Most people will experience low back pain at some point in their lives. It’s not rare-it’s normal. But just because it’s common doesn’t mean it’s always harmless. The real danger isn’t the pain itself, but missing the signs that something serious might be going on. Too many people get an X-ray right away, or assume rest is the answer. Others ignore warning signs until it’s too late. The truth? Most low back pain isn’t caused by a broken spine, tumor, or infection. It’s just muscle strain or joint irritation. But that 1-2% that is serious? You need to catch it fast.
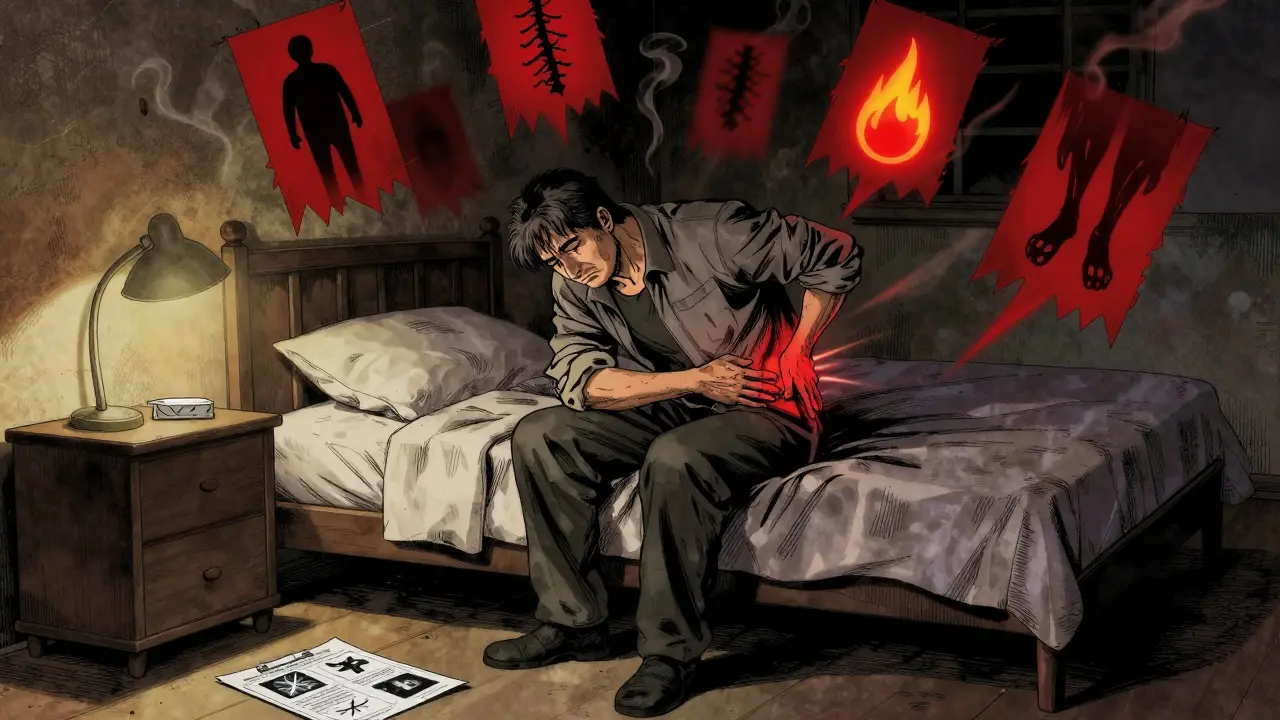
What Are Red Flags, and Why Do They Matter?
Red flags aren’t scary words from a doctor’s script. They’re clinical signals that something more than a pulled muscle might be going on. Think of them like smoke alarms. You don’t panic every time one chirps, but if it’s screaming, you act. In low back pain, red flags point to four main dangers: cancer, fracture, infection, or cauda equina syndrome. These are rare-only 1-2% of cases-but they can change your life forever if missed.Here’s what to watch for:
- History of cancer-If you’ve had cancer before, especially breast, lung, prostate, or kidney, any new back pain needs attention. The risk isn’t high, but the stakes are.
- Unintentional weight loss-Losing 10 pounds or more without trying, especially with back pain, is a major red flag. It’s not about dieting. It’s about your body sending a signal.
- Major trauma-A fall from height, a car crash at speed, or a direct blow to the back. Even if you feel okay now, a fracture can hide in plain sight.
- Pain at night or while resting-If your back pain wakes you up or doesn’t improve when you lie down, it’s not just sore muscles. Inflammatory or cancer-related pain often gets worse when you’re still.
- Fever or chills-Back pain with fever? That’s not a cold. It could be an infection in the spine, like discitis or osteomyelitis.
- Bladder or bowel problems-This is critical. If you can’t control urination, feel like you can’t empty your bladder, or lose control of your bowels, get help now. Same with numbness in your groin or inner thighs-that’s saddle anesthesia. These are signs of cauda equina syndrome, a surgical emergency.
- Weakness in legs-Foot drop, tripping often, or sudden leg weakness that doesn’t go away? That’s nerve damage. Don’t wait.
Here’s the catch: Not every red flag means cancer. Many are nonspecific. A 55-year-old with mild back pain and no other symptoms? Age alone isn’t enough. The 2023 NICE guidelines removed "over 55" as a red flag because it leads to too many false alarms. Same with "age over 50"-a common myth. Studies show age alone has almost no predictive power. The real red flags are the ones tied to actual disease patterns, not just demographics.
When Do You Actually Need an X-Ray or MRI?
Most people don’t need imaging at all. Not even an X-ray. And yet, doctors order them anyway. In the U.S., nearly half of all acute low back pain patients get imaging within the first month-despite guidelines saying it’s unnecessary.The American College of Radiology, the American College of Physicians, and the Canadian Family Physicians Association all agree: If you have low back pain without red flags, and it’s been less than 4 weeks, don’t get imaging. Why? Because 97% of the time, it’s not structural. It’s mechanical. X-rays won’t show a strained ligament. MRIs won’t reveal a muscle spasm. And finding degenerative changes on an MRI in a 40-year-old with pain? That’s normal. It’s like finding wrinkles on a face-you wouldn’t treat wrinkles with surgery.
Imaging is only appropriate when red flags are present:
- Cauda equina syndrome → MRI without contrast, immediately.
- Suspected fracture after trauma → CT scan if neurological symptoms are present; X-ray if no red flags but high-risk mechanism.
- Suspected infection → MRI or bone scan with SPECT/CT. Blood tests like ESR and CRP help too-levels above 20 mm/hr and 10 mg/L, respectively, raise suspicion.
- Suspected cancer → MRI without contrast. It shows soft tissue and bone better than anything else.
For chronic pain (over 12 weeks) without red flags? Still no imaging. X-rays are useless here. They show arthritis or disc space narrowing-but those changes are common in people with no pain at all. A 2019 Canadian guideline says it plainly: "X-rays of the lumbar spine are very poor indicators of serious pathology in chronic low back pain."
And here’s the kicker: Unnecessary imaging leads to more harm. A 2021 study found that patients who got early MRIs for low back pain were 3 times more likely to have surgery-even if their pain improved on its own. Why? Because once you see a bulging disc on an MRI, your brain starts blaming it for everything. You don’t need to see it to fix it.
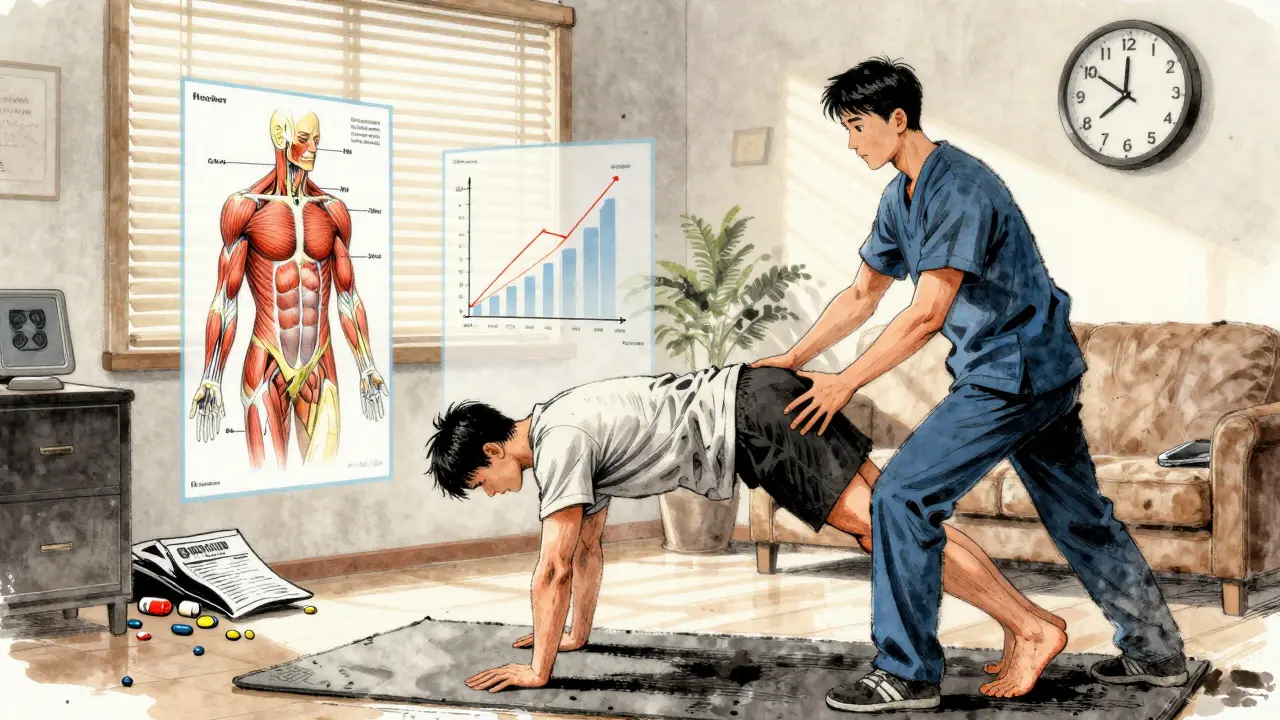
Exercise Therapy: The Only Treatment That Works Long-Term
If you’ve been told to rest, stretch, or get a massage, you’ve heard the wrong advice. Rest doesn’t fix back pain. In fact, it makes it worse. The best treatment for most low back pain isn’t a pill, a needle, or a scan. It’s movement.A 2020 Cochrane Review of 97 studies with nearly 20,000 people found that exercise reduces pain and improves function better than any other non-drug treatment. The average pain reduction? Over 6 points on a 100-point scale. That’s not small. That’s meaningful. And the benefits last. People who stick with exercise for 6 to 12 months still feel better than those who didn’t move.
Not all exercises are equal. Here’s what the evidence supports:
- Motor control exercises-These retrain your deep core muscles (transverse abdominis, multifidus) to stabilize your spine. Think pelvic tilts, bird-dogs, dead bugs. Effect size: 0.61 for pain reduction.
- Graded activity-Start slow, move more each day. No pain, no gain? Wrong. This approach says: move within pain limits. Walk 5 minutes today, 7 tomorrow. Build up. It works better than rest.
- Combined programs-Mix strength, aerobic, and flexibility. Walking, swimming, cycling, and bodyweight squats or planks. Effect size: 0.58.
Here’s how to do it right:
- Start with 2-3 supervised sessions per week for 4-6 weeks. A physical therapist can teach you proper form.
- Progress slowly. Strength training should start at 40-60% of your one-rep max, then go up to 70-85% over 8-12 weeks.
- Add aerobic activity: 20-30 minutes, 3-5 days a week, at 60-80% of your max heart rate. That’s a pace where you can talk but not sing.
- Do it at home. If you only do exercises at the clinic, you’ll quit. Home programs are the key to long-term success.
Adherence is everything. If you do less than half the prescribed sessions, benefits drop by 60%. That’s why consistency beats intensity. Five minutes a day, every day, beats an hour once a week.

Why So Many Doctors Get It Wrong
You’d think guidelines would be followed. But they’re not. A 2022 survey of over 1,200 primary care doctors found that 68% still think "age over 50" is a red flag. That’s wrong. 43% order X-rays for acute back pain without red flags. That’s against every major guideline.Why? Time. Doctors average just 12.7 minutes per back pain visit. The recommended time? 18-22. They don’t have time to screen properly. They don’t have time to explain why imaging won’t help. So they order it. Or they prescribe painkillers. Or they refer you to a specialist who does the same.
There’s a better way. Tools like the "Red Flag Decision Tool" from the International Framework for Red Flags help. It’s a 3-step checklist: 1) Is there a red flag? 2) Is there a high-risk factor? 3) Does the clinical picture fit? It cuts unnecessary imaging by 28% in real clinics.
And the Choosing Wisely campaign-started in 2012-has already reduced inappropriate imaging by over 15% in the U.S. It’s working. But it needs patient awareness. You have to ask: "Do I really need this scan?"
What Comes Next?
The future of back pain care is smarter, not just more tests. AI tools are being trained to spot red flags better than humans. A 2022 study in Nature Digital Medicine showed an AI tool improved diagnostic accuracy from 73% to 89%. That’s huge.Research is also looking at genetic markers and blood biomarkers to predict who’s at risk for serious spine conditions. The SPINE Act of 2022 is funding $15 million for this. In 5 years, we might have a simple blood test that tells you if your back pain is likely benign-or something more.
But right now? The tools you have are enough. Know the red flags. Skip the scan unless you have them. Move. Consistently. Don’t wait for pain to go away. Move through it. Your spine doesn’t need fixing. It needs loading, strengthening, and moving.
Is back pain always a sign of something serious?
No. In fact, 97% of low back pain cases are not serious. They’re caused by muscle strain, joint stiffness, or poor movement patterns. These improve with time and movement. Only 1-2% involve cancer, infection, fracture, or nerve damage-those are the cases that need urgent attention.
Should I get an MRI if my back pain doesn’t improve in a few weeks?
Not necessarily. If you have no red flags-no numbness, weakness, fever, weight loss, or bladder issues-an MRI won’t tell you anything useful. Degenerative changes like disc bulges are common in people with no pain at all. Getting an MRI without a clear reason can lead to unnecessary surgery or anxiety. Stick with exercise and movement for at least 6-8 weeks before considering imaging.
What’s the best exercise for low back pain?
There’s no single "best" exercise, but the strongest evidence supports motor control exercises (like bird-dogs and dead bugs), graded activity (gradually increasing daily movement), and combined programs that include walking, strength training, and light cardio. The key isn’t the type-it’s consistency. Do something every day, even if it’s just 10 minutes.
Can I still exercise if my back hurts?
Yes-within reason. Pain during movement doesn’t mean damage. It means your tissues are sensitive. Avoid sharp, shooting, or nerve-like pain. But mild discomfort (2-4 out of 10) during walking, stretching, or strengthening is normal and safe. The goal is to move without worsening symptoms. If pain spikes above 5/10 or lasts more than 2 hours after exercise, scale back.
When should I go to the ER for back pain?
Go to the ER immediately if you have: sudden loss of bladder or bowel control, numbness in your groin or inner thighs (saddle anesthesia), severe leg weakness, or fever with back pain. These are signs of cauda equina syndrome or spinal infection-both require emergency treatment. Don’t wait for a doctor’s appointment. Call 911 or go to the nearest ER.
Does age make back pain more dangerous?
Not by itself. Age over 50 or 55 used to be considered a red flag, but recent guidelines (including NICE 2023) removed it. Older adults are more likely to have arthritis or disc degeneration-but those changes don’t cause pain on their own. The real danger is if you have cancer history, unexplained weight loss, or trauma. Age alone doesn’t raise your risk of serious spine conditions.