When you hand a patient a prescription for a generic drug, you’re not just giving them a pill-you’re asking them to trust a system they don’t fully understand. Many patients see the difference in color, shape, or size and assume something’s wrong. Others worry they’re getting a cheaper, weaker version. And honestly? It’s not their fault. The system is confusing. But as a provider, you have the power to turn that confusion into confidence.
Patients aren’t resisting generics-they’re resisting uncertainty
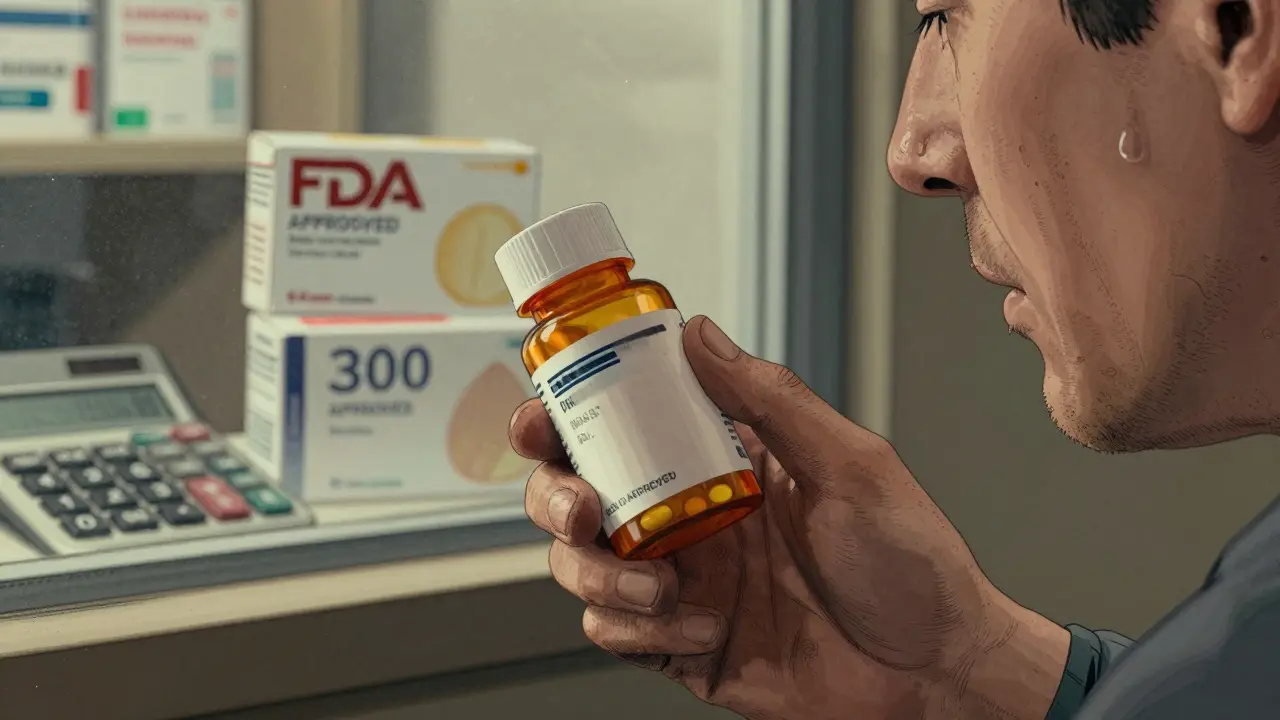
The truth is, 90% of prescriptions filled in the U.S. are generics. They’re not experimental. They’re not second-rate. They’re FDA-approved copies of brand-name drugs that work the same way, at the same dose, with the same active ingredient. The difference? Price. Generics cost 80-85% less. That’s why they save the U.S. healthcare system over $370 billion every year. But here’s the catch: 28% of patients are nervous about switching from brand to generic. And 17% stop taking their medication altogether after the switch-not because it doesn’t work, but because they weren’t told it would. It’s not about the pill. It’s about the story behind it.What makes a generic drug really the same?
Let’s clear up the biggest myth: generic drugs are not cheaper because they’re less effective. They’re cheaper because they don’t need to repeat expensive clinical trials. The FDA requires every generic to prove it delivers the exact same amount of active ingredient into the bloodstream as the brand-name version-within a tight range of 80-125% bioequivalence. That’s not a guess. It’s science. The FDA inspects every manufacturing facility for generics the same way they inspect brand-name makers. The same quality standards. The same purity requirements. The same labeling rules-except for the brand name and logo. So why do they look different? Trademark laws. A pill can’t look identical to the brand version, even if it’s chemically the same. That’s why your generic lisinopril is blue, but the brand is white. That’s why your generic metformin is oval, but the brand is round. It’s not a change in medicine. It’s a change in packaging.Why patients doubt generics-and how to fix it
Most concerns come from three places:- Appearance changes-63% of patient complaints are about pills looking different. One patient told me, “The blue one made me nauseous, but the white one was fine.” Turns out, they’d switched manufacturers twice in three months. The active ingredient didn’t change. The filler did. And that’s okay.
- Efficacy fears-27% worry the drug won’t work as well. But a review of 47 studies involving over 9,000 people found no meaningful difference in outcomes between generics and brand-name cardiovascular drugs.
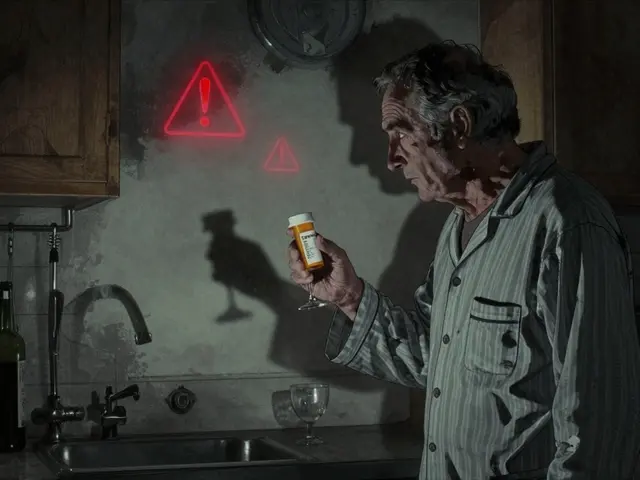
- Previous bad experiences-10% had a bad reaction to a generic from a different manufacturer. This isn’t common, but it’s real. For drugs with a narrow therapeutic index-like warfarin or levothyroxine-switching between generic brands can sometimes require monitoring. That’s not because generics are unsafe. It’s because tiny variations in inactive ingredients can affect absorption in sensitive patients.
The TELL method: A simple framework that works
Pharmacists and providers who use the TELL method see 22% higher adherence at six months. Here’s how it works:- Tell: “This generic has the same active ingredient as your brand-name drug. It’s required by law to work the same way.”
- Explain: “The color and shape are different because of trademark rules. The inactive ingredients-like dyes or fillers-are changed to avoid copying the brand. But they don’t affect how the medicine works.”
- Listen: Don’t assume. Ask, “What’s your biggest concern about switching?” Maybe they had a bad experience. Maybe they’re scared of side effects. Let them say it.
- Link: “This switch could save you $200 a month. That’s money you can use for groceries, transportation, or your next doctor visit. And you’ll still get the same result.”
What to say when they ask the hard questions
Patients will ask the same things over and over. Be ready.“Is this really the same medicine?”
Yes. Same active ingredient. Same strength. Same way it works in your body. The FDA requires it.
“Why does it look different?”
By law, generics can’t look exactly like the brand. It’s a trademark rule, not a safety rule. Think of it like two different brands of aspirin-they’re both acetaminophen, but one’s red, one’s white.
“Is it as strong?”
It’s not weaker. It’s identical in strength. The FDA checks this with blood tests before approving any generic. If it doesn’t match the brand within strict limits, it doesn’t get approved.
“I tried one before and it didn’t work.”
That’s worth exploring. Did you switch manufacturers? Sometimes, changing from one generic to another-even though both are approved-can cause small differences in how your body absorbs it. For most drugs, that’s fine. For some, like thyroid meds or blood thinners, we may need to monitor you more closely. Let’s check your levels.
Use the teach-back method to confirm understanding
Don’t just explain. Ask them to explain it back. Say: “Just so I’m sure I explained this right-can you tell me in your own words why this generic is safe to take?” Studies show this simple technique increases retention by 40%. Patients who can repeat the key points are far less likely to stop taking their meds.Document the conversation
Write down what you said and what they said. Note: “Patient expressed concern about pill appearance. Explained bioequivalence and inactive ingredients. Patient agreed to try generic and will call if side effects occur.” That documentation protects you, helps future providers, and shows the patient you took their concern seriously.
When to consider authorized generics
Some patients still won’t budge. For them, there’s an option: authorized generics. These are brand-name drugs sold under a generic label-same manufacturer, same pill, same packaging, just cheaper. About 37% of top-selling brand drugs now have authorized generic versions. If a patient says, “I only trust the brand,” ask: “Would you be open to trying the same pill, just without the brand name on it?” Often, that’s enough.The bigger picture: Why this matters
This isn’t just about saving money. It’s about access. A Medicare patient in Texas told me she skipped her cholesterol meds for six months because the brand cost $300 a month. She switched to generic rosuvastatin. It cost $12. She’s now on track. Her LDL dropped 40%. That’s the real impact. Generics aren’t a compromise. They’re a solution. And when patients understand that, adherence goes up, hospitalizations go down, and lives get better.What’s next for generics?
The FDA is now funding video-based education tools to help patients understand generics. Early results show combining a short video with a conversation increases acceptance by 31%. More biosimilars-complex generics for biologic drugs like insulin or rheumatoid arthritis treatments-are coming too. That means more conversations ahead. But the core message won’t change: Generics work. They’re safe. And you deserve to take them without fear.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they deliver the same amount of medicine into the bloodstream at the same rate-within strict bioequivalence limits. A review of 47 studies involving over 9,000 patients found no clinically significant difference in effectiveness between generics and brand-name drugs for cardiovascular conditions.
Why do generic pills look different from brand-name ones?
By U.S. trademark law, generic drugs cannot look identical to brand-name versions, even if they’re chemically the same. This means the color, shape, size, or markings may differ. These changes are only in inactive ingredients-like dyes or fillers-which do not affect how the drug works. The active ingredient, which is what treats your condition, remains unchanged.
Can switching to a generic cause side effects?
For most people, no. But some patients may notice minor differences if they switch between different generic manufacturers, especially with drugs that have a narrow therapeutic index-like levothyroxine, warfarin, or certain seizure medications. These drugs require very precise blood levels. While all approved generics meet FDA standards, small variations in inactive ingredients can affect absorption in sensitive individuals. If side effects occur after switching, monitor symptoms and contact your provider. In some cases, sticking with one generic manufacturer or using an authorized generic helps.
Are generic drugs made in the same quality facilities as brand-name drugs?
Yes. The FDA inspects all manufacturing facilities-brand and generic-using the same standards. In fact, many brand-name companies also produce generic versions of their own drugs. The FDA checks for purity, potency, and consistency in every batch. There is no evidence that generic drugs are made in lower-quality facilities.
Why do insurance plans push generics so hard?
Because generics save patients and insurers money-without sacrificing effectiveness. Generics make up 90% of prescriptions but only 23% of drug spending. On average, a generic drug costs 80-85% less than its brand-name counterpart. Insurance companies encourage generics because they help patients afford their medications, which leads to better adherence and fewer hospital visits.
What’s an authorized generic, and should I consider it?
An authorized generic is the exact same drug as the brand-name version, made by the same company, but sold under a generic label. It has the same inactive ingredients, same appearance, and same packaging-just without the brand name. It’s often cheaper than the brand and may help patients who are reluctant to switch to a generic that looks different. About 37% of top-selling brand drugs now have authorized generic versions available.




Arjun Seth
15 January 2026 - 06:15 AM
Look, I’ve seen people panic over a blue pill instead of white-like it’s witchcraft. It’s not. It’s science. Stop letting Big Pharma scare you with colors and shapes. The FDA doesn’t lie. If it’s generic, it works. Period.
Mike Berrange
17 January 2026 - 01:32 AM
Actually, the bioequivalence range of 80–125% is not ‘identical’-it’s a 45% variance window. That’s not science-it’s a loophole. And don’t get me started on how many generic manufacturers are in India and China with zero FDA oversight. You think they’re inspecting every batch? Please.
Dan Mack
18 January 2026 - 10:21 AM
They’re lying. The FDA is owned by Big Pharma. The ‘same active ingredient’? Yeah right. They swap in fillers that cause anxiety, insomnia, weight gain-you name it. I switched to generic lisinopril and my blood pressure spiked. They don’t want you to know the truth: generics are testing grounds for corporate experiments.
Amy Vickberg
19 January 2026 - 04:29 AM
I love how this article doesn’t just tell you what to say-it tells you how to listen. So many providers rush through the explanation and miss the real issue: patients feel dismissed. When you actually sit with someone’s fear, even for five minutes, they feel seen. That’s the magic. Not the pill. The person.
Ayush Pareek
20 January 2026 - 21:34 PM
As someone who’s seen patients in rural India choose between food and medicine, I can tell you-generics aren’t a luxury. They’re survival. If a man with diabetes can afford his metformin because it costs $2 instead of $200, he’ll live. And that’s worth more than any brand logo.
Nishant Garg
21 January 2026 - 10:31 AM
You know what’s wild? Back home in Delhi, we’ve got generics made by the same factories that make the brand names-just repackaged. The pill? Identical. The box? Different. The cost? A tenth. But here in the States, people act like it’s a knockoff Rolex. It’s not. It’s the same watch, just without the gold plating and the $500 price tag.
Nicholas Urmaza
22 January 2026 - 12:33 PM
Let’s be clear-this isn’t about trust. It’s about accountability. If you’re prescribing generics, you owe your patient clarity. Not a pamphlet. Not a handout. A conversation. You’re not a salesperson. You’re a healer. So act like it. Stop treating patients like they’re stupid. They’re just uninformed. Fix that.
Sarah Mailloux
24 January 2026 - 01:48 AM
I had a patient cry because she thought her generic antidepressant wasn’t working. Turns out she’d switched manufacturers three times in six months. We stuck her with one brand and she said, ‘I feel like myself again.’ Not because the drug changed. Because she finally felt stable. That’s the real win.
Nilesh Khedekar
24 January 2026 - 19:05 PM
Oh sure, ‘it’s the same pill’-until you’re the one who got the generic that gave you migraines for a month. Then suddenly, ‘science’ doesn’t sound so comforting. And yeah, I know the FDA says it’s fine. But I’ve seen people get sick because no one told them to stick with one maker. You think that’s ethical? I don’t.
Jami Reynolds
26 January 2026 - 12:44 PM
Did you know that 60% of generic drugs are manufactured in countries with zero transparency? The FDA inspects less than 2% of foreign facilities annually. So when you say ‘same standards,’ you’re trusting a system that’s barely watching. This isn’t medicine-it’s a gamble.
Amy Ehinger
27 January 2026 - 20:43 PM
I used to be terrified of generics too-until I started taking them for my thyroid. I switched from Synthroid to a generic, then to another generic, then back. I tracked my labs. My TSH stayed within 0.5 points every time. I didn’t feel different. My doctor didn’t even notice. Turns out, the fear was way worse than the pill. And now? I save $180 a month. I’m not a guinea pig. I’m just a person who wants to live without going broke.