Acid Indigestion & IBS Symptom Checker
Symptom Assessment
Select the symptoms you're experiencing to get personalized insights about acid indigestion and IBS.
Upper Digestive Symptoms
Lower Digestive Symptoms
Trigger-Related Symptoms
Ever felt a burning stomach after a big meal and then, a few hours later, battled cramping in your lower belly? Those two bouts might not be random - they often share hidden pathways. Below we untangle the link between acid indigestion and Irritable Bowel Syndrome (IBS), show why the connection matters, and give you practical steps to break the cycle.
Key Takeaways
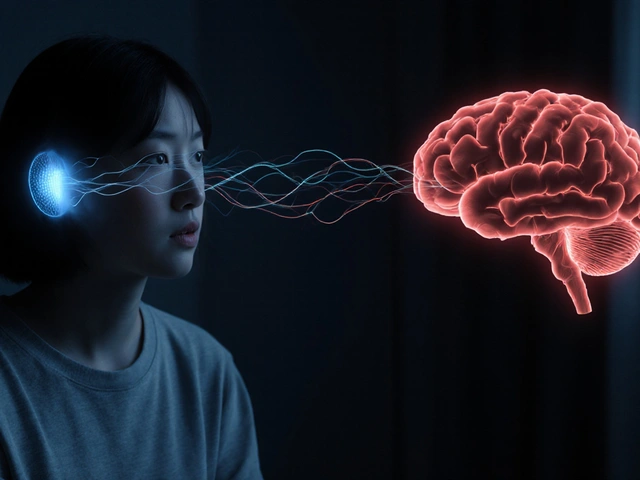
- Acid indigestion (dyspepsia) and IBS frequently overlap because they both involve gut motility, sensitivity, and the gut‑brain axis.
- Common triggers-spicy foods, stress, caffeine, and certain medications-can flare both conditions at the same time.
- Diagnosing the overlap starts with a thorough symptom diary and, when needed, tests for GERD, H. pylori, and IBS‑type bowel patterns.
- Managing the duo usually means a blended approach: diet tweaks (low‑FODMAP), stress‑reduction, targeted meds (PPIs or antispasmodics), and sometimes probiotics.
- Seek medical help if you notice weight loss, blood in stool, or persistent vomiting, as these can signal more serious disease.
What Is Acid Indigestion?
Acid indigestion is a common name for dyspepsia, a feeling of fullness, discomfort, or burning in the upper abdomen after eating. It often stems from excess stomach acid, delayed gastric emptying, or irritation of the lining. Typical signs include bloating, belching, nausea, and a sour taste that rises into the throat.
Understanding Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder marked by recurring abdominal pain, altered bowel habits (diarrhea, constipation, or both), and bloating. Unlike structural diseases, IBS shows no clear tissue damage, but the gut’s nerves and muscles react abnormally to normal stimuli.

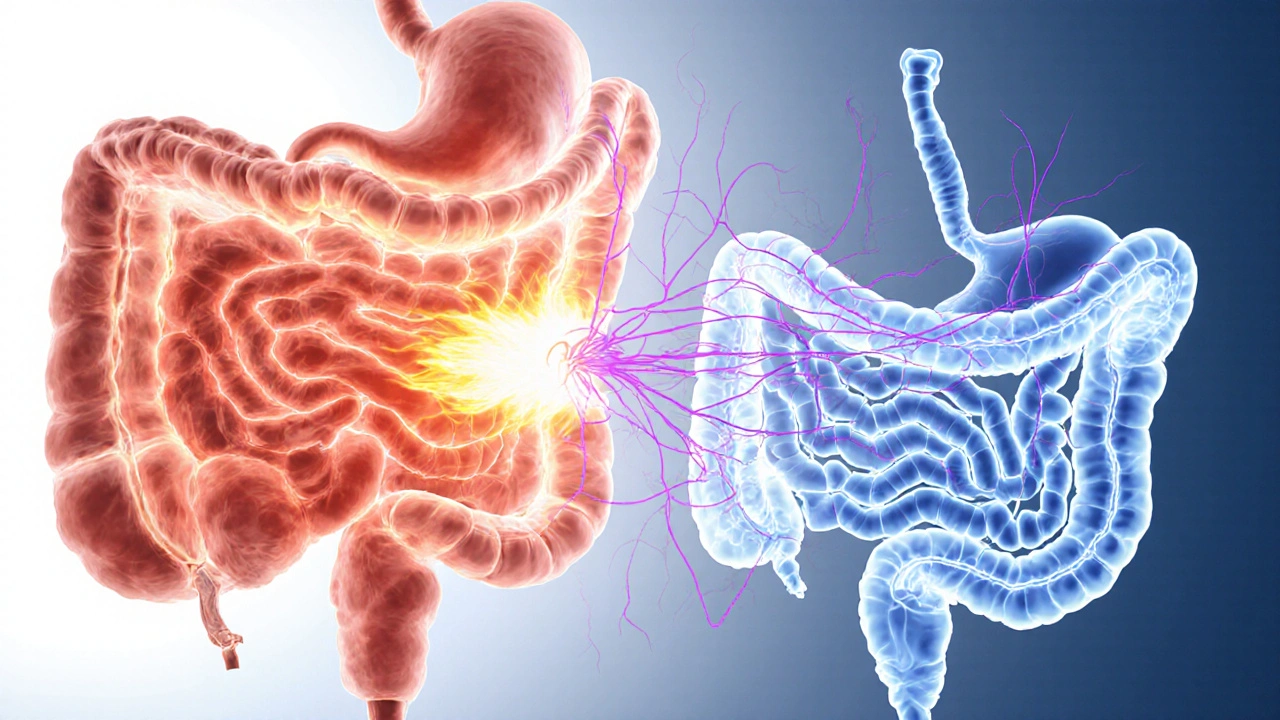
Why the Two Often Appear Together
Both conditions share three major underlying mechanisms:
- Gut‑brain axis disruption: Stress or anxiety sends signals that can increase stomach acid production (worsening indigestion) while also heightening intestinal muscle sensitivity (triggering IBS pain).
- Visceral hypersensitivity: People with IBS often have a lowered pain threshold throughout the GI tract, making them more likely to feel the burning of acid as a painful event.
- Motility irregularities: Slower gastric emptying can cause indigestion, and irregular colonic motility is a hallmark of IBS. The same hormonal imbalances (like excess serotonin) can affect both stomach and colon.
Key Overlapping Triggers
Identifying shared triggers helps you target both problems simultaneously. Common culprits include:
- High‑fat or fried meals - they delay stomach emptying and boost gas production in the colon.
- Spicy foods - capsaicin can irritate the esophageal lining and also stimulate colonic nerves.
- Caffeine and carbonated drinks - they increase acid secretion and can cause rapid bowel movements.
- Alcohol - relaxes the lower esophageal sphincter (allowing reflux) and irritates the gut lining.
- Stress & lack of sleep - amplify the gut‑brain axis, raising both acid output and bowel spasm frequency.
Diagnosing the Overlap
Doctors start with a detailed history, asking you to track:
- Meal types and timing of symptoms.
- Frequency of heartburn, belching, and lower‑abdomen pain.
- Any red‑flag signs (weight loss, anemia, blood in stool).
If red flags are absent, they may employ the following tests:
- Upper endoscopy - checks for erosive esophagitis or ulcers that could cause chronic indigestion.
- H. pylori breath or stool test - a bacterial infection that raises stomach acid levels and can mimic IBS symptoms.
- Breath hydrogen test - identifies excess carbohydrate fermentation, a frequent IBS trigger.
When both sets of symptoms persist, clinicians often label the condition as “functional dyspepsia with IBS overlap.”
Management Strategies That Hit Both Targets
Because the two conditions share triggers, a combined plan works best. Below is a step‑by‑step approach you can start at home, then fine‑tune with a healthcare professional.
- Dietary Reset
- Adopt a low‑FODMAP diet for 4‑6 weeks. It reduces fermentable carbs that cause gas and IBS cramps, and often lessens bloating that worsens indigestion.
- Limit trigger foods identified in your symptom diary (spicy, fatty, caffeine, alcohol).
- Eat smaller, more frequent meals - this helps keep stomach acid from pooling and steadies colonic activity.
- Stress Management
- Practice mindfulness or guided breathing for 10 minutes daily - studies show a 30‑40% drop in both heartburn episodes and IBS pain.
- Regular low‑impact exercise (walking, yoga) improves gut motility and reduces stress hormones.
- Targeted Medications
- For frequent acid reflux, a short course of proton pump inhibitor (PPI) such as omeprazole can calm stomach acid.
- If you experience cramping, an antispasmodic like dicyclomine may ease colonic muscle spasms.
- When constipation dominates, a fiber supplement (psyllium) or a low‑dose osmotic laxative can normalize stool frequency.
- Probiotics and Gut‑Brain Support
- Strains like Bifidobacterium infantis have been shown to reduce IBS bloating and improve dyspepsia scores.
- Consider a daily fermented food (yogurt, kefir) if you tolerate dairy.
- When to Seek Professional Help
- Unexplained weight loss or night sweats.
- Blood in vomit or stool.
- Symptoms that persist despite lifestyle changes for more than 8 weeks.
Comparing Symptoms: Acid Indigestion vs. IBS
| Feature | Acid Indigestion (Dyspepsia) | Irritable Bowel Syndrome |
|---|---|---|
| Primary location | Upper abdomen, behind breastbone | Lower abdomen, often left or central |
| Typical triggers | Spicy/fatty foods, caffeine, alcohol, H. pylori | FODMAPs, stress, irregular meals, antibiotics |
| Key sensations | Burning, fullness, sour taste, bloating | Cramping, urgency, diarrhea or constipation, gas |
| Relief methods | Antacids, PPIs, smaller meals | Low‑FODMAP diet, antispasmodics, probiotics |
| Overlap signs | Persistent bloating, belching that continues after meals | Upper‑abdomen discomfort that worsens after eating |
Real‑World Example: Sarah’s Journey
Sarah, a 34‑year‑old graphic designer, started noticing a sour after‑taste and occasional heartburn after lunch. Two months later, she added frequent abdominal cramps and alternating diarrhea. She kept a food‑symptom log, which showed that pizza nights, coffee spikes, and late‑night stress were common before flare‑ups.
Her doctor ordered a breath test (negative for H. pylori) and recommended a trial of a low‑FODMAP diet combined with a short PPI course. Within three weeks, Sarah’s burning subsided, and after six weeks her IBS‑type cramps dropped by 60%. Adding a daily probiotic with Bifidobacterium infantis sealed the improvement.
Sarah’s case illustrates how addressing both acid production and gut‑brain stress can break the vicious cycle.
Quick Checklist for Managing Both Conditions
- Track meals and symptoms for at least two weeks.
- Trim trigger foods: high‑fat, spicy, caffeine, alcohol.
- Eat 4-5 small meals a day; avoid lying down within 2hours after eating.
- Start a low‑FODMAP trial (see reputable guide or dietitian).
- Practice daily stress‑relief (mindful breathing, short walk).
- Consider a short PPI if heartburn persists more than twice a week.
- Introduce a probiotic strain with clinical IBS support.
- Schedule a doctor visit if red‑flag symptoms appear.
Frequently Asked Questions
Can acid reflux cause IBS?
Acid reflux itself doesn’t cause IBS, but the irritation and inflammation from chronic reflux can sensitize the gut’s nerves, making IBS‑type pain more likely. Managing reflux often eases IBS symptoms as well.
Is it safe to take PPIs long‑term if I also have IBS?
Short‑term PPI use (up to 8 weeks) is generally safe. Long‑term use may affect gut microbiota, potentially worsening IBS. If you need ongoing acid control, talk to your doctor about the lowest effective dose or alternative strategies like H2 blockers.
Do probiotics help both acid indigestion and IBS?
Certain probiotic strains, especially Bifidobacterium infantis and Lactobacillus plantarum, have shown benefit in reducing IBS bloating and improving dyspepsia scores. Choose a product with ≥10billion CFU and clinically studied strains.
How long should I follow a low‑FODMAP diet?
Typically 4-6 weeks for the elimination phase, followed by a gradual re‑introduction to pinpoint specific triggers. A dietitian can help you personalize the re‑introduction schedule.
When is an endoscopy necessary?
If you have alarm symptoms like vomiting blood, unintentional weight loss, or difficulty swallowing, an upper endoscopy helps rule out ulcers, esophageal cancer, or severe GERD.


Marcia Hayes
14 October 2025 - 17:56 PM
Great breakdown! I love how it ties the gut‑brain axis into everyday habits.
Danielle de Oliveira Rosa
17 October 2025 - 03:32 AM
Indeed, the interconnection between acid dyspepsia and IBS underscores the importance of a holistic diagnostic approach. The article correctly highlights symptom overlap without conflating distinct pathophysiologies. By emphasizing a detailed symptom diary, clinicians can differentiate primary from secondary manifestations. Moreover, the acknowledgment of red‑flag signs reflects prudent clinical vigilance. Ultimately, this synthesis serves as a valuable guide for both patients and providers.
Tarun Rajput
19 October 2025 - 13:08 PM
Allow me to elaborate on the nuanced mechanisms that bind acid indigestion and irritable bowel syndrome into a unified clinical tapestry; the gut‑brain axis, a bidirectional conduit of neural, hormonal, and immunological signals, operates like an intricate orchestra where each instrument-be it gastric acid secretion, colonic motility, or central processing-must remain in harmony to maintain gastrointestinal equilibrium. When one component falters, such as an overproduction of gastric acid triggered by stress‑induced cortisol surges, the resulting mucosal irritation not only precipitates the classic burning sensation but also sensitizes visceral afferents, lowering the pain threshold throughout the gastrointestinal tract. This heightened visceral hypersensitivity predisposes the colon to exaggerated contractile responses to ordinary luminal stimuli, manifesting as the cramping and altered bowel habits characteristic of IBS. Furthermore, delayed gastric emptying, a frequent accompaniment of dyspepsia, prolongs exposure of the duodenum to acidic chyme, fostering feedback loops that exacerbate both upper and lower abdominal discomfort. Dietary indiscretions rich in fat and spice impede gastric clearance while simultaneously providing fermentable substrates for colonic microbiota, thereby amplifying gas production and bloating-a shared symptom that often blurs diagnostic boundaries. Psychological stress, mediated through the hypothalamic‑pituitary‑adrenal axis, intensifies gastric acid output and disrupts enteric nervous system regulation, creating a vicious cycle wherein anxiety fuels reflux, which in turn aggravates gut motility disturbances. In this context, therapeutic strategies that target a single facet-such as proton pump inhibitors-may offer transient relief yet fail to address the broader dysregulation; a multimodal approach encompassing low‑FODMAP dietary modification, stress‑reduction techniques, and judicious use of antispasmodics tends to yield more sustainable outcomes. It is also noteworthy that certain probiotic strains, particularly Bifidobacterium infantis, have demonstrated efficacy in attenuating both dyspeptic and IBS‑related symptoms by restoring microbial balance and modulating mucosal immunity. Clinicians should therefore adopt a comprehensive assessment protocol, integrating symptom chronology, trigger identification, and targeted investigations, to delineate the predominant pathology while remaining vigilant for alarm features that mandate endoscopic evaluation. Patient education remains paramount; empowering individuals to maintain a meticulous food‑symptom log facilitates personalized therapy adjustments and fosters a collaborative patient‑provider relationship. In sum, the confluence of physiological, neuro‑endocrine, and psychosocial elements necessitates an integrative management paradigm that respects the complexity of this overlap, rather than compartmentalizing each condition in isolation.
Joe Evans
21 October 2025 - 22:44 PM
Nice summary! 😊 The diet tweaks are simple, the stress tips are easy, and the meds are clear. Keep it up!
Colin Boyd
24 October 2025 - 08:20 AM
While the article is comprehensive it neglects the economic burden of long‑term PPI use on health systems.
Annie Tian
26 October 2025 - 16:56 PM
Great point! It’s true that prolonged acid‑suppressor therapy can have downstream effects, such as altered gut microbiota and increased infection risk; therefore, periodic reassessment is essential, especially when patients are also managing IBS symptoms.
April Knof
29 October 2025 - 02:32 AM
From a cultural standpoint, many traditional cuisines already incorporate low‑FODMAP principles-think of fermented kimchi, simple rice dishes, and lean proteins-which can make dietary transitions smoother for diverse populations.
Tina Johnson
31 October 2025 - 12:08 PM
While I appreciate the cultural nod, the article fails to address that certain regional spices, such as chilies and cinnamon, can exacerbate acid production; a more nuanced guide should differentiate between beneficial fermentation and harmful irritants.
Sharon Cohen
2 November 2025 - 21:44 PM
Honestly, I think the overlap is overhyped; most people just have bad eating habits.
Rebecca Mikell
5 November 2025 - 07:20 AM
I see where you’re coming from, but the evidence shows a genuine physiological link, and acknowledging it helps many sufferers get proper care.
Ellie Hartman
7 November 2025 - 16:56 PM
For anyone starting out, I recommend beginning with a simple symptom diary-note meals, timing, and any discomfort. This foundation makes later diet tweaks and medical discussions much more effective.
dany prayogo
10 November 2025 - 02:32 AM
Well, if you’re going to suggest a low‑FODMAP trial, perhaps you should also mention the psychological toll of such restrictive eating-because let’s face it, most people will feel like they’re living on a bland diet forever, which can be just as stressful as the symptoms themselves; furthermore, the article doesn’t even hint at the importance of re‑introducing foods systematically to avoid unnecessary long‑term deprivation; on top of that, the recommendation to use probiotics feels a bit like a sales pitch without citing specific strains; and finally, while the checklist is handy, it omits a key point: hydration, which is absolutely vital for both acid regulation and bowel regularity.
Wilda Prima Putri
12 November 2025 - 12:08 PM
Nice checklist-just don’t forget to actually follow it.
Edd Dan
14 November 2025 - 21:44 PM
I think the article does a good job, but sometimes the language can be a bit confusing, especially when it talks about the gut‑brain axis. It could use some simpler examples to help readers get the point.
Cierra Nakakura
17 November 2025 - 07:20 AM
Let’s keep the momentum going! 🚀