Transferring a prescription shouldn’t feel like a game of telephone. One wrong digit on a label, one missed refill, one truncated dose - and someone could end up in the ER. In 2026, with digital systems everywhere, you’d think this would be simple. But it’s not. Medication errors linked to poor prescription transfers still cause 7,000 deaths each year in the U.S., according to the Institute of Medicine. The good news? There are clear, enforceable rules now - and if you follow them, you can avoid the most common mistakes.
Why Prescription Label Accuracy Matters More Than You Think
A prescription label isn’t just a piece of paper with instructions. It’s a safety contract between the pharmacist, the prescriber, and you. The FDA estimates that standardized, accurate labeling could prevent 1.5 million adverse drug events annually. That’s not theoretical. In 2022, the National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) analyzed over 2,300 medication errors and found that trailing zeros - like writing ‘1.0 mg’ instead of ‘1 mg’ - caused tenfold dosing errors. That’s the difference between a safe dose and a lethal one.Another hidden danger? Units. If a label says ‘.4 mg’ instead of ‘0.4 mg’, someone might read it as ‘4 mg’. That’s a 10x overdose. That’s why federal rules now require leading zeros for doses under 1 - always write ‘0.4’, never ‘.4’. And no abbreviations. ‘HCTZ’ for hydrochlorothiazide? Out. ‘MOM’ for magnesium oxide mixture? Gone. Write it out. Full names. No shortcuts.
The DEA’s 2023 Rule: What Changed for Controlled Substances
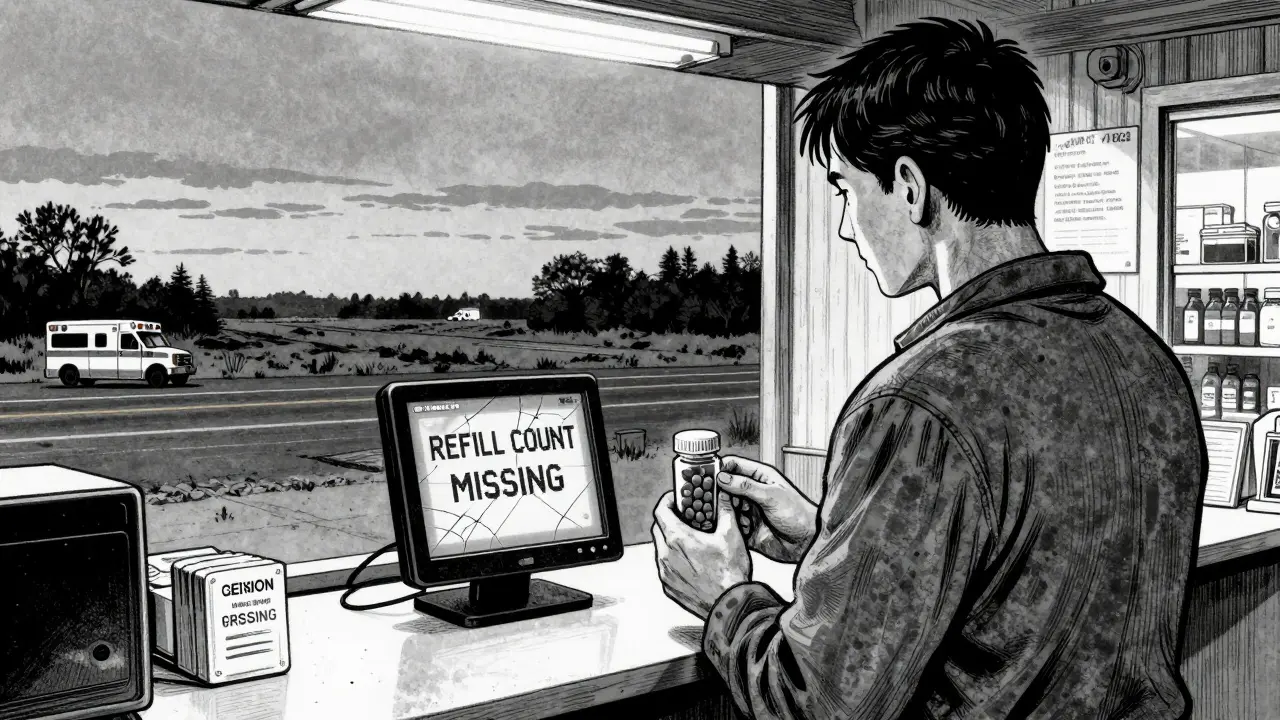
Before August 2023, you couldn’t transfer a Schedule II prescription - like oxycodone or fentanyl - between pharmacies at all. Not even electronically. That meant if you moved or your pharmacy closed, you were stuck. The DEA changed that. Now, you can transfer Schedule II-V controlled substances one time electronically between retail pharmacies. But here’s the catch: it has to be electronic only. No faxing. No phone calls. No handwritten notes.For Schedule III-V drugs - like codeine cough syrup or anabolic steroids - you can transfer up to the number of refills left on the original prescription. But the data must stay untouched. Every field must transfer exactly as it appears: patient name, drug name, strength, quantity, directions, prescriber, pharmacy info, refill count, and the date it was first filled. If any part is missing, cut off, or changed - the transfer is invalid. The pharmacy can’t fill it. And if they do, they’re breaking federal law.
What Goes on the Label - The Exact Requirements
Federal law (21 CFR § 201.100 and § 1306.13) says every prescription label must include these nine things:- Patient’s full name
- Drug name (generic or brand, but spelled out)
- Strength in metric units (e.g., 5 mg, not 5 grains)
- Dosage form (tablet, capsule, liquid)
- Quantity dispensed
- Directions for use (e.g., “Take one tablet by mouth twice daily”)
- Prescriber’s full name
- Prescription number
- Date issued
- Number of refills allowed
- Pharmacy name, address, and phone number
That’s it. No extra fluff. No marketing. No tiny fonts. The label must be readable without magnification. And if it’s a controlled substance, the pharmacy must also note on the electronic record: “Transferred from [Pharmacy Name], DEA #XXXXXXX, on [Date], by [Pharmacist Name].” The receiving pharmacy must add: “Received via transfer from [Original Pharmacy].” No exceptions.
How Electronic Transfers Work - And Why Faxing Is Risky
The gold standard for transfers is the NCPDP SCRIPT standard, version 2017071 or higher. Pharmacies using this system have 98.7% data accuracy, according to a 2022 University of Florida study. Fax transfers? Only 82.3% accurate. Phone transfers? Down to 76.1%. Why? Because humans mishear. Humans misread. Humans type wrong numbers.Here’s how it works in practice:
- You call or visit the new pharmacy and ask to transfer your prescription.
- They verify your identity and the prescription details.
- Their system sends a secure electronic request to your old pharmacy.
- The old pharmacy checks: Is this prescription still valid? Are there refills left? Is it a Schedule II? (Only one transfer allowed.)
- If all checks pass, they send the full, unaltered data - including refill history - to the new pharmacy.
- The new pharmacy adds the transfer notation, prints the label, and dispenses.
Important: If you’re transferring a Schedule II prescription, you can’t refill it after the transfer. It’s used up. That’s why you need to confirm the new pharmacy has the drug in stock before you request the transfer. Otherwise, you’re stuck waiting days for a new prescription from your doctor.
State Rules Still Matter - And They’re Not All the Same
The DEA rule standardized electronic transfers nationally, but states still have their own layers. Wisconsin requires the receiving pharmacy to write the transferring pharmacy’s name, address, and DEA number on the back of the invalidated prescription. Massachusetts requires the transfer record to include the date of the original fill and the first dispensing date. California, after its 2022 law allowing outsourcing facilities to dispense prescriptions, saw 23% of transfers fail because patients didn’t check if the pharmacy carried the drug.That’s why you can’t assume one rule fits all. If you’re moving across state lines, call the new pharmacy first. Ask: “Do you accept electronic transfers from out-of-state pharmacies? Do you have my medication in stock? Can you confirm the refill count?” Don’t wait until you’re out of pills.
What Patients Can Do to Prevent Errors
You’re not just a passive recipient. You’re a critical checkpoint.- Always verify the label when you pick up your prescription. Does the drug name match what your doctor prescribed? Is the dose correct? Is the refill number right?
- Never assume the new pharmacy has your medication. Call ahead. Ask for the exact brand or generic name.
- Don’t transfer on a Friday if you’re out of pills. Pharmacies close on weekends. If you wait until the last minute, you might go without.
- Ask for a printed copy of your prescription label. Keep it. Compare it to the bottle. If something looks off - even a decimal point - speak up.
- Use the same pharmacy whenever possible. Consistency reduces errors. If you’re using multiple pharmacies, you’re increasing your risk.
One Reddit user shared a story from October 2023: they transferred a Schedule IV anxiety med, didn’t check stock, and ended up with a 5-day gap. Their panic attack returned. That’s not rare. It’s predictable.
How Pharmacies Are Fixing the System - And Where They’re Still Falling Short
Chain pharmacies like CVS and Walgreens now use barcode scanning and automated label verification systems. A 12-hospital study published in JAMA Internal Medicine found barcode use reduced dispensing errors by 41%. Many now use AI tools that scan for trailing zeros, missing leading zeros, or ambiguous abbreviations before the label even prints.But independent pharmacies? They’re struggling. In a 2023 National Community Pharmacists Association survey, 67% cited system interoperability as their biggest challenge. Their software doesn’t talk to the big pharmacy networks. The result? Data gets truncated. Refill counts disappear. Directions get cut off.
And rural pharmacies? Only 41% are connected to electronic transfer networks, according to the National Rural Health Association. That’s why patients in those areas have a 15% higher rate of prescription abandonment - they just give up after too many failed transfers.
What’s Coming in 2025 - The FDA’s Patient Medication Information Rule
By 2025, the FDA’s new Patient Medication Information (PMI) rule will require all prescription labels to follow a standardized format. The goal? Make labels so clear that even someone with low health literacy can understand them. The label will be printed on paper by default (not just digital). It will include:- Plain language instructions (“Take one pill every 12 hours” instead of “Q12H”)
- Warning icons for high-risk drugs
- Color-coded sections for dosage, warnings, and storage
- QR codes linking to video instructions (optional, patient-requested)
Early adopters report implementation costs between $12,500 and $18,750 per location. But the payoff? The FDA predicts this will cut medication errors caused by label confusion by 30%. Dr. Michael Cohen of ISMP says it’s the biggest step forward since the 2010 EPCS rule.
Final Checklist: Your 5-Point Safety Plan
Before you transfer any prescription - controlled or not - run through this:- Confirm the new pharmacy carries the exact medication - brand or generic.
- Check how many refills remain - especially for Schedule II drugs (only one transfer allowed).
- Ask if they use NCPDP SCRIPT 2017071 or higher - this ensures full data transfer.
- Verify the label when you pick it up - compare it to your old one.
- Report any mismatch immediately - even a typo in the dose number.
Prescription transfers are no longer a paperwork chore. They’re a safety system. And when done right, they keep people alive.





steve rumsford
7 January 2026 - 22:43 PM
This post should be mandatory reading for every pharmacist and patient. I’ve seen a friend almost die because a label said ‘.5 mg’ instead of ‘0.5 mg’. No exaggeration. That decimal point nearly killed her. We’re talking about lives here, not paperwork.
Andrew N
9 January 2026 - 03:29 AM
Actually, the FDA estimate of 1.5 million adverse events is outdated. The 2023 CDC report shows it’s closer to 1.8 million when you factor in outpatient errors from non-DEA-regulated transfers. Also, trailing zeros aren’t the only issue-missing spaces between numbers and units (like ‘5mg’ vs ‘5 mg’) cause misreads too. You missed that.
Aparna karwande
9 January 2026 - 05:20 AM
India has been doing this right for decades. We never use abbreviations. We write ‘Hydrochlorothiazide’ in full. We never write ‘MOM’-that’s child’s play. And we print labels in bold 14-point font. Why? Because we respect life. You Americans treat prescriptions like fast food orders. It’s embarrassing. Our system works. Yours doesn’t.
Jessie Ann Lambrecht
9 January 2026 - 13:51 PM
Thank you for this. I’m a pharmacist in rural Ohio, and I see this every day. People show up with no refills, no contact info, and no clue about their meds. I’ve started printing a one-page safety sheet with every transfer-simple icons, plain language, and a checklist. Patients love it. And yes, I’ve had to say ‘no’ to a transfer because the label said ‘.25 mg’-and I’m proud of that. This system saves lives. Don’t take shortcuts.
Christine Joy Chicano
11 January 2026 - 08:26 AM
One thing not mentioned: the role of pharmacy technicians in transfer errors. In many stores, techs handle the initial data entry. If they miss a refill count or miskey a dose, the pharmacist might not catch it until the patient is already holding the bottle. Training is inconsistent. Standardization needs to include techs-not just pharmacists.
Adam Gainski
11 January 2026 - 12:35 PM
I’ve been transferring prescriptions for my mom since she had her stroke. The system is a mess. One time, the new pharmacy said they got the transfer, but the label had the wrong strength. I called the old pharmacy-they said they sent it correctly. Turned out the system glitched. I had to fax a copy (which I hate) just to get her meds. This needs to be foolproof. We’re not asking for magic. Just consistency.
Sai Ganesh
12 January 2026 - 22:38 PM
In India, we don’t have the same infrastructure, but we have something better: community trust. My uncle’s pharmacy still writes prescriptions by hand, but everyone knows the pharmacist. If there’s a doubt, they call the doctor. No system replaces human care. Maybe the answer isn’t just tech-it’s connection.
Paul Mason
14 January 2026 - 08:11 AM
Wow. I just transferred my dad’s blood pressure med. I didn’t check the label. I’m an idiot. I just assumed. Now I’m terrified. I’ll go back tomorrow and check. Seriously, folks-read the label. Don’t be like me.
LALITA KUDIYA
16 January 2026 - 03:30 AM
Thank you for writing this. I’ve been scared to transfer my anxiety med for months because I don’t trust the system. Now I know what to ask. I’ll call the pharmacy tomorrow. You made me feel less alone.