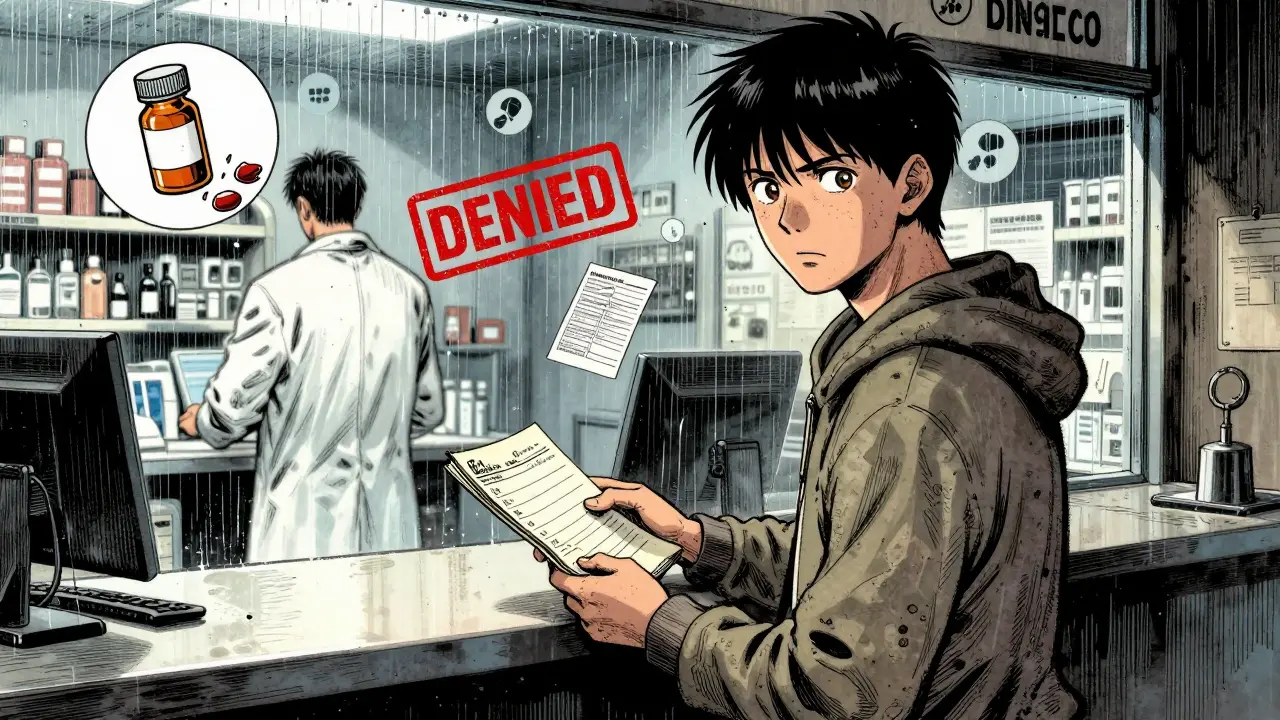
When your doctor prescribes a generic medication and the pharmacy says it’s not covered, it’s not a mistake. It’s a non-formulary generic - a drug that’s FDA-approved, safe, and cheaper than brand names, but your insurance plan simply doesn’t list it. And when that happens, you’re left paying full price - sometimes hundreds of dollars more - or going without. This isn’t rare. In 2022, over 12% of all generic prescriptions were blocked by formulary restrictions. For conditions like Crohn’s disease, diabetes, or epilepsy, that denial can mean real health risks.
Why are some generics not covered?
Insurance plans build formularies to control costs. They pick one or two generics per drug class - usually the cheapest ones - and make those the only covered options. Even if your doctor prescribes a different generic version of the same drug - say, metformin ER made by a different manufacturer - it might not be on the list. That’s not because it’s less effective. It’s because the plan negotiated a better deal with one supplier. The problem? Not all generics work the same for every person. Some people react differently to fillers, binders, or release mechanisms. A switch can mean worse side effects, lower effectiveness, or even dangerous drops in blood sugar or inflammation markers.
What the law says: you have rights
Federal law doesn’t let insurers just say no and walk away. If a drug is medically necessary, you have the right to ask for an exception. This isn’t a suggestion. It’s a requirement under Medicare Part D and most commercial plans. The plan must review your request and respond within 72 hours - or 24 hours if your condition is urgent. You can even get a 72-hour emergency supply while you wait. Many people don’t know this. A GoodRx survey found only 29% of patients knew they could request an urgent review. That’s a gap that costs people their health.
How to get your non-formulary generic approved
Getting coverage isn’t about begging. It’s about proving medical necessity. Here’s how to do it right:
- Get the denial in writing. The pharmacy must give you a formal coverage determination. Don’t take a verbal no. Ask for the form or email.
- Work with your doctor. Your provider must fill out a Coverage Determination Request form. But here’s the key: generic templates won’t cut it. The plan needs specifics. What happened when you tried the formulary alternative? Did your A1c spike? Did your stool calprotectin levels rise? Did you get a rash or dizziness? Document dates, lab values, symptoms. Dr. Jane Sarasohn-Kahn says the most approved requests include clinical proof - not just "this works better for me."
- Submit with evidence. Attach recent lab reports, past prescription records, or even a letter from your specialist. The Crohn’s & Colitis Foundation found that requests with three or more clinical details had approval rates over 70%.
- Ask for an expedited review if needed. If you’re running out of medication or your condition is worsening, call the plan immediately. Say: "I need an expedited review under CMS guidelines for urgent medical need." Keep records of who you spoke to and when.
What happens if you’re denied?
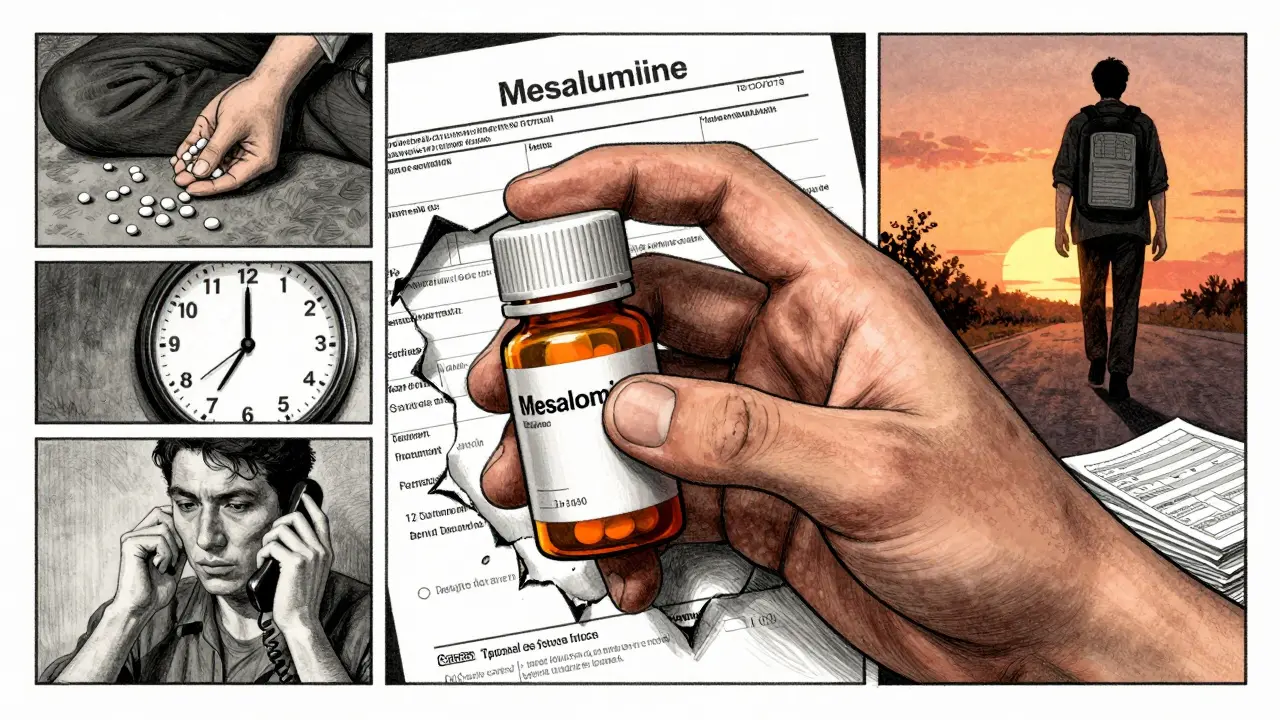
Denial isn’t the end. It’s step two. You have 60 days to file an internal appeal. If that fails, you can request an external review by an independent third party - free of charge. The approval rate for appeals is high: 58% of initial denials are overturned, according to the Crohn’s & Colitis Foundation. But only if you push. Most people give up after the first no. The ones who win? They submit a second, more detailed request. One Reddit user, PharmTechSarah, got her mesalamine approved only after four tries - each time adding new flare-up data.
Costs you might not realize
Even if you win the exception, you’re not out of the woods. Federal rules say: if a non-formulary drug is approved, you can’t ask for a lower cost-sharing tier. That means you might still pay 3.7 times more than the formulary version. SmithRx found patients paid an average of $287 more per month for the same generic drug just because it wasn’t on the list. That’s why 38% of people skip doses or cut pills in half. It’s not noncompliance - it’s survival.
Who gets denied most - and why
Not all drug classes are treated equally. Anticonvulsants and insulin have high approval rates because CMS mandates them. But gastrointestinal drugs? That’s where the system breaks down. For non-formulary mesalamine or sulfasalazine, approval rates hover around 52%. Why? Insurers assume all 5-ASA drugs are interchangeable. But for people with ulcerative colitis, they’re not. One formulation might cause nausea. Another might not release properly in the colon. The plan doesn’t see that. Your doctor has to prove it.
What’s changing in 2025
The system is slowly getting better. In October 2023, CMS rolled out standardized clinical criteria for common conditions - meaning doctors now have clear guidelines on what evidence to include. By 2025, the exceptions process will integrate directly with electronic health records, cutting approval times by up to 40%. The Inflation Reduction Act now forces plans to automatically cover insulin and naloxone without exceptions. That’s progress. But new problems are emerging. Specialty pharmacies are now handling more generics - like bioidentical hormones - and those are often excluded from standard formularies entirely. The system is catching up, but it’s still a maze.
What to do right now
If you’re facing a denial:
- Don’t stop taking your medication unless your doctor says so.
- Call your pharmacy and ask for the formal denial notice.
- Ask your doctor: "Can you complete a coverage determination form with my lab results and history?" Bring printed records.
- Call your insurer and ask: "What are the exact clinical criteria you need to approve this?" Write it down.
- Use the GoodRx or NeedyMeds app to find cash prices. Sometimes paying out-of-pocket is cheaper than waiting.
And if you’ve been denied before? Try again. With better documentation. The system works - but only if you use it.
What is a non-formulary generic?
A non-formulary generic is a generic version of a medication that is not included on your insurance plan’s official list of covered drugs. Even though it’s the same active ingredient as the covered version, the plan doesn’t pay for it - so you pay full price unless you get an exception.
Can I appeal a denial for a non-formulary generic?
Yes. Federal law requires all Medicare Part D and most commercial plans to have an exceptions process. You can request coverage based on medical necessity. Over half of these appeals are approved, especially when you include clinical evidence like lab results or past treatment failures.
How long does the exception process take?
For standard requests, plans must respond within 72 business hours. For urgent cases - like a worsening condition or running out of medication - they must respond within 24 hours. You can also request a 72-hour emergency supply while waiting.
Why is my doctor’s note not enough?
Generic statements like "this drug works better for my patient" aren’t enough. Plans need specific clinical data: lab values, dates of failed alternatives, symptoms experienced, or documented side effects. The more objective evidence you provide, the higher your approval odds.
Can I get a lower copay after approval?
No. Even if your non-formulary drug is approved, federal rules prevent you from requesting a lower cost-sharing tier. You’ll still pay more than if it were on the formulary - sometimes 3 to 4 times more. That’s why some patients pay cash instead, especially if the cash price is lower than their coinsurance.
Which drugs are most often denied?
Gastrointestinal drugs like mesalamine and sulfasalazine have the lowest approval rates - around 52%. Autoimmune and neurological drugs are also frequently blocked. Insulin and anticonvulsants are rarely denied because CMS requires plans to cover them.
Is it worth appealing if I’m paying cash?
Yes. Even if you’re paying out of pocket now, getting coverage approved means you won’t have to do it again next year. Many plans lock in exceptions for a full year. Plus, if you’re on Medicare, the cost you pay now counts toward your out-of-pocket maximum. That can save you thousands later.




Kelly Beck
4 January 2026 - 15:53 PM
OMG I literally cried reading this. My mom got denied for her mesalamine last year and we had to pay $400 out of pocket for a month’s supply-she’s on SSDI and it nearly broke us. I didn’t know you could appeal-thank you for laying this out like a roadmap. I just submitted her second request with her colonoscopy results and lab values. Fingers crossed. 💪❤️
Wesley Pereira
4 January 2026 - 19:32 PM
So let me get this straight… the system’s designed so you have to be a medical researcher just to get a generic drug that’s been on the market for 15 years? And the insurance company’s ‘formulary’ is just a fancy word for ‘we made a deal with Big Pharma to screw you over’? Classic. I’ve seen this with my cousin’s insulin too. They call it ‘cost containment.’ I call it ‘medical extortion.’
Isaac Jules
6 January 2026 - 04:02 AM
Why are people still surprised by this? Insurance is a racket. They don’t care if you die slowly from uncontrolled Crohn’s-they care if their quarterly earnings dip. If you’re not rich, you’re just collateral damage. Stop pretending this is a healthcare system. It’s a profit engine with a stethoscope.
Rachel Wermager
7 January 2026 - 22:47 PM
Actually, the 2025 EHR integration is only mandated for Medicare Advantage plans under CMS 1724-F. Commercial insurers aren’t required to adopt it unless they’re under state-level formulary transparency laws. Also, ‘clinical evidence’ isn’t just lab values-it needs to include pharmacokinetic data, bioequivalence reports, and documented adverse event timelines per FDA Guidance 2020-01. Most docs don’t know this.
Vinayak Naik
7 January 2026 - 23:19 PM
Been there. Got denied for my sulfasalazine last year. Paid $310 cash at Walmart-cheaper than my $450 copay. Then I called my insurer and said, ‘I’m paying cash now, but I’ll submit this as a retroactive exception if you ever want to reimburse me.’ They called back in 48 hours. Approved. No appeal needed. Sometimes you just gotta be annoying.
Brian Anaz
9 January 2026 - 15:07 PM
This is why I hate American healthcare. You get punished for being sick. My brother had to cut his epilepsy meds in half because the ‘cheaper’ generic made him seize. He’s a veteran. They gave him a medal and then denied his meds. This ain’t freedom. It’s cruelty with a clipboard.
Ashley S
11 January 2026 - 03:19 AM
People just need to stop being lazy. If your insurance doesn’t cover it, get a different insurance. Or pay cash. Or move to Canada. Simple.
Tom Swinton
12 January 2026 - 10:15 AM
I’ve helped over 30 people navigate this process, and the #1 thing that changes the outcome? The doctor’s letter. Not just ‘my patient needs this’-but ‘Patient X experienced 3 hospitalizations in 6 months on Formulary Drug A, with A1c rising from 6.8 to 9.1, and stool calprotectin spiking from 12 to 184 ug/g.’ That’s the language that makes them pause. It’s not about begging. It’s about speaking their bureaucratic language.
Pavan Vora
14 January 2026 - 00:05 AM
Wait… so… if I’m on a non-formulary generic… and I get approved… I still pay more? Even though it’s the same drug? That’s… that’s… insane. I mean… like… how is this even legal? I’m from India, and here generics are cheap and covered… I don’t understand how this works here. Is this… capitalism? Or just… greed?
Indra Triawan
14 January 2026 - 07:37 AM
It’s all so tragic. We’re all just floating in a sea of systemic neglect. The body remembers trauma, and so does the healthcare system. When you’re denied a drug, you’re not just denied a pill-you’re denied dignity. And yet, we’re told to be grateful for what we have. What a cruel, beautiful paradox.
Susan Arlene
14 January 2026 - 09:36 AM
my dr just handed me a form and said ‘fill this out’ and i was like… ok. turned out the pharmacy gave me the wrong generic. turned out the right one was covered. no appeal needed. sometimes it’s just a mix-up. check the label. check the name. don’t assume it’s a conspiracy… unless it is.
Venkataramanan Viswanathan
15 January 2026 - 23:57 PM
As someone who works in pharmaceutical logistics in India, I can confirm: the same generic drug manufactured in Hyderabad and shipped to the U.S. is often priced 10x higher here, not because of quality, but because of insurance middlemen, rebate structures, and formulary gatekeeping. The active ingredient is identical. The cost difference is purely corporate. This isn’t healthcare. It’s financial engineering disguised as medicine.
Leonard Shit
17 January 2026 - 14:19 PM
My cousin got her mesalamine approved after 5 tries. Each time she added a new flare-up log, a photo of her stool (yes, really), and a calendar of missed workdays. The insurer finally caved when she included her therapist’s note: ‘Patient reports suicidal ideation due to financial stress from medication costs.’ That’s when they moved. Mental health + physical health = power move.
Joann Absi
19 January 2026 - 03:28 AM
THIS IS WHY I HATE AMERICA. WE HAVE THE BEST MEDICINE IN THE WORLD BUT WE LET CORPORATIONS DECIDE WHO LIVES AND WHO DIES. I’M SO ASHAMED. MY GRANDMA HAD TO CHOOSE BETWEEN HER INSULIN AND HER HEATING BILL. THIS ISN’T JUST BROKEN. IT’S EVIL.
Mukesh Pareek
19 January 2026 - 20:56 PM
Let’s be clear: formularies exist for a reason. If every generic were covered, premiums would skyrocket. The issue isn’t greed-it’s sustainability. Patients need to understand that insurers aren’t villains; they’re triaging risk. The solution isn’t to rage against the system-it’s to advocate for tiered access based on clinical necessity, not emotional appeals. Data over drama.