When your back hurts, your head throbs, or your knees ache after a long day, you reach for the medicine cabinet. But which pill should you grab-ibuprofen, naproxen, or Tylenol? It’s not just about what’s on the shelf. The difference between NSAIDs and acetaminophen isn’t just brand names. It’s about how your body reacts, what’s causing the pain, and how to avoid serious side effects you might not even know about.
How They Work (And Why It Matters)
| Medication Type | How It Works | Does It Reduce Swelling? |
|---|---|---|
| NSAIDs (ibuprofen, naproxen, aspirin) | Block COX enzymes throughout the body, reducing prostaglandins that cause pain, fever, and inflammation. | Yes |
| Acetaminophen (Tylenol) | Mainly affects pain signals in the brain and spinal cord. Exact mechanism still not fully understood. | No |
Acetaminophen? It’s quieter. It doesn’t touch inflammation at all. It just turns down the volume on pain signals heading to your brain. That’s why it’s great for headaches or a fever from a cold-but useless if your pain comes from swelling.
When to Choose NSAIDs
If your pain comes with redness, heat, or swelling, NSAIDs are usually the better pick. That includes:
- Arthritis pain in knees, hips, or hands
- Back or neck pain from muscle strain or disc issues
- Menstrual cramps
- Sprains, bruises, or tendonitis
Studies show NSAIDs work better than acetaminophen for osteoarthritis pain. One analysis from the Hospital for Special Surgery found that people with knee or hip arthritis got significantly more relief from ibuprofen than from Tylenol alone.
But here’s the catch: NSAIDs can hurt your stomach. About 1 in 5 regular users get upset stomach, ulcers, or bleeding. The risk goes up if you’re over 60, take blood thinners, or use them for weeks at a time. They also raise your chance of heart attack or stroke-especially if you already have heart disease. The FDA has required black box warnings on all NSAIDs since 2005 for this reason.
When to Choose Acetaminophen
Acetaminophen is the go-to for pain without inflammation:
- Headaches and migraines
- Fever from colds or flu
- Toothaches or minor injuries
- Pain if you can’t take NSAIDs (due to stomach issues or heart risks)
It’s easier on the stomach. No irritation. No bleeding risk. That’s why doctors often recommend it for people with ulcers, high blood pressure, or kidney problems.
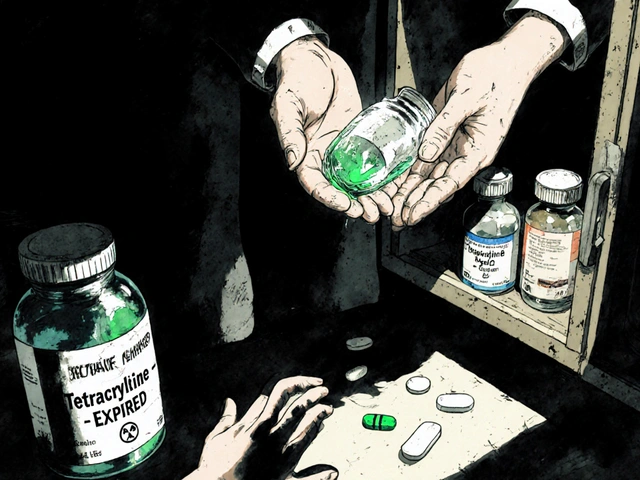
But there’s a dark side: your liver.
Take more than 4,000 milligrams in a day-just eight extra-strength Tylenol tablets-and you risk serious liver damage. The FDA says over 56,000 ER visits each year are from acetaminophen overdoses. Many people don’t realize they’re doubling up. Cold medicines, sleep aids, and prescription painkillers like Vicodin all contain acetaminophen. You can easily hit the limit without meaning to.

Who Should Avoid Each One
Not everyone can safely use either drug.
Avoid NSAIDs if you:
- Have a history of stomach ulcers or bleeding
- Have heart disease, high blood pressure, or kidney disease
- Take blood thinners like warfarin (NSAIDs can interfere with them)
- Are pregnant in the third trimester (they can affect fetal circulation)
Avoid acetaminophen if you:
- Drink alcohol regularly (even 2-3 drinks a day increases liver risk)
- Have liver disease like hepatitis or cirrhosis
- Take multiple medications that contain acetaminophen
Some people think acetaminophen is "safer" because it doesn’t hurt the stomach. That’s true-but it’s not safer overall. It just trades one risk for another.
Can You Take Them Together?
Yes-and many doctors recommend it.
Research from the Mayo Clinic and Hospital for Special Surgery shows that combining acetaminophen with a low-dose NSAID can give you better pain relief than either one alone. You can use less of each, lowering your risk of side effects.
Here’s a common schedule used by pain specialists:
- 8 AM: 500 mg acetaminophen
- 2 PM: 200 mg ibuprofen
- 8 PM: 500 mg acetaminophen
- 10 PM: 200 mg ibuprofen
This keeps pain under control without pushing either drug to its limit. But never combine them without checking with your doctor, especially if you have liver or kidney issues.
Dosage Rules You Can’t Ignore
Over-the-counter doesn’t mean "take as much as you want."
Acetaminophen:
- Standard dose: 325-650 mg every 4-6 hours
- Max daily: 3,000 mg (safer) or 4,000 mg (absolute limit)
- Extra-strength tablets: 500 mg each → max 6 per day
NSAIDs:
- Ibuprofen (Advil, Motrin): 200 mg every 4-6 hours → max 1,200 mg/day (OTC)
- Naproxen (Aleve): 220 mg every 8-12 hours → max 660 mg/day (OTC)
- Aspirin: 325-650 mg every 4-6 hours → max 4,000 mg/day (but rarely used for pain anymore)
Always read labels. Many cold and flu products include acetaminophen or ibuprofen. Don’t stack them.

What the Experts Say
Doctors don’t pick one over the other blindly. They ask: What’s causing the pain?
Dr. Kramskiy from the Hospital for Special Surgery says: "Tylenol works best as part of a team. It’s not the star-it’s the supporting actor." He often pairs it with NSAIDs for arthritis patients.
Harvard Health says: "If you’re unsure, start with acetaminophen. If it doesn’t help after a few days, try an NSAID. But don’t switch back and forth without knowing why."
The American Academy of Family Physicians reminds us: "This advice is for healthy adults using pain relievers occasionally." If you’re taking pain meds daily, you need a plan-not just a bottle.
Real-World Tips
- For a headache or fever? Start with acetaminophen.
- For a swollen knee or sore back? Try ibuprofen.
- Don’t take NSAIDs on an empty stomach. Eat something first.
- Keep a pain journal: note what you took, when, and how much relief you got.
- If you drink alcohol, stick to acetaminophen-but keep your daily dose under 2,000 mg.
- If you’re on blood thinners, acetaminophen is usually safer.
- Never mix NSAIDs with aspirin for heart protection. Ibuprofen can block aspirin’s benefits.
And remember: pain is a signal. If you need pain relievers for more than 10 days straight, see a doctor. You might be treating the symptom, not the cause.
Can I take ibuprofen and Tylenol together?
Yes, you can safely take ibuprofen and acetaminophen together, as long as you stay within the daily limits for each. Many doctors recommend this combination because it gives better pain control with lower doses of each drug, reducing the risk of side effects. For example, take 500 mg of acetaminophen at 8 AM and 200 mg of ibuprofen at 2 PM, then repeat in the evening. Always check other medications you’re taking to avoid accidental overdose.
Which is better for back pain: NSAIDs or acetaminophen?
NSAIDs like ibuprofen are usually better for back pain because most back pain involves inflammation-from muscle strains, disc issues, or arthritis. Acetaminophen may help with the pain, but it won’t reduce the swelling causing it. Studies show NSAIDs provide more relief for inflammatory back pain. If you can’t take NSAIDs due to stomach or heart issues, acetaminophen is a backup, but you may need a higher dose or other treatments.
Is Tylenol safer than ibuprofen?
It depends on your health. Tylenol is safer for your stomach and heart, but it’s harder on your liver. Ibuprofen is safer for your liver but can cause stomach bleeding and raise your risk of heart attack or stroke. If you have liver disease or drink alcohol, Tylenol isn’t safe. If you have high blood pressure or kidney disease, ibuprofen may not be safe. Neither is universally safer-it’s about matching the drug to your body’s risks.
Why do some cold medicines have acetaminophen?
Acetaminophen is added to cold and flu medicines because it reduces fever and eases headaches and body aches-common symptoms of illness. But this creates a hidden risk: if you take Tylenol separately on top of a cold medicine that already contains acetaminophen, you can easily overdose. Always check the "Active Ingredients" section on the label. If it says "acetaminophen," don’t take extra Tylenol.
Can I use NSAIDs for a headache?
Yes, NSAIDs like ibuprofen and naproxen can help with headaches, including migraines. In fact, they’re often more effective than acetaminophen for migraine pain. But if you get frequent headaches, NSAIDs can cause rebound headaches if used too often. Acetaminophen is gentler for occasional headaches, especially if you have stomach sensitivity. If you’re not sure, try acetaminophen first. If it doesn’t work after a couple of doses, switch to an NSAID.
What’s the safest long-term pain reliever?
There’s no perfect long-term pain reliever. Both NSAIDs and acetaminophen carry risks with daily use. For chronic pain, the safest approach is using the lowest effective dose, rotating medications, and combining them with non-drug treatments like physical therapy, heat, or stretching. If you need daily pain relief, talk to your doctor. You may need a different strategy-like physical therapy, nerve blocks, or low-dose antidepressants-that doesn’t rely on OTC pills.
Final Thought: Pain Is Personal
There’s no one-size-fits-all answer. What works for your neighbor might not work for you. Some people feel relief with Tylenol. Others need the anti-inflammatory punch of ibuprofen. The key is knowing why you’re in pain-and what your body can handle.
Start low. Watch for side effects. Don’t mix medications blindly. And if pain sticks around longer than a week or two, don’t just reach for the bottle-see a doctor. You’re not just treating pain. You’re protecting your body.




kabir das
29 January 2026 - 14:39 PM
Wait, so you're telling me I've been taking Tylenol for my back pain like a fool?? I thought it was just "milder"-turns out it's just useless against inflammation?? My knees have been screaming for months and I've been babying them with acetaminophen like it's a spa day... 😭
Laura Arnal
31 January 2026 - 10:40 AM
OMG YES!! I switched from ibuprofen to Tylenol after my stomach started rebelling, and honestly? My headaches vanished. I used to think NSAIDs were the "stronger" option, but now I know it’s about matching the drug to the pain. 🙌 Also-READ THE LABELS ON COLD MEDS. I once took 3 Tylenol + NyQuil and nearly ended up in the ER. Don’t be me. 😅
Eli In
31 January 2026 - 14:22 PM
I’m from India and we’ve got this weird cultural thing where everyone just pops painkillers like candy. My grandma takes ibuprofen for her arthritis, but she also drinks 3 glasses of whiskey a day. 🤯 I told her "Aunty, Tylenol is your friend," and she said, "Beta, if it doesn’t burn my stomach, it’s not working." We need more public education on this stuff. 🌏💊
Ryan Pagan
2 February 2026 - 05:29 AM
Let’s cut the fluff: NSAIDs are the MVP for inflammatory pain. Full stop. Acetaminophen? It’s the quiet cousin who shows up to Thanksgiving but never talks. You want swelling gone? NSAIDs. You want to feel like your brain isn’t in a vice? Tylenol. But here’s the kicker-most people don’t realize they’re stacking meds like a Jenga tower. I’ve seen patients take Advil, Excedrin, and a cold tablet all at once. And then they wonder why their liver looks like a burnt pancake. 🚨 Don’t be that person. Know your labels. Know your limits.
Paul Adler
2 February 2026 - 15:56 PM
While the article provides a comprehensive overview, it is worth noting that individual variability in drug metabolism plays a significant role in efficacy and risk. Genetic polymorphisms in CYP450 enzymes, particularly CYP2E1 and CYP3A4, influence acetaminophen detoxification pathways. Similarly, COX-1 and COX-2 isoform expression affects NSAID response. Personalized medicine approaches, though not yet mainstream, may eventually guide safer analgesic selection. For now, cautious, informed use remains the standard.
DHARMAN CHELLANI
3 February 2026 - 23:19 PM
NSAIDs? Pfft. Just use aspirin. It’s cheaper, older, and your grandpa used it. Tylenol? That’s for weaklings who can’t handle a little stomach burn. Also, who even uses naproxen anymore? Everyone’s on ibuprofen. And why are you telling people to eat before taking it? Like, duh. Basic human behavior. 😴
Kacey Yates
5 February 2026 - 08:16 AM
Acetaminophen kills your liver. NSAIDs kill your stomach. Pick your poison. I take both every day and I’m fine. Everyone else is just scared of pills. You think your liver is sacred? It’s a muscle. It handles booze, stress, and bad decisions. Stop acting like a baby. And read the damn label. If you can’t, don’t take anything.
ryan Sifontes
5 February 2026 - 10:35 AM
So NSAIDs cause heart attacks? And Tylenol causes liver failure? And the government knows this? And they still sell it? And we’re supposed to trust this? I’m starting to think the real pain is the system. Maybe the answer isn’t pills. Maybe it’s… silence. Or fasting. Or moving to a cabin in the woods. I’m just saying.
Jasneet Minhas
7 February 2026 - 02:37 AM
How ironic that in a country that worships efficiency, we’ve turned pain relief into a high-stakes math problem. 500mg here, 200mg there. It’s like we’re solving for X in a calculus equation where X is "not dying." Meanwhile, my cousin in Kerala just rubs warm coconut oil on his knee and calls it a day. 🙏 Maybe we’ve overcomplicated this. Or maybe we just like having rules.
Megan Brooks
8 February 2026 - 15:13 PM
There’s an underlying assumption here that pain is purely biological. But pain is also psychological, social, and cultural. For some, the ritual of taking a pill-its texture, its timing, its symbolic act of self-care-is as therapeutic as the pharmacology. To reduce this to a biochemical choice ignores the embodied experience of suffering. We treat symptoms, yes-but we also treat meaning.
Doug Gray
8 February 2026 - 22:24 PM
It’s not about NSAIDs vs. acetaminophen. It’s about the epistemological rupture between biomedical reductionism and phenomenological experience. The COX enzyme is a proxy, not a truth. The liver is a metaphor for systemic fragility. We are not molecules-we are narratives. And yet, we’ve outsourced our suffering to a pill. What have we become?
Kristie Horst
9 February 2026 - 00:11 AM
Oh, so now we’re recommending combining drugs like they’re cocktail ingredients? How thoughtful. Let’s just throw acetaminophen and ibuprofen together and call it a "synergistic pain management strategy." Meanwhile, the average person can’t tell the difference between a 500mg tablet and a 325mg tablet. This isn’t medicine. It’s a liability waiting to happen. And now we’re handing out schedules like they’re yoga routines. 🤦♀️
LOUIS YOUANES
9 February 2026 - 09:53 AM
I’ve been taking Tylenol for 15 years. My liver is fine. My stomach is fine. I don’t drink. I don’t take anything else. So your "risks" are just fear-mongering. I don’t need a 2000-word essay to tell me what works for me. I’m not a statistic. I’m a person who feels pain and takes a pill. End of story.
Andy Steenberge
10 February 2026 - 09:15 AM
Great breakdown. One thing missing: hydration. Both NSAIDs and acetaminophen are harder on your kidneys if you’re dehydrated. Drink water. Especially if you’re active or in hot weather. And if you’re taking either daily for more than a week? Get your liver and kidney numbers checked. Simple. Cheap. Smart.
Alex Flores Gomez
12 February 2026 - 08:50 AM
NSAIDs are for people who don’t know how to meditate. Acetaminophen is for people who don’t know how to drink. I just take aspirin and go for a walk. Problem solved. Also, why is everyone so obsessed with pills? We’re not robots. We’re meatbags with feelings. Maybe stop treating pain like a bug to be eradicated and start treating it like feedback.