Scabies Treatment Effectiveness Checker
Treatment Assessment
Enter details about your scabies treatment to evaluate potential resistance risk and effectiveness.
Treatment Assessment Results
Scabies outbreaks are on the rise, and a growing worry among clinicians is whether the tiny mite Sarcoptes scabiei can develop resistance to the drugs we rely on. This article unpacks the science behind resistance, reviews the evidence that resistance is already showing up, and offers practical steps for doctors, veterinarians, and anyone dealing with an infestation.
Why resistance matters
When a treatment loses its punch, patients suffer longer, transmission spikes, and healthcare costs climb. The classic example comes from malaria: once‑effective antimalarials fell short because the parasite mutated. A similar pattern could happen with scabies if Sarcoptes scabiei starts outsmarting our best‑selling acaricides.
How resistance develops in mites
Resistance isn’t magic; it follows a few well‑documented biological routes:
- Genetic mutations that alter the drug’s target site, making it harder for the chemical to bind.
- Increased expression of detoxifying enzymes that break the drug down before it reaches the mite’s nervous system.
- Behavioral changes, such as deeper burrowing, that shield the mite from topical agents.
These mechanisms have been observed in other arthropods, like head lice and ticks, and laboratory studies confirm that Sarcoptes scabiei can acquire similar mutations after repeated exposure to sub‑lethal doses of acaricides.
What the data say: early signs of resistance
In 2022, a study from the University of Sydney reported treatment failures in a cohort of 68 patients who received standard 5% permethrin cream. DNA sequencing of surviving mites revealed a point mutation in the voltage‑gated sodium channel gene- the same mutation that underpins permethrin resistance in house‑dust mites.
Similarly, a 2024 field survey in Norway documented a 12% rise in cases that required a second course of oral ivermectin after the first dose failed to clear the rash. The researchers linked the outcome to repeated community‑wide ivermectin mass‑drug administrations for scabies control.
Both findings align with warnings issued by the World Health Organization (WHO) that antimicrobial resistance is a looming threat for ectoparasitic diseases and the Centers for Disease Control and Prevention (CDC) which now recommends surveillance for treatment failure in high‑risk settings.

Key treatments and how they work
Current first‑line options fall into two categories:
| Drug | Formulation | Mode of Action | Typical Efficacy | Resistance Risk |
|---|---|---|---|---|
| Permethrin | 5% cream | Blocks sodium channels, paralyzing the mite | 96‑99% cure rate | Emerging (point mutations observed) |
| Ivermectin | Oral 200µg/kg | Opens glutamate‑gated chloride channels | 92‑95% cure rate | Low but increasing after repeated mass dosing |
| Benzyl benzoate | 25% lotion | Disrupts mite cuticle | 80‑85% cure rate | Limited data, but tolerance reported |
All three drugs belong to the broader class of acaricides chemicals that target arthropods. Because they act on nervous system pathways, mutations that change channel structure can blunt their impact.
Detecting resistance early
Clinicians can’t wait for a full‑blown outbreak to spot a problem. Here are three practical tools:
- Clinical failure monitoring: If a patient still shows active burrows two weeks after a full course of permethrin or ivermectin, flag it as a possible resistance case.
- Skin‑scrape microscopy: Collect a few skin flakes and look for live mites after treatment. Persistence suggests the drug didn’t work.
- Genetic testing: PCR assays targeting the sodium‑channel gene (for permethrin) or the glutamate‑gated chloride receptor (for ivermectin) can confirm known resistance mutations. Labs in Australia, Europe, and the US now offer this service.
These steps align with recommendations from the American Academy of Dermatology (AAD), which encourages reporting of treatment failures to local public‑health departments.
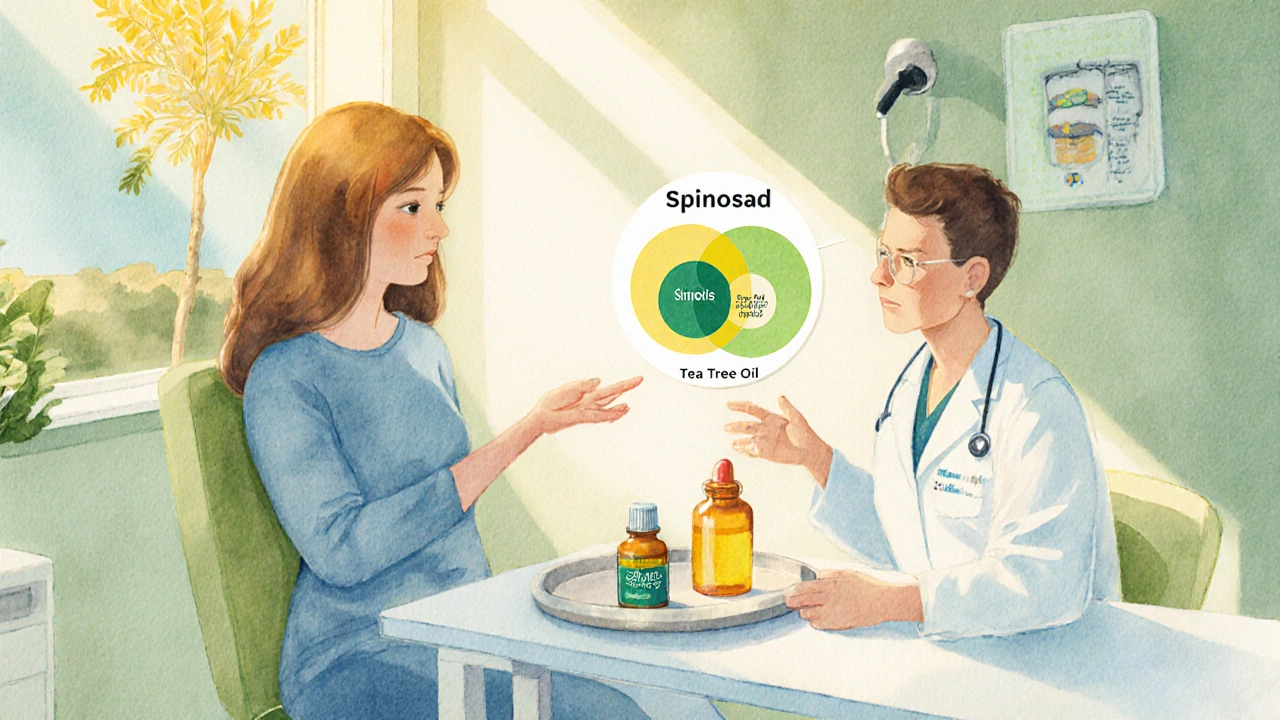
Alternative and next‑generation options
If resistance becomes widespread, we’ll need a broader toolbox:
- Spinosad: A newer insecticide that targets nicotinic acetylcholine receptors. Early trials in Norway show 94% cure rates without cross‑resistance to permethrin.
- Tea tree oil (Melaleuca alternifolia): Some small‑scale studies report mite mortality at 5% concentration, though standardization remains an issue.
- Combination therapy: Using permethrin followed by a single oral dose of ivermectin can overcome low‑level resistance, similar to strategies used in malaria.
Research funded by the National Institutes of Health (NIH) is exploring monoclonal antibodies that could neutralize mite saliva proteins, a completely different attack vector.
Practical steps for clinicians and caregivers
Whether you’re a family doctor, a dermatologist, or a pet owner dealing with a scabies‑like infestation in animals, here’s a quick checklist:
| Action | When to Apply | Key Considerations |
|---|---|---|
| Confirm diagnosis with dermoscopy or skin scrape | Before starting any therapy | Rule out bacterial infection or eczema |
| Use standard 5% permethrin or oral ivermectin | First‑line treatment | Follow dosage guidelines precisely |
| Check for clinical cure at day 14 | Two weeks post‑treatment | Persistent burrows = possible resistance |
| Order genetic resistance test | If failure is suspected | Send skin‑scrape to certified lab |
| Consider alternative or combination therapy | Confirmed resistance | Document response for surveillance |
Documenting each step helps public‑health agencies map resistance hotspots and adjust guidelines accordingly.
Looking ahead: research and policy priorities
Three areas need urgent attention if we want to stay ahead of a resistant scabies mite:
- Standardized surveillance: Nations should adopt a unified case‑reporting system, much like the influenza monitoring network.
- Incentivizing new drug development: The market for scabies treatments is small, so public‑private partnerships (e.g., the Drugs for Neglected Diseases initiative) could drive innovation.
- Education campaigns: Misuse of over‑the‑counter creams- applying half‑dose or re‑using old containers- creates the perfect breeding ground for resistance. Clear guidance for patients is essential.
Until these measures take hold, the best defense remains vigilant prescribing, proper dosing, and early detection of treatment failures.
Frequently Asked Questions
Can scabies come back after a successful treatment?
Yes. Reinfection can happen if close contacts aren’t treated simultaneously or if the environment (bedding, clothing) isn’t cleaned. This is not a sign of resistance; it’s a failure to break the transmission cycle.
How common is permethrin resistance right now?
Data are still limited, but recent surveys in Australia, Europe, and parts of Asia report resistance rates between 5% and 15% in high‑use communities. The trend is upward, prompting calls for routine monitoring.
Is oral ivermectin safe for children?
The FDA has approved ivermectin for children weighing at least 15kg. Below that weight, the safety profile is less well‑studied, so topical permethrin remains the preferred first‑line therapy for younger kids.
What should I do if my pet shows scabies‑like symptoms?
Seek a veterinarian. Animal scabies (sarcoptic mange) is caused by the same mite but often requires different dosing and sometimes a different drug class, such as selamectin or moxidectin.
Can resistance be reversed?
If a drug is withdrawn for a few generations, the selective pressure eases, and susceptible mite strains can re‑emerge. However, this process can take years and is not guaranteed.
Sarcoptes scabiei resistance is not inevitable, but ignoring early warning signs could let it spread. By combining proper dosing, vigilant monitoring, and a willingness to adopt new therapies, clinicians and patients can keep the scabies mite in check for years to come.





Shelley Beneteau
5 October 2025 - 14:26 PM
I wonder how often clinicians actually send skin‑scrape samples for resistance testing.
Sonya Postnikova
7 October 2025 - 03:20 AM
Great rundown! The checklist at the end really helps keep things straight, especially for busy practices :)
Anna Zawierucha
9 October 2025 - 10:53 AM
Oh fantastic, another reminder that tiny mites can outwit us like they’re starring in a sci‑fi thriller. Nothing like a bit of resistance drama to spice up a routine skin exam.
Mary Akerstrom
11 October 2025 - 18:26 PM
Thanks for pulling together the data it makes it easier for us to explain to patients why we need proper dosing and cleaning.
Delilah Allen
14 October 2025 - 02:00 AM
Resistance isn’t just a buzzword it’s a living, breathing threat that forces us to confront our own complacency. If we keep treating mites like they’re simple pests we’ll watch the problem grow larger and more uglier than a kindergarten drawing of a monster.
Nancy Lee Bush
16 October 2025 - 09:33 AM
Exactly! The more we ignore the early signals the faster we’ll need a whole new arsenal – and that’s a nightmare for patients and providers alike 😊.
Dan Worona
18 October 2025 - 17:06 PM
What they don’t tell you is that the pharmaceutical giants have a vested interest in downplaying mite resistance so they can keep selling the same old creams forever. They’re probably sitting on a vault of unpublished data that shows the real failure rates skyrocketing, but who cares when the profit margins stay fat?
Chuck Bradshaw
21 October 2025 - 00:40 AM
Let’s dissect the facts step by step. First, the pharmacodynamics of permethrin involve blocking voltage‑gated sodium channels, a mechanism that is well documented in arthropod neurobiology. Second, mutations in the para gene have been identified in multiple mite populations, directly reducing binding affinity for pyrethroids. Third, epidemiological surveys from Australia and Europe have reported treatment failure rates climbing from under 5% to upwards of 15% in high‑use communities. Fourth, the WHO has officially recognized acaricide resistance as a growing concern, which lends weight to the laboratory findings. Fifth, the clinical data presented in the 2022 Sydney study showed a statistically significant association between repeated permethrin exposure and the presence of the L925I point mutation. Sixth, oral ivermectin, while effective in many cases, also faces the specter of resistance through up‑regulation of glutamate‑gated chloride channel subunits, as hinted by the 2024 Norway field survey. Seventh, combination therapy, such as permethrin followed by a single dose of ivermectin, has demonstrated synergistic effects, potentially overcoming low‑level resistance, similar to combination regimens in malaria treatment. Eighth, newer agents like spinosad target nicotinic acetylcholine receptors, offering a mechanistic pathway that is largely orthogonal to existing drugs. Ninth, the development pipeline remains thin because of limited market incentives, a point underscored by the lack of new FDA‑approved scabies medications in the past decade. Tenth, public‑health surveillance systems for scabies are still fragmented, making it harder to capture real‑time resistance trends. Eleventh, proper application techniques, including thorough coverage of the entire body and a full 8‑hour contact time, are crucial; sub‑optimal use can masquerade as resistance. Twelfth, environmental decontamination-washing bedding and clothing at >60 °C-remains a non‑pharmacological pillar that can prevent reinfestation and reduce selective pressure. Thirteenth, genetic testing via PCR for known resistance markers is becoming more accessible and should be integrated into failure protocols. Fourteenth, patient education about avoiding over‑the‑counter half‑doses can mitigate the evolution of resistant strains. Finally, continued investment in research, perhaps through public‑private partnerships, is essential to stay ahead of this adaptable parasite.
Howard Mcintosh
23 October 2025 - 08:13 AM
Yo, that spinosad thing sounds cool but does it actually work on the nursin' kids? I heard some docs say it’s a game changer, but my aunt swears she’s stuck on the old cream.
Jeremy Laporte
25 October 2025 - 15:46 PM
All in all, keeping an eye on treatment outcomes and being ready to pivot when resistance shows up will protect patients and keep the mite population in check.