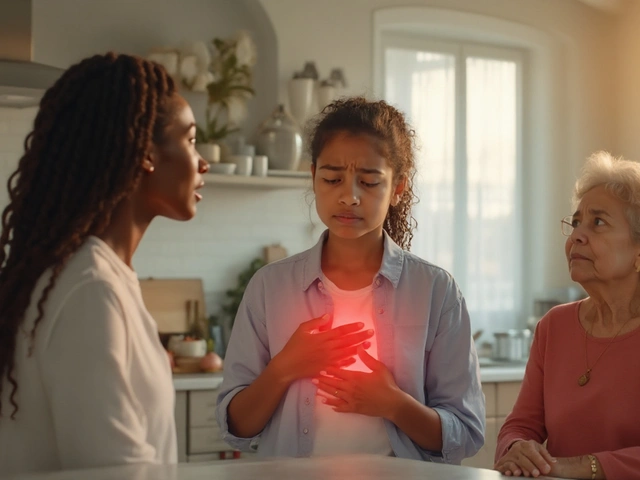
Ever felt that persistent itch around the anus and wondered if it could be more than a simple irritation? That uncomfortable sensation can sometimes be a clue that your gut is sending distress signals. Below we break down why anal itching and Crohn's disease often show up together, what to watch for, and how to get back to comfort.
What Exactly Is Anal Itching?
Anal itching is the urge to scratch the skin around the anus, caused by irritation, inflammation, or moisture. It’s technically called pruritus ani and can spark from everyday things like sweat, tight clothing, or a sudden diet change. However, when the itch lingers for weeks, it’s worth digging deeper.
Getting to Know Crohn’s Disease
Crohn's disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from mouth to anus. Unlike ulcerative colitis, which stays limited to the colon, Crohn’s can create patchy lesions, fistulas, and strictures. Around 3 million people in the U.S. live with this condition, and one of the trickier side‑effects is perianal discomfort.
Why Crohn’s Can Trigger Anal Itching
The link isn’t magic-it’s a cascade of physiological events:
- Perianal inflammation: Active disease near the rectum inflames the skin, making it hypersensitive.
- Fistulas and abscesses: Crohn’s often creates abnormal tunnels (fistulas) that leak fluid, causing irritation and a burning itch.
- Frequent watery stools: Diarrhea leaves the anal area moist, breaking down the protective skin barrier.
- Medication side effects: Some steroids or antibiotics disrupt the gut flora, leading to skin irritation.
When any of these factors combine, the nerve endings around the anus receive a constant “scratch‑me” signal, turning a minor nuisance into a daily frustration.
Common Itching Triggers vs. Crohn’s‑Related Triggers
| Cause | Typical Scenario | Why It Happens |
|---|---|---|
| Hygiene Issues | Insufficient cleaning after bowel movements | Residual stool irritates skin nerves |
| Hemorrhoids | Swollen veins causing itching after bowel movements | Enlarged vessels press on sensitive tissue |
| Skin Conditions (eczema, psoriasis) | Pre‑existing dermatitis on the perianal area | Inflammatory skin disease adds extra itch signals |
| Crohn's disease - Perianal Fistula | Visible opening or discharge near the anus | Leakage of intestinal fluid irritates skin |
| Crohn's disease - Diarrhea‑Induced Moisture | Multiple loose stools per day | Continuous wetness breaks down protective barrier |
| Medication‑Induced Dermatitis | Topical steroids or antibiotics used for flare‑ups | Altered skin flora leads to secondary irritation |
When to Call a Doctor
If you notice any of the following, it’s time to get professional help:
- Itch that lasts longer than two weeks despite good hygiene.
- Bleeding, discharge, or a visible lump around the anus.
- Severe pain that wakes you up at night.
- Concurrent Crohn’s flare‑ups - fever, abdominal cramping, weight loss.
A gastroenterologist can differentiate a Crohn’s‑related issue from a simple skin problem and recommend targeted treatment.
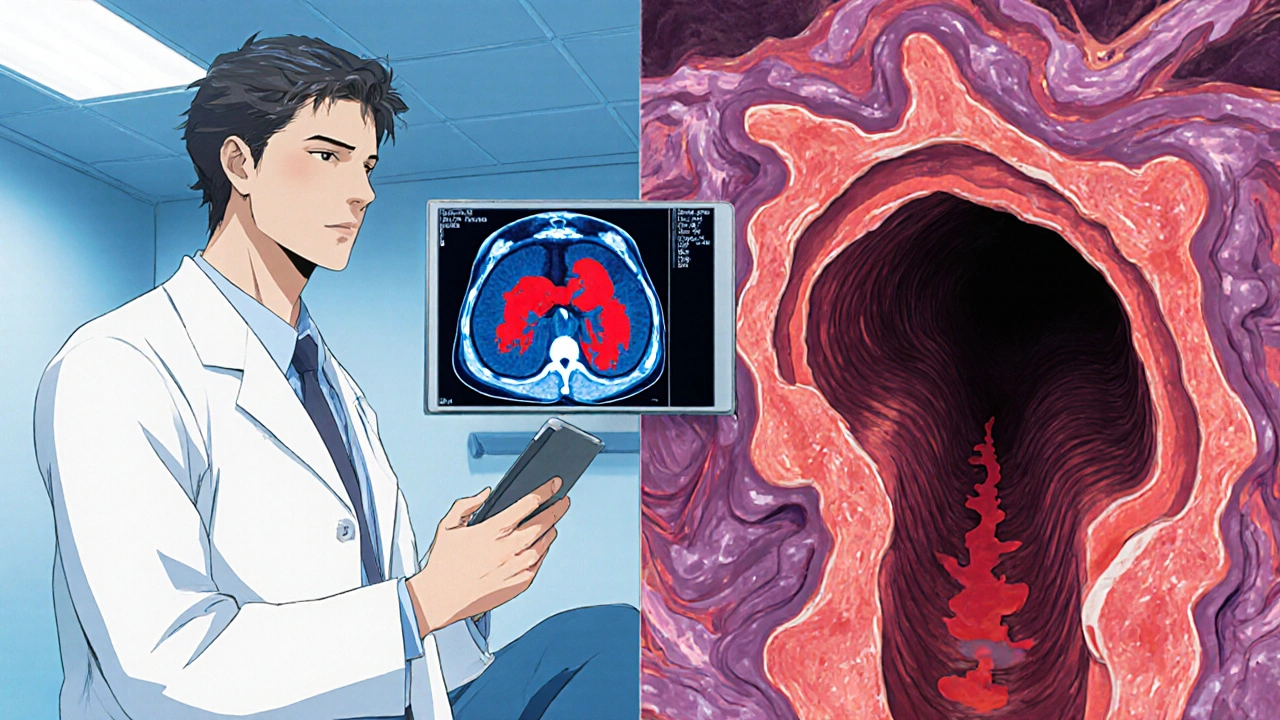
How Doctors Diagnose the Source
The diagnostic pathway typically includes:
- Physical exam: Visual inspection and gentle palpation to spot abscesses or fistulas.
- Endoscopy or colonoscopy: Direct view of the colon lining, often with biopsies.
- Imaging (MRI, ultrasound): Best for mapping fistulas and deep tissue inflammation.
- Stool tests: Rule out infections that could mimic Crohn’s symptoms.
Finding the exact cause guides the next steps - whether you need a medication adjustment or a minor surgical procedure.
Managing Anal Itching When Crohn’s Is Behind It
Effective relief usually means tackling both the itch and the gut inflammation.
1. Control the Underlying Disease
- Biologics (e.g., infliximab, adalimumab): Reduce systemic inflammation, often shrinking fistulas.
- Immunomodulators (azathioprine, methotrexate): Keep flare‑ups at bay.
- Targeted antibiotics (metronidazole, ciprofloxacin): Helpful for perianal abscesses.
2. Local Symptom Relief
- Barrier creams: Zinc oxide or petroleum‑jelly protect skin from moisture.
- Topical steroids: Low‑dose hydrocortisone for short‑term inflammation.
- Prescription suppositories: Mesalamine or corticosteroid suppositories calm the rectal lining.
3. Hygienic Practices
- Pat, don’t rub, after each bowel movement.
- Use fragrance‑free, hypoallergenic wipes.
- Switch to sitz baths (warm water) for 10‑15 minutes twice daily during flare‑ups.
4. Dietary Tweaks
- Increase soluble fiber (oats, peeled apples) to bulk up stools.
- Limit spicy foods, caffeine, and alcohol - common culprits for diarrhea.
- Consider a low‑FODMAP diet if you notice gas and watery stools worsening the itch.
5. Probiotic Support
Evidence from 2023 trials shows certain strains (Bifidobacterium longum, Lactobacillus rhamnosus) can restore gut flora balance, reducing both diarrhea frequency and perianal irritation.
Living with the Flare‑Ups: Lifestyle Tips
Even with medication, you’ll likely have good‑and‑bad days. Here are practical habits that keep the itch at bay:
- Stay hydrated: Aim for 2‑3 liters of water daily; it softens stool without causing excess liquid loss.
- Schedule bathroom breaks: Avoid prolonged sitting on the toilet - it increases pressure on the anal sphincter.
- Wear breathable underwear: Cotton or moisture‑wicking fabrics reduce sweat buildup.
- Track symptoms: A simple diary (stool consistency, flare‑up intensity, diet) helps your doctor fine‑tune therapy.
Quick Takeaways
- Anal itching can be a sign of Crohn’s‑related perianal inflammation or fistulas.
- Frequent watery stools and moisture are major culprits for skin irritation.
- Diagnosing the cause involves physical exams, endoscopy, and sometimes MRI.
- Treat Crohn’s systemically while using barrier creams, sitz baths, and diet changes for immediate relief.
- Seek medical care if itching persists beyond two weeks, bleeds, or is accompanied by discharge.
Frequently Asked Questions
Can Crohn’s cause anal itching without visible fistulas?
Yes. Even without an actual fistula, inflammation of the rectal lining and chronic diarrhea can leave the skin constantly damp, triggering itch sensations.
Are over‑the‑counter creams safe for Crohn’s patients?
Barrier ointments like zinc oxide are generally safe. However, steroid creams should be used only as prescribed, because prolonged use can thin the skin and increase infection risk.
How long does it take for a sitz bath to relieve itching?
Most patients notice a calm‑down of burning within 10‑15 minutes of the first bath. Consistent twice‑daily baths during flare‑ups speed up healing.
Do biologics cure perianal fistulas?
Biologics can close many fistulas, but they don’t guarantee a permanent cure. Some patients need surgical set‑backs combined with medication.
Is a low‑FODMAP diet recommended for everyone with Crohn’s?
It helps many, especially those with frequent diarrhea and gas, but it isn’t a one‑size‑fit solution. Work with a dietitian to avoid nutrient gaps.




eric smith
21 October 2025 - 18:43 PM
Oh, you didn’t spot the obvious: chronic diarrhea is the primary source of that never‑ending moisture that turns the perianal skin into a literal sandpaper. When the stool streams past the sphincter, it strips away the protective mucous layer faster than you can reach for a wipe. The resulting exposure triggers the nerve endings to scream “scratch me!” like a bad pop‑song hook. Add a fistula to the mix, and you’ve got fluid leaking straight onto the skin, creating a perfect breeding ground for irritation. Bottom line: if you’re constantly battling an itch, look at your stool consistency first, not just the hemorrhoids.
Brandy Eichberger
21 October 2025 - 20:06 PM
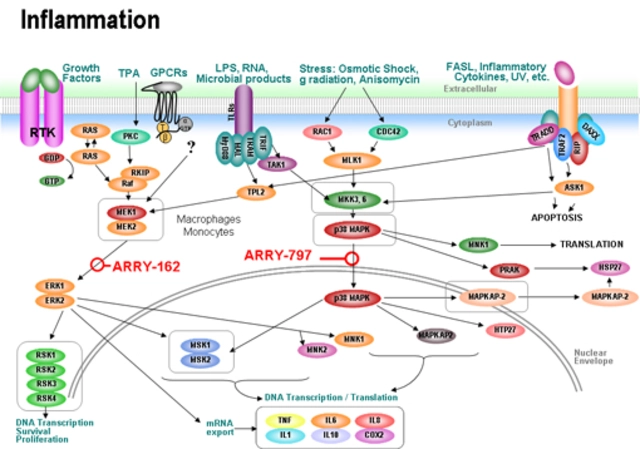
From a more refined perspective, one might consider the interplay between systemic inflammation and localized cutaneous responses. The cytokine cascade inherent to Crohn’s disease does not confine itself to the gut; it can sensitize peripheral nerves, augmenting pruritus. Moreover, the use of broad‑spectrum antibiotics occasionally disrupts the perianal microbiome, further compromising barrier function. It would be prudent to incorporate probiotic strains, such as Bifidobacterium, into the therapeutic regimen. Ultimately, a holistic approach-addressing both the immune dysregulation and the micro‑environment-offers the most elegant solution.
Eli Soler Caralt
21 October 2025 - 21:30 PM
i cant help but wonder wtf the gut does to our skin 😒 it's like the body playing hide n seek with the itch 🤔
i read that even without a fistula the mere inflammation of the rectal mucosa releases prostaglandins that prank the nerve endings 😅
so yeah, prolly not just about the poop, it's also about the internal fire 🌶️
anyway, hope this helps, stay dry & keep that zinc ointment handy 🙌
Eryn Wells
21 October 2025 - 22:53 PM
Let’s remember that dealing with perianal discomfort can feel isolating, but you’re definitely not alone. A supportive community, whether online or in a local IBD group, can share practical tips like the best fragrance‑free wipes or breathable underwear brands. Also, don’t underestimate the power of a warm sitz bath; it can dramatically reduce the burning sensation within minutes. If you ever feel the itch is getting out of hand, reaching out to a gastroenterologist early can prevent complications. 🌍💙
Kathrynne Krause
22 October 2025 - 00:16 AM
Absolutely! Turning those small daily rituals into empowering habits can transform your whole outlook. Picture this: a quick 10‑minute sitz bath each morning, followed by a splash of zinc oxide-like armor for your skin. Pair that with a colourful, cotton‑blend brief that says, “I’m ready to tackle the day, itch‑free!” and you’ll notice a shift in confidence. Keep tracking your flare‑ups in a journal; it’s the secret weapon to fine‑tune your meds with your doctor. You’ve got this! 🌟💪
Angela Koulouris
22 October 2025 - 01:40 AM
One practical piece of advice that often gets overlooked is the timing of bowel movements. By scheduling regular, relaxed visits to the restroom-avoiding the urge to rush-you reduce pressure on the anal sphincter, which can lessen irritation. Additionally, consider using a peri‑bottle with lukewarm water instead of dry wipes; it gently cleanses without stripping natural oils. Pair these habits with a low‑FODMAP diet to curb excess watery stools, and you’ll likely see a noticeable drop in itching. Remember, consistency is key, and small adjustments can add up to big relief.
Esther Olabisi
22 October 2025 - 03:03 AM
Oh great, another “just use wipes” suggestion. Yeah, because that solved everything for everyone else, right? 🙄
Ivan Laney
22 October 2025 - 04:26 AM
Let us begin by acknowledging the sheer complexity of the human gastrointestinal tract, a marvel of evolutionary engineering that, when afflicted by Crohn’s disease, becomes a battlefield of immunological misfires. The first point of contention lies in the relentless inflammatory cascade, where cytokines such as TNF‑alpha and interleukin‑6 wage war upon the mucosal lining, eroding the very barrier that protects the perianal skin. Consequently, the exposed nerve endings are directly assaulted, sending pruritic signals that are interpreted by the central nervous system as an incessant itch. In parallel, the formation of perianal fistulas creates aberrant conduits through which intestinal contents extrude, each droplet of fluid acting as a chemical irritant that further compromises the epidermal integrity. This dual onslaught-systemic inflammation and localized fluid leakage-ensures that the patient experiences a chronic, often nocturnal, scratching compulsion. Adding to the misery, the frequent watery stools characteristic of an active Crohn’s flare strip away residual moisturizing factors, leaving the skin desiccated and more susceptible to micro‑abrasions. The use of broad‑spectrum antibiotics, while sometimes indispensable, can decimate the beneficial bacterial flora that ordinarily competes with pathogenic organisms, thereby fostering opportunistic overgrowth that may manifest as secondary dermatitis. It is here that the practitioner must consider adjunctive probiotic therapy, selecting strains such as Bifidobacterium longum and Lactobacillus rhamnosus, which have demonstrated efficacy in re‑establishing a balanced microbiome and reducing diarrheal frequency. On the pharmacologic front, biologic agents targeting TNF‑alpha, notably infliximab and adalimumab, have been shown to precipitate the closure of many perianal fistulas, while also dampening the upstream inflammatory signals that precipitate pruritus. Complementary to systemic therapy, local measures are indispensable: zinc‑oxide based barrier creams provide a physical shield against moisture, and low‑dose hydrocortisone creams mitigate superficial inflammation without overly suppressing local immunity. Sitz baths, conducted twice daily for fifteen minutes, offer thermally induced vasodilation that promotes tissue healing and alleviates the burning sensation. Dietary modifications, particularly the adoption of a low‑FODMAP regimen, can curtail fermentable carbohydrate intake, thus reducing gas production and stool liquidity, which together are notorious agitators of perianal irritation. In summary, a multi‑modal strategy-integrating systemic biologics, targeted antibiotics, probiotic supplementation, meticulous skin care, and judicious dietary adjustment-constitutes the most comprehensive approach to conquering the insidious itch that shadows Crohn’s disease.
Vivian Annastasia
22 October 2025 - 07:13 AM
Honestly, the whole “just add a barrier cream and you’re fine” narrative feels like a convenient marketing ploy, ignoring the fact that many patients are already juggling a cocktail of immunosuppressants and can’t afford another topical side effect. The underlying immunological turmoil doesn’t magically resolve itself with a dab of zinc oxide. While the recommendations are technically correct, they gloss over the socioeconomic barriers that prevent consistent access to sitz baths or specialized diets. A more nuanced discussion would acknowledge these real‑world constraints rather than offering a one‑size‑fits‑all checklist. 🙃
John Price
22 October 2025 - 08:36 AM
Keep the skin dry and the itch will fade.
Erika Thonn
22 October 2025 - 10:00 AM
i think the itch is like a whisper of the gut, a subtle reminder that the body is trying to comunicate something deeper. sometimes the itich isnt just about the skin it also be about the inflamation, the whole system is intertwined. a simple wash and a good diet might not be enough if the underlying immune storm keep raging. maybe we should look at the issue from a philosophical perspective, ask why our body is in pain, and not just treat the symptom. those thoughts can guide more holistic solutions 😊