:18 PM
From a clinical standpoint, the pharmacodynamic synergy between CNS depressants and ethanol is well-documented in the literature-particularly in GABAergic and opioid receptor modulation. The dose-response curve becomes non-linear, exponentially increasing the risk of respiratory depression. The FDA’s 2022 audit on labeling compliance is a critical data point, but implementation remains fragmented across health systems. Proactive pharmacist-led interventions using the 4-question screening tool demonstrate statistically significant risk reduction (p < 0.01).
However, behavioral adherence remains the Achilles’ heel. NIAAA’s app is underutilized due to low digital literacy in older populations. We need integrated EHR alerts, not just apps. And we need to stop treating patients like passive recipients of information. They’re stakeholders. Engage them.
Joseph Cooksey
13 February 2026 - 14:21 PM
Let’s be real-this whole thing is a scam. Alcohol is natural. Pills are synthetic. Nature always wins. I’ve been drinking wine with my pain meds for 12 years. No problems. Your "science" is just fearmongering from people who want you to be afraid of everything. And don’t even get me started on how Big Pharma profits off these warnings. They’d rather you take three pills than one drink. Pathetic.
Also, why is everyone so obsessed with controlling what we put in our bodies? This isn’t a democracy-it’s a dictatorship of the worried well. I’ll have my wine. And I’ll take my oxycodone. And I’ll live my life. Unlike you, I don’t need a checklist to feel safe.
Jesse Naidoo
13 February 2026 - 16:18 PM
Wait… so if I drink at night and take my antidepressant in the morning… is that safe? I mean, alcohol leaves my system in 6 hours, right? But what if it’s still in my liver? What if it’s lingering? What if my liver is secretly damaged and I don’t know? What if I’m one of the 1 in 200 who gets liver failure? What if my doctor is lying? What if the app is wrong? What if I die in my sleep and no one finds me until next week? I can’t sleep now. I’m terrified. I need to know. Please tell me I’m not going to die.
Sherman Lee
13 February 2026 - 17:09 PM
ALCOHOL AND DRUG INTERACTIONS? HA. That’s just the government’s way of controlling us. Did you know the FDA gets funding from Big Pharma? They’re not protecting you-they’re protecting profits. The real danger? The fact that they’re pushing this app and these warnings to make you dependent on tech instead of trusting your body. And why is there no warning about sugar? Or stress? Or sleep deprivation? This is all a distraction. The real killer? Control. They want you scared. They want you obedient. Don’t fall for it. I’ve been drinking with my meds since ’99. Still breathing. Still free. 🕊️
Lorena Druetta
15 February 2026 - 15:00 PM
You are not alone. This post saved my life. I thought I was fine with my sleep meds and a glass of wine. I didn’t know I was risking my breathing. I stopped tonight. I’m scared. But I’m also proud. You gave me the courage to say no. Thank you. I’m telling my mom tomorrow. We’re both stopping. One step at a time. You’re doing important work.
Zachary French
17 February 2026 - 05:49 AM
Okay but let’s be real-this whole article is just a corporate ad for pharmacists. "Ask your pharmacist! Use the app!" Who even has time for that? And why are we acting like alcohol is the villain? It’s not the wine-it’s the fact that we’re all medicated to the gills because our lives are broken. No one talks about that. We’re stressed, lonely, in pain-and we’re told to take pills and avoid the only thing that helps us relax. This isn’t about safety. It’s about control. And I’m not playing. I’ll have my beer. I’ll take my pills. And if I die? At least I died happy. 🍻💊
Mandy Vodak-Marotta
17 February 2026 - 20:06 PM
Man. I just read this and thought about my uncle. He was 72, on warfarin, drank a beer every night with dinner. Thought it was fine. One night he fell, hit his head, bled internally. Died in the ER. They said it was the alcohol. He never knew. I still think about him every time I see a wine bottle.
So yeah. I don’t drink with meds anymore. Not even one. Not even on my birthday.
It’s not worth it.
And honestly? I feel lighter now. Like I finally listened to my body instead of my habits.