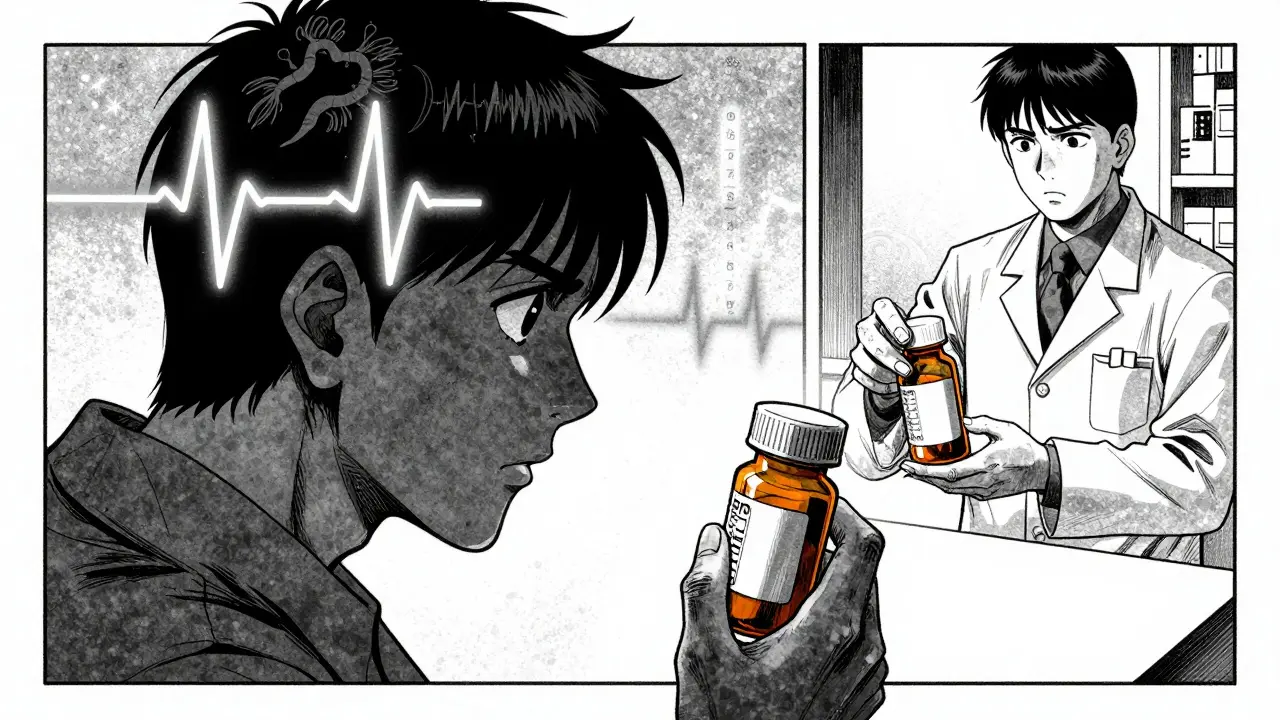
When you pick up a prescription, you might see two options: the brand-name drug you’ve heard of, or a cheaper generic version. The price difference can be huge-sometimes 80% less. But the big question hanging over your mind is simple: are generic drugs as safe as brand names? The answer isn’t just yes or no. It’s layered, backed by data, and shaped by real-world use.
What Makes a Generic Drug a Generic Drug?
A generic drug isn’t a copycat. It’s required by law to contain the exact same active ingredient, in the same strength, same form (pill, injection, etc.), and same way of getting into your body as the brand-name version. The U.S. Food and Drug Administration (FDA) doesn’t just accept claims-it demands proof. Before a generic hits the shelf, manufacturers must show bioequivalence. That means the drug gets absorbed into your bloodstream at nearly the same rate and to the same extent as the brand.
How do they prove it? Through pharmacokinetic studies. They measure two key things: Cmax (the highest concentration in your blood) and AUC (how much of the drug your body absorbs over time). The FDA requires that the 90% confidence interval for these measurements falls between 80% and 125% of the brand-name drug. That’s not a wide gap-it’s tight. It means your body handles the generic almost identically to the brand.
And yes, generics have different inactive ingredients-fillers, dyes, coatings. These don’t affect how the drug works, but they can cause rare allergic reactions. That’s why some people notice a change in pill shape or color when switching. But the active ingredient? Identical.
The Evidence: Do Generics Work the Same?
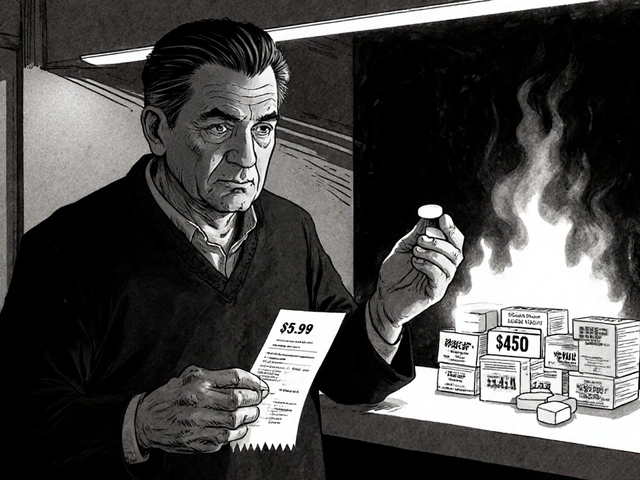
Let’s look at the numbers. In 2023, generics made up 90% of all prescriptions filled in the U.S.-over 6 billion prescriptions. But they only accounted for about 18% of total drug spending. That’s billions saved every year. And if generics were unsafe or ineffective, that number wouldn’t hold.
A 2020 study published in Nature Scientific Reports analyzed over 1.5 million patients in Austria who were taking 17 different medications, including blood pressure drugs, antidepressants, and statins. Researchers compared outcomes between brand and generic users. After adjusting for age, health status, and other factors, they found that patients taking generics had fewer deaths in 10 of the 17 drugs studied. For heart-related events, the difference was even starker: generic users had nearly 40% fewer major cardiac events than those on brand names.
How could cheaper drugs lead to better outcomes? One theory: because generics cost less, patients are more likely to take them consistently. Missed doses of blood pressure or cholesterol meds are a major cause of hospitalizations. Lower cost = better adherence = better results.
When Things Don’t Go as Expected
But it’s not perfect. There are documented cases where patients report feeling worse after switching from brand to generic. These aren’t myths-they’re real experiences, especially with certain drugs.
Thyroid medication, like levothyroxine, is a prime example. Small changes in hormone levels can cause fatigue, weight gain, or heart palpitations. In 2017, a Canadian study found that after generic versions of thyroid drugs became available, more older adults were hospitalized for thyroid-related issues. One patient reported her TSH level jumped from 1.2 to 8.7 after switching to a generic-despite taking the same dose. That’s a dramatic shift.
The American Thyroid Association now recommends sticking with one version-either brand or generic-and not switching back and forth. Why? Because even tiny differences in how the drug dissolves in the gut can affect absorption. For drugs with a narrow therapeutic index-where the difference between a helpful dose and a harmful one is small-consistency matters.
Same goes for epilepsy drugs like phenytoin or carbamazepine. A 2013 review in the Journal of Clinical Pharmacy and Therapeutics found that about 30% of patients switched from brand to generic reported side effects or loss of seizure control. In some cases, patients had to switch back to the brand to regain stability.
And then there’s warfarin, a blood thinner. A 1% change in concentration can mean the difference between a clot and a bleed. While most generic warfarin performs fine, the FDA and doctors still recommend sticking with one version if possible.
What Do Pharmacists and Patients Really See?
Pharmacists are on the front lines. A 2021 survey by the National Community Pharmacists Association found that 67% of pharmacists had seen patients complain about reduced effectiveness or new side effects after a generic switch. The most common complaints? Psychiatric meds, seizure drugs, and thyroid meds.
But here’s the flip side: a 2022 Consumer Reports survey of over 10,000 people found that 89% reported no difference between brand and generic drugs. Only 11% noticed any change-and even then, many said they couldn’t tell if it was the drug or something else in their life.
And the FDA’s own adverse event database (FAERS) from 2018 to 2022 showed no meaningful difference in reported side effects per million prescriptions between generics and brands. For 15 commonly used drugs, generics had 12.7 reports per million; brands had 13.2. That’s practically the same.
Why the Confusion? It’s Not the Drug, It’s the Switch
Here’s a key insight: most problems aren’t caused by generics being inferior. They’re caused by switching.
When you switch from one brand to another brand, you don’t panic. But when you switch from a brand to a generic, your brain says, “This is different.” That’s the nocebo effect-the opposite of placebo. You expect to feel worse, so you notice every little change.
Studies show that patients who know they’re taking a generic report more side effects than those who don’t know-even when they’re taking the exact same pill.
Also, not all generics are made the same. One manufacturer’s version might dissolve slightly faster than another’s. That’s why doctors sometimes write “Dispense as Written” on prescriptions-for drugs where consistency is critical.

What Should You Do?
For most people: take the generic. It’s safe, effective, and saves money. Statins, antibiotics, blood pressure meds, antidepressants-generics work just as well.
But if you’re on one of these:
- Levothyroxine (thyroid)
- Warfarin (blood thinner)
- Phenytoin, carbamazepine (seizure meds)
- Some psychiatric drugs like lithium or cyclosporine
Then be cautious. If you’ve been stable on a brand, stay on it. If you’re on a generic and doing fine-don’t switch. If you start feeling off after a switch, talk to your doctor. Get a blood test. Don’t assume it’s all in your head.
Ask your pharmacist: “Is this the same version I’ve been taking?” If you’re on a narrow therapeutic index drug, try to stick with one manufacturer. Consistency beats savings when your health is on the line.
The Bottom Line
Generic drugs are not second-rate. They’re held to the same standards as brand names. The science overwhelmingly supports their safety and effectiveness. For 9 out of 10 people, switching to a generic is a smart, safe move.
But for a small group-those on drugs where tiny changes matter-the story is more nuanced. The problem isn’t the generic itself. It’s the switch. And that’s something you can control.
Don’t fear generics. Understand them. Ask questions. Stay consistent. And remember: the goal isn’t to pick the most expensive drug. It’s to find the one that keeps you healthy-and keeps you taking it.





Jennifer Littler
11 January 2026 - 05:33 AM
As someone who’s been on levothyroxine for 12 years, I’ve switched between generics and brand twice. The first time, my TSH spiked to 9.3-felt like a zombie. Second switch back to Synthroid? Back to normal in 3 weeks. It’s not placebo. The dissolution profiles vary between manufacturers, and for narrow therapeutic index drugs, that’s not trivial. The FDA’s 80–125% bioequivalence window is statistically acceptable but clinically dangerous for some of us.
Doctors don’t always know this. Pharmacists get pressured to switch. Patients get stuck in the middle. It’s not about cost-it’s about consistency.
Sam Davies
12 January 2026 - 17:17 PM
Oh wow. A 900-word essay on pills. Who knew generics were so… dramatic? Next up: ‘The Hidden Truth About Aspirin: Why Your Local Pharmacy Is Lying To You.’
Look, if your thyroid is so fragile that a different filler makes you hallucinate, maybe don’t self-diagnose via Reddit. Also, 18% of drug spending? Congrats, you just proved capitalism works. Now go touch grass.
Alfred Schmidt
14 January 2026 - 05:16 AM
YOU’RE ALL IGNORANT. I’ve been on warfarin for 15 years. I switched to generic-got a DVT. I switched back-got my INR back to 2.4. The FDA doesn’t test for long-term bioequivalence. They test for 24-hour AUC. That’s not enough. My blood clots or bleeds based on which generic batch I get.
And no, it’s not ‘in my head.’ I have lab results. I have hospital records. I have a scar from a bleed that nearly killed me. And now you’re telling me to ‘just take the generic’? You don’t get to say that to people who’ve nearly died because of your complacency.
Priscilla Kraft
14 January 2026 - 08:10 AM
Thank you for this incredibly thoughtful breakdown 🙏
I’m a nurse and I see this all the time-patients terrified to switch, then relieved when they realize they feel the same. But the ones on thyroid meds? Yeah, they need to stick with one. I always check the manufacturer name on the bottle now. If it changes, I flag it.
Also, the nocebo effect is REAL. I had a patient swear her generic antidepressant made her ‘numb’-switched back to brand, same pill, different label-she cried saying she ‘felt like herself again.’ Turned out it was the color of the pill. 🤦♀️
So yes-generics are safe. But context matters. Always listen to your body. And your pharmacist.
Michael Patterson
14 January 2026 - 19:58 PM
Look, I’m not a doctor but I read a lot of medical journals and I’ve got a cousin who works at Pfizer so I know things. The FDA’s bioequivalence standards are a joke. 80-125%? That’s like saying a car engine that gets 25 mpg is ‘equivalent’ to one that gets 35 mpg because it’s still in the same ballpark. But no one would buy a car that might stall at 70 mph. Why are we okay with that for our brains and hearts?
Also, generics are made in India and China. I saw a video of a factory in Hyderabad where they’re dumping chemical waste into a river next to the pill production line. That’s not science, that’s a horror movie. And the FDA doesn’t inspect every batch. They inspect one per year. ONE. PER. YEAR.
So yeah, maybe your statin’s fine. But your seizure med? Your blood thinner? You’re playing Russian roulette with your life. And you’re too lazy to pay $10 more. I’m not judging. I’m just saying.
Matthew Miller
16 January 2026 - 13:18 PM
Wow. So you wrote a 1000-word article to say ‘some people feel weird after switching’? Congrats, you’ve discovered that humans are sensitive to change.
Here’s the real issue: the pharmaceutical industry wants you to fear generics so they can keep charging $1000 for a pill that costs $0.50 to make. The entire system is rigged. The ‘brand loyalty’ myth is a marketing scam.
And if you’re one of the 0.1% who actually has a problem? Then don’t switch. But don’t let your anecdote become a national panic. The data is clear: generics save lives. Period. Stop being a fearmonger.
Adewumi Gbotemi
16 January 2026 - 20:00 PM
Here in Nigeria, we don’t even have brand drugs most times. Only generics. And we live. My uncle takes blood pressure generic for 10 years, no problem. My sister take epilepsy generic, no seizure. Maybe the problem is not the drug. Maybe the problem is we think expensive = better. But in Africa, we know: if it works, it works. No need to pay extra for logo.
Sean Feng
16 January 2026 - 21:00 PM
Generic drugs work. End of story.
Christian Basel
16 January 2026 - 21:57 PM
Let’s be real-the entire debate is a distraction. The real issue isn’t whether generics are safe. It’s that we’ve outsourced our entire pharmaceutical supply chain to countries with zero regulatory transparency. The FDA approves generics based on paperwork, not audits. And the active ingredient? It’s often synthesized in a lab in Bengaluru, shipped to a facility in Guadalajara, then pressed into pills with dyes that aren’t even FDA-approved for ingestion.
And yet we’re supposed to trust that the 80-125% bioequivalence window is enough? That’s not science. That’s corporate theater.
Meanwhile, the real cost isn’t the pill-it’s the ER visits from patients who switch and then can’t afford to switch back. We’re not saving money. We’re shifting the burden.
Jason Shriner
18 January 2026 - 08:15 AM
So… we’re all just… floating in a sea of chemical uncertainty?
Is this what modern medicine has come to? A lottery ticket with your heartbeat?
I mean, I get it. The system’s broken. But I’m just sitting here wondering… if the pill I take to stay alive is made by someone who doesn’t even speak English… how do I know it’s not just… glitter in a capsule?
And why does it feel like we’re all just one bad batch away from becoming a statistic?
…I’m going to go stare at my pill bottle now.
Vincent Clarizio
19 January 2026 - 22:41 PM
You think this is about pills? No. This is about control.
Who gets to decide what’s ‘safe’? The FDA? The CEOs? The pharmacists paid by insurance companies to switch your meds?
Think about it: you’re not being asked to choose between two drugs. You’re being asked to choose between trust and fear.
And the system wants you afraid. Because if you’re afraid, you’ll pay more. You’ll stay loyal. You’ll stop asking questions.
But here’s the truth: your body doesn’t care about the label. It only cares about what’s in the capsule.
So if you’re stable on a generic? Stay. If you’re stable on a brand? Stay. But don’t let someone else’s profit margin dictate your health.
That’s not medicine. That’s capitalism with a stethoscope.
Alex Smith
20 January 2026 - 09:35 AM
Interesting thread. I’m a pharmacist in rural Ohio. We switch people to generics all the time.
Here’s what I’ve learned: 95% of people don’t notice a difference. But the 5% who do? They’re usually on thyroid, seizure, or psych meds.
My rule? If the patient says ‘I feel different,’ I don’t argue. I don’t say ‘it’s placebo.’ I check labs. I switch them back.
And I always write ‘Dispense as Written’ on scripts for levothyroxine and warfarin.
Because sometimes, the most ethical thing you can do is ignore the cost-saving algorithm and just… listen.
Madhav Malhotra
20 January 2026 - 15:30 PM
My cousin in Mumbai takes generic metformin for diabetes. Costs $2/month. He’s been stable for 8 years. His doctor never even mentioned brand names.
Here in India, we don’t have the luxury of choice. But we do have trust-in doctors, in science, in consistency.
Maybe the problem isn’t generics. Maybe it’s that we’ve turned medicine into a brand war.
What matters is: does it work? Does it keep you alive?
Then why are we arguing about the logo?
Jennifer Littler
20 January 2026 - 16:22 PM
Just to clarify: I’m not anti-generic. I’m pro-consistency.
My endocrinologist now refuses to switch me unless I get a blood test first. That’s the gold standard. Not ‘trust the system.’ Not ‘save money.’ Just: test, monitor, adjust.
That’s what real medicine looks like.