Fluoroquinolone Tendon Risk Calculator
Your Risk Factors
How This Works
This tool estimates your relative risk of tendon rupture based on key factors from clinical studies. Your risk is calculated relative to a healthy person under 60 taking ciprofloxacin with normal kidney function.
Important: This is a general estimate only. Individual risk can vary significantly. The FDA warns that tendon rupture can occur within 48 hours of starting fluoroquinolones.
Risk Assessment
Fluoroquinolones Can Break Tendons - Even If You’re Not on Steroids
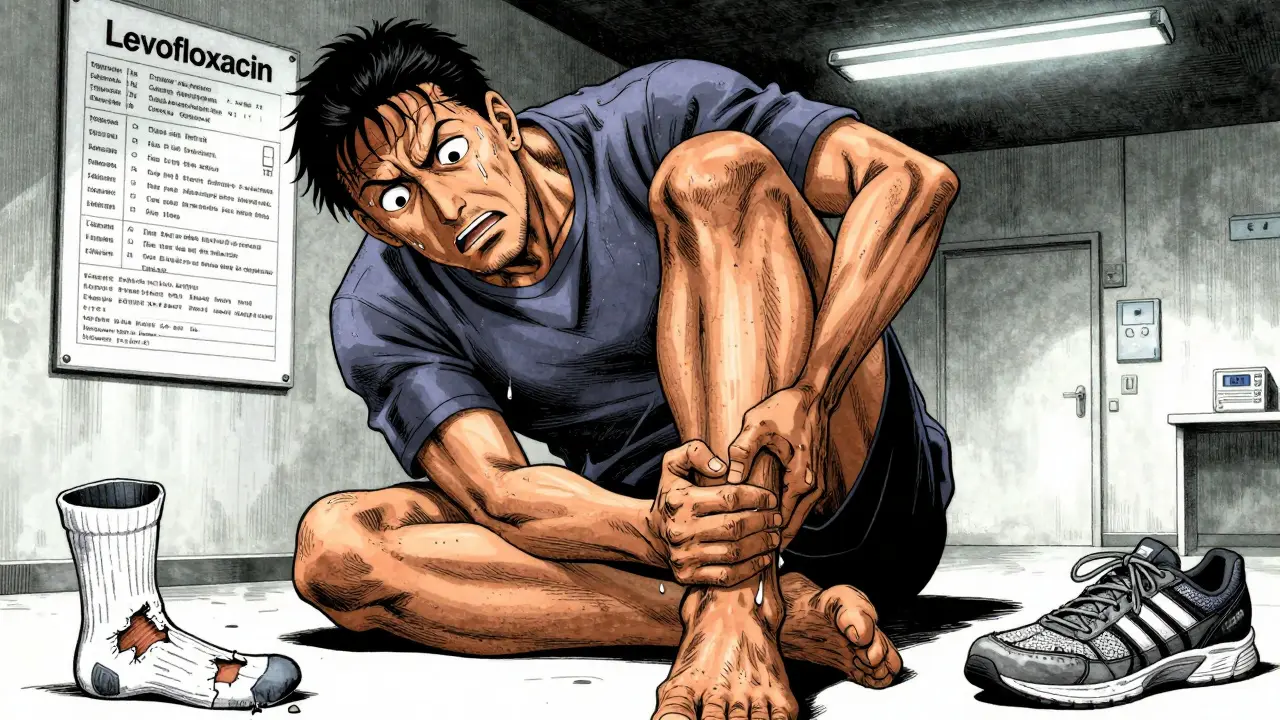
You take an antibiotic for a urinary tract infection or a stubborn sinus infection. A few days later, your heel starts aching. You think it’s just sore from walking too much. But it’s not. It’s your Achilles tendon - and it could tear completely within days. This isn’t rare. It’s a known, documented danger tied to a class of antibiotics called fluoroquinolones.
Many people hear about the risk and assume it’s only a problem if you’re also taking steroids. That’s what the warnings focus on. But here’s the truth: fluoroquinolones alone are enough to cause tendon rupture. And NSAIDs? They don’t make it worse. At least, not according to the science.
Which Fluoroquinolones Are Dangerous?
Not all fluoroquinolones are created equal. The class includes ciprofloxacin, levofloxacin, moxifloxacin, and others. But their risk profiles are wildly different.
Levofloxacin is the big red flag. A 2022 study in BMJ Open found people taking levofloxacin had a 120% higher risk of Achilles tendon rupture compared to those not taking it. That’s not a small increase. It’s nearly triple the baseline risk. And it’s not just the Achilles - rotator cuff tears also went up by 16%.
Meanwhile, ciprofloxacin and moxifloxacin? Multiple studies show no significant increase in rupture risk. One study even found levofloxacin carried the highest risk for actual rupture, while ciprofloxacin was more linked to tendonitis - inflammation that can lead to rupture if ignored.
Third-generation fluoroquinolones like moxifloxacin may be safer. The same 2022 Japanese study found no increased risk of Achilles rupture with these drugs. That’s a critical distinction. If you need a fluoroquinolone, ask: is there a lower-risk option?
How Fast Does This Happen?
It doesn’t take months. Symptoms can start within 48 hours. The median time from first dose to tendon pain? Just six days. Eighty-five percent of cases happen within the first month. And here’s the kicker - it can still happen months after you’ve stopped the drug.
One Reddit user, u/TendonWorrier, posted about starting levofloxacin for a UTI. By day two, his Achilles was throbbing. By day 10, it snapped. He didn’t realize the pain was a warning - he thought it was just muscle strain. He needed surgery. Recovery took over a year.
That’s not an outlier. The FDA’s own database, FAERS, shows thousands of tendon rupture cases tied to fluoroquinolones. Most of them happened fast. And many patients weren’t warned.
NSAIDs Don’t Increase the Risk - But They Hide It
Let’s clear up the biggest myth: NSAIDs like ibuprofen or naproxen don’t make fluoroquinolone-induced tendon rupture more likely. There’s no solid evidence that combining them raises the risk.
So why do people think they do? Because NSAIDs mask the pain. You take ibuprofen for your sore heel. The pain fades. You keep walking. You keep exercising. You ignore the warning. And then - snap.
NSAIDs aren’t the cause. They’re the distraction. They let you keep going until it’s too late. That’s why doctors warn against using them to treat fluoroquinolone-related tendon pain. You’re not fixing the problem - you’re hiding it.

Who’s Most at Risk?
Age is the biggest factor. If you’re over 60, your risk of tendon rupture from fluoroquinolones jumps 3.8 times. Kidney problems? That’s another red flag. Your body can’t clear the drug as fast, so levels build up.
Organ transplant patients? High risk. Steroid users? Even higher. But here’s what most people don’t know: even healthy, active people under 50 can get hit. Athletes, runners, gym-goers - they’re not immune. In fact, they’re more likely to notice the pain early because they’re tuned into their bodies. That’s why they’re often the ones reporting these cases.
And it’s not just the Achilles. About 10% of cases involve other tendons - the rotator cuff, the patellar, the wrist. But 90%? It’s the Achilles. That’s the one that gives out without warning.
What Happens Inside the Tendon?
Fluoroquinolones don’t just irritate tendons. They attack them at the molecular level.
They trigger the release of enzymes called matrix metalloproteinases (MMPs), which chew up collagen - the main structural protein in tendons. They also kill tendon cells (tenocytes) through oxidative stress. And they interfere with DNA replication, which stops the tendon from repairing itself.
The result? A tendon that’s weak, brittle, and unable to heal. It’s not inflammation. It’s structural breakdown. That’s why rest and ice don’t fix it. And why steroids - which reduce inflammation - don’t help either. In fact, steroids make it worse. That’s why the FDA specifically warns against using them with fluoroquinolones.
What Should You Do If You’re Prescribed One?
First: Ask if you really need it. Fluoroquinolones are powerful, but they’re not always the best choice. For simple UTIs, amoxicillin or nitrofurantoin are safer. For sinus infections, amoxicillin-clavulanate often works just as well.
If your doctor says you need a fluoroquinolone, ask: Which one? Is levofloxacin necessary? Or could ciprofloxacin or moxifloxacin work instead?
Then: Know the signs. Sharp pain, swelling, or stiffness in a tendon - especially the Achilles - within days of starting the drug? Stop taking it. Call your doctor. Don’t wait. Don’t tough it out. Don’t take NSAIDs to hide it.
Immobilize the area. Get an ultrasound or MRI if needed. Early action can prevent a full rupture. Once it tears, surgery is often required. Recovery takes six months to a year. And you might never get your full strength back.

Why Are These Warnings Still Ignored?
The FDA put a black-box warning on fluoroquinolones in 2008. That’s the strongest warning they can give. Yet in 2021, only 32% of patients said they were told about tendon rupture risk when prescribed these drugs.
Doctors are busy. Patients assume antibiotics are safe. Pharmacies don’t always print clear warnings on labels. And the media? They focus on rare side effects like hallucinations or heart rhythm issues - not the slow, silent destruction of tendons.
Meanwhile, prescriptions have dropped 21% since 2016, thanks to better awareness. But the number of reported tendon injuries is still rising. Why? Because when people do take them, they’re often older, sicker, and more vulnerable. The risk hasn’t gone away. It’s just concentrated in the people least likely to be warned.
What’s Next?
Researchers are now looking for biomarkers - early signs in the blood or tissue that predict who’s at risk. A 2023 study found elevated levels of MMP-2 and MMP-9 in patients who later developed tendon damage. That could lead to a simple blood test before prescribing.
Meanwhile, new antibiotics are being developed. Two next-generation quinolones, JNJ-Q2 and delafloxacin derivatives, are in trials with early signs of reduced tendon toxicity. They might offer the same power without the risk.
But until then? The message is simple: fluoroquinolones are not harmless. They’re powerful tools - but tools that can break your body if used carelessly. Don’t let a quick fix cost you your mobility.
Do NSAIDs increase the risk of tendon rupture when taken with fluoroquinolones?
No, there is no strong evidence that NSAIDs like ibuprofen or naproxen increase the risk of tendon rupture when taken with fluoroquinolones. However, NSAIDs can mask early symptoms of tendon pain, making it harder to notice warning signs. This delay can lead to a full rupture before the problem is addressed. The real danger is ignoring the pain - not the NSAID itself.
Which fluoroquinolone has the highest risk of tendon rupture?
Levofloxacin carries the highest documented risk for tendon rupture, with studies showing a 120% increased risk for Achilles tendon rupture compared to non-users. Ciprofloxacin is more often linked to tendonitis (inflammation), while moxifloxacin and other third-generation fluoroquinolones show little to no increased risk in recent studies. Always ask your doctor which specific drug they’re prescribing and why.
How soon after starting a fluoroquinolone can tendon pain begin?
Tendon pain can start as early as 48 hours after the first dose. The median time to onset is just six days. Most cases occur within the first month of treatment, but symptoms can also appear weeks or even months after stopping the medication. Never assume it’s safe just because you’ve been on the drug for a while.
Can tendon damage from fluoroquinolones be reversed?
Early-stage tendonitis (inflammation) may improve with rest, physical therapy, and stopping the antibiotic. But once a tendon ruptures, it usually requires surgery and months of rehabilitation. Even after recovery, many patients report lasting weakness, stiffness, or chronic pain. Prevention - stopping the drug at the first sign of pain - is the only reliable way to avoid permanent damage.
Are there safer alternatives to fluoroquinolones for common infections?
Yes. For uncomplicated urinary tract infections, nitrofurantoin, fosfomycin, or amoxicillin-clavulanate are often effective and safer. For sinus infections, amoxicillin or doxycycline are preferred first-line options. Fluoroquinolones should only be used when no other suitable antibiotic is available, especially in older adults or those with kidney issues.
Final Takeaway
Fluoroquinolones aren’t evil. They save lives - especially in serious infections like anthrax or complicated pneumonia. But they’re not for every bug. And they’re not safe for every person.
If you’re prescribed one, ask questions. Know which one. Know your risk. Know the signs. And if your tendon starts hurting - stop the drug. Don’t wait. Don’t take painkillers to push through it. Your tendon doesn’t heal itself if you keep using it.
One missed warning can cost you months of recovery. Or worse. Don’t let convenience override caution. Your body will thank you later.

Marc Bains
31 January 2026 - 15:37 PM
Man, I wish I'd known this before I took levofloxacin for that UTI last year. My Achilles felt weird on day three, but I figured it was just from hiking. By day 8, I couldn't walk. Surgery. Six months of PT. Now I'm careful with antibiotics. If your doc pushes a FQ, ask for the alternatives first. Your tendons will thank you.
Natasha Plebani
1 February 2026 - 17:27 PM
The molecular mechanism here is fascinating-fluoroquinolones induce mitochondrial dysfunction via topoisomerase II inhibition in tenocytes, triggering caspase-mediated apoptosis and upregulating MMP-2/9, which degrade collagen fibrils. The oxidative stress cascade essentially disables endogenous repair mechanisms. NSAIDs don't exacerbate this-they merely provide nociceptive masking, creating a dangerous feedback loop where tissue degradation proceeds unchecked. This isn't pharmacokinetics-it's pharmacodynamic sabotage of connective tissue homeostasis.
Kelly Weinhold
2 February 2026 - 03:01 AM
I just want to say-you're not alone if this happened to you. I had the same thing with levofloxacin. Thought it was just soreness, kept running. Ended up in a boot for three months. But here's the good part: I learned to listen to my body. Now I do yoga, stretch daily, and always ask my doctor about alternatives. It's scary, yeah, but knowledge is power. You can still be strong, active, healthy-just smarter about how you get there. You got this 💪
Rob Webber
2 February 2026 - 15:38 PM
Doctors are still prescribing these like candy. The FDA warning has been out since 2008 and yet I got this script last month for a sinus infection. No one mentioned tendon rupture. No one. This is medical malpractice. They don't care because they're not the ones lying in recovery for a year. If you're a doctor reading this-stop. Just stop. There are safer options. Your laziness is destroying people's lives.
calanha nevin
3 February 2026 - 17:05 PM
Levofloxacin carries the highest documented risk for tendon rupture among fluoroquinolones based on multiple large cohort studies including the 2022 BMJ Open analysis. Ciprofloxacin is associated more with tendonitis than rupture. Moxifloxacin shows no significant increase in rupture risk in recent data. NSAIDs do not increase rupture risk but mask early symptoms. Patients over 60 and those with renal impairment are at highest risk. Early discontinuation at first sign of pain prevents rupture. Always request alternative antibiotics when appropriate.
Lisa McCluskey
4 February 2026 - 07:06 AM
I've seen this in physical therapy. Patients come in with sudden Achilles pain after antibiotics. They're confused because they didn't do anything wrong. We tell them to stop the drug immediately. No NSAIDs. No stretching. Just rest. Sometimes it's tendonitis and it heals. Sometimes it's too late. The worst part? Most didn't know the risk. It shouldn't be this hard to find out. Just tell people.
owori patrick
5 February 2026 - 06:01 AM
This is so important. In Nigeria we don't always have access to alternatives but we need to be more aware. I shared this with my cousin who just got prescribed cipro. He didn't know about the risk. Now he's asking his doctor for something else. Education saves tendons. Thank you for writing this.
Adarsh Uttral
6 February 2026 - 02:45 AM
bro i took cipro for a bad ear infection last year and my knee started hurting like wtf. i thought i just sat wrong. turned out it was tendonitis. i stopped the med and it got better. never took another fq again. also why do docs even give these out for ear infections???
Yanaton Whittaker
7 February 2026 - 12:50 PM
So you're telling me the government knew about this for 16 years and still let Big Pharma push these drugs? This is why America is dying. We're being poisoned by corporate greed and lazy doctors. Stop the FQs. Ban them. This isn't a debate. It's a national health crisis.
Beth Cooper
9 February 2026 - 06:49 AM
Actually, the real danger is that this whole thing is a distraction. The FDA’s black box warning? A PR move. The real cause of tendon rupture is glyphosate exposure from GMO foods. Fluoroquinolones are just the scapegoat. You think they’d let you know the truth? They want you dependent on drugs. Read the studies-MMP-9 spikes in people who eat Roundup-laced corn. It’s all connected. Your tendon is just the messenger.
Donna Fleetwood
9 February 2026 - 08:40 AM
Thank you for sharing this. I’m a nurse and I’ve seen too many patients come in with ruptured tendons after FQs. I always ask if they’ve been on antibiotics lately. So many don’t connect the dots. Please, if you’re reading this and you’re prescribed one-ask your doctor why. Ask for the name. Ask for alternatives. And if your tendon hurts? Stop. Don’t wait. You’re not being dramatic-you’re being smart. Your body is trying to tell you something. Listen.