After a heart attack, bypass surgery, or other major cardiac event, the last thing you want to do is sit still. But jumping back into your old routine? That’s just as dangerous. The truth is, exercise isn’t just okay after a heart event-it’s one of the most powerful tools you have to live longer, feel better, and avoid another crisis. Yet most people either do too little or too much. And that’s where cardiac rehabilitation comes in.
Why Exercise After a Heart Event Isn’t Optional
It’s not hype. Studies show people who stick to a supervised cardiac rehab program cut their risk of dying within five years by 30%. That’s not a small number. It means three out of ten people who complete rehab won’t die from another heart problem. Compare that to people who try to exercise on their own-those with no guidance have nearly double the chance of being readmitted to the hospital within a year.
Why does this work? Because your heart isn’t just a muscle-it’s a system. After damage, it needs help rebuilding strength, improving blood flow, and learning to handle stress again. Exercise trains your heart to pump more efficiently. It lowers blood pressure, reduces bad cholesterol, and helps control blood sugar. But most importantly, it rebuilds your confidence. Many people live in fear after a heart event-afraid that walking too fast or climbing stairs will trigger another attack. Rehab teaches them it’s safe.
The Three Phases of Safe Recovery
Cardiac rehab doesn’t happen all at once. It’s broken into three clear stages, each with specific goals and limits. Skipping ahead? That’s how people end up back in the ER.
Phase 1: Hospital and Early Recovery (Days 1-5)
This starts while you’re still in the hospital. No running. No lifting. Just movement. Simple things like sitting up, swinging your legs over the side of the bed, and taking a few steps with help. Ankle pumps-flexing your feet up and down-are common. Why? They keep blood moving and prevent clots. Activity is measured in METs-metabolic equivalents. In this phase, you’re working at just 1-2 METs. That’s like slowly walking around your room.
Doctors now recommend getting up and moving within 24 hours after procedures like stent placement. Studies show patients who do this recover function 15-19% faster than those who wait two days. But it’s not about how far you go-it’s about how safely you start.
Phase 2: Outpatient Rehab (Weeks 2-12)
This is where most people begin their real journey. You’ll attend sessions three times a week, usually for 6-12 weeks. Each session includes warm-up, aerobic exercise, strength training, and cool-down-all under supervision.
Aerobic work? Start with walking. Five to ten minutes on day one. Add two minutes every few days. By week six, you’re aiming for 30 minutes. The goal isn’t speed-it’s consistency. You should be able to talk while walking. If you can’t, you’re going too hard. That’s the talk test. Simple. Effective.
Heart rate targets? Usually your resting heart rate plus 20-30 beats per minute. If you’re on beta-blockers, your max heart rate might be 20-30% lower than normal. That’s normal. Don’t chase old numbers. Use the Borg scale for exertion-aim for 11 to 14 out of 20. That’s light to moderate effort.
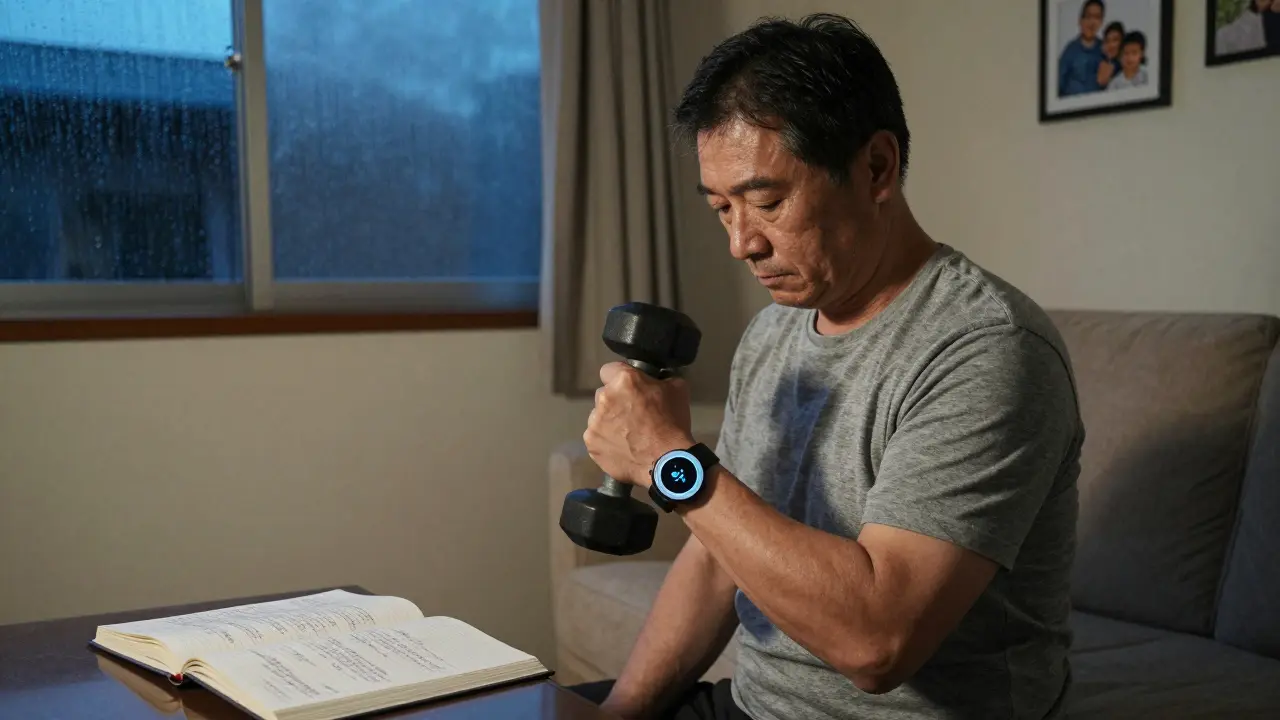
Strength training starts with light resistance: 1-3 pound weights, seated rows, leg lifts. Two days a week. No heavy lifting. No holding your breath. Breathing is key. Exhale when you push, inhale when you release.
Phase 3: Long-Term Maintenance (After 12 Weeks)
Now you’re on your own-but not alone. The American Heart Association recommends 150 minutes of moderate aerobic activity per week. That’s 30 minutes, five days a week. Or 75 minutes of vigorous activity, like brisk cycling or stair climbing. Plus, two days of strength training.
Here’s the catch: you still need to monitor yourself. Keep using the talk test. Track your heart rate with a simple wrist monitor. And pay attention to warning signs. If you feel chest pressure, dizziness, nausea, or sudden weakness-stop. Don’t push through it.
Supervised Rehab vs. Going It Alone
Can you just follow a generic fitness plan after a heart event? Technically, maybe. But statistically? No.
People in formal rehab programs recover 25% faster and are 30% less likely to die within five years than those who exercise on their own. Why? Three big reasons:
- Personalization: Your rehab plan is built around your specific condition-not a one-size-fits-all routine. Someone with heart failure needs different work than someone who had a stent placed.
- Monitoring: Your heart rate, blood pressure, and rhythm are tracked in real time. If something goes wrong, help is right there.
- Education: You learn how to recognize danger signs, manage medications during activity, and adjust for weather or fatigue.
Meanwhile, 27% of people who exercise without supervision push past safe heart rate limits in the first month. That’s not bravery-it’s risk. And 8% of them end up needing emergency care because of it.

What to Watch Out For
You don’t need to be scared-but you do need to be aware. There are seven warning signs that mean STOP immediately:
- Chest pain or pressure
- Pain spreading to your arm, neck, jaw, or back
- Dizziness or lightheadedness
- Irregular or racing heartbeat
- Unusual shortness of breath
- Slurred speech or confusion
- Sudden weakness or numbness in face, arm, or leg
These aren’t vague symptoms. They’re red flags. If you feel any of these during exercise, sit down, rest, and call your doctor. Don’t wait. Don’t assume it’s just fatigue.
Also, be smart about timing. If you take medication that affects your heart rate-like beta-blockers-your peak performance window might be 1-2 hours after taking it. Schedule workouts then. Avoid exercising right after meals, in extreme heat or cold, or when you’re sick.
How to Stay on Track
Sticking with it is harder than starting. Here’s what works:
- Use a journal: Write down how you felt before, during, and after each session. Note fatigue, breathing, or discomfort. Patterns emerge over time.
- Find a buddy: Someone to walk with makes it easier to show up.
- Use indoor options: If it’s freezing or rainy, walk in a mall, use a stationary bike, or follow a seated exercise video.
- Track progress, not perfection: Did you walk 10 minutes today? Great. Did you do it three days this week? Even better. Progress isn’t linear.
One study found that 92% of people who completed 36 rehab sessions were still exercising on their own a year later. Only 45% of those who tried on their own stuck with it. The difference? Support, structure, and knowing you’re not alone.
What’s New in Cardiac Rehab
The field is changing fast. Telehealth is now a big part of rehab. Programs like Cleveland Clinic’s “Cardiac Rehab Connect” mix 12 in-person visits with 24 virtual ones, using FDA-approved wearables to monitor heart rate and rhythm remotely. In 2023, 65% of accredited programs use this tech.
High-intensity interval training (HIIT) is also gaining ground. For stable patients, short bursts of higher effort-like 30 seconds of fast walking followed by 90 seconds of slow walking-can improve fitness 37% more than steady walking. But this is only safe under professional supervision. Don’t try HIIT at home without clearance.
And yes, insurance covers it. Medicare and most private plans pay for up to 36 sessions after a qualifying event. If your doctor didn’t mention rehab, ask. It’s not an add-on-it’s standard care.
Final Thought: This Isn’t About Getting Back to Normal
It’s about becoming stronger than before. Your heart has been through trauma. But it’s also incredibly resilient. With the right plan, you won’t just survive-you’ll thrive. You’ll walk farther, climb stairs without gasping, play with your grandkids without fear, and sleep better at night.
Cardiac rehab isn’t a punishment. It’s your second chance. And the best part? You don’t have to do it alone.
Can I start exercising the same day after a heart attack?
For low-risk patients, light movement like sitting up and taking a few steps is encouraged within 24 hours after procedures like stent placement. But intense exercise is not safe. Always follow your medical team’s guidance. Early mobility reduces recovery time, but only when done safely.
How do I know if I’m exercising too hard?
Use the talk test: if you can’t speak in full sentences without gasping, you’re pushing too hard. Also, watch for chest pain, dizziness, nausea, or an irregular heartbeat. Your heart rate should stay within your prescribed range-usually resting heart rate plus 20-30 bpm. If you’re on beta-blockers, your max may be lower. Always check with your rehab team.
Is it safe to lift weights after a heart event?
Yes-but only after clearance and with light resistance. Start with 1-3 pound weights, seated exercises, and controlled movements. Avoid holding your breath, lifting heavy weights overhead, or doing rapid repetitions. Strength training should be done no more than two days per week, and always after aerobic activity.
What if I can’t get to a rehab center?
Many programs now offer hybrid or fully virtual options using wearable heart monitors and video check-ins. Ask your doctor for a referral to a telehealth cardiac rehab program. Medicare and most insurers cover these. If none are available, work with your provider to get a personalized home plan with clear limits and warning signs to watch for.
Why is cardiac rehab so underused?
Only 20-30% of eligible patients enroll. Common reasons include lack of transportation, work conflicts, insurance confusion, and not being referred by a doctor. Rural areas have even lower participation. But it’s covered by Medicare and most private plans. If you’re eligible, ask your doctor to refer you-don’t wait.
Can I ever return to my old workout routine?
Maybe-but not right away, and not without adjustments. Your body has changed. What felt easy before might now be too intense. Most people return to activities like swimming, cycling, or walking, but often at a lower intensity. Never go back to high-intensity training without medical approval. Your new normal is healthier and safer than your old one.





Chris Clark
21 December 2025 - 08:17 AM
man i wish they told me this stuff when i had my stent. i thought i could just jump back into lifting like nothing. ended up in the er after trying to carry groceries. dumb move. now i walk every morning and use that talk test like they said. still can't believe how much better i feel. no more chest tightness when i climb stairs. thanks for laying it out so clear.
Nancy Kou
22 December 2025 - 07:58 AM
This is exactly what my dad needed to hear after his bypass. He refused rehab for months because he thought it was 'for old people.' Started a virtual program last month and now he walks 45 minutes every day. He says he feels like he got his life back. If you're on the fence, just do it. No excuses.
Janelle Moore
23 December 2025 - 10:19 AM
they're lying about rehab. the real reason they push it is so they can track your heart rate and sell your data to insurance companies. i read a guy on reddit who said his device sent his bpm to a server every 30 seconds. they use it to raise premiums. don't fall for it. just walk slow in your yard and ignore the machines.
Henry Marcus
24 December 2025 - 10:45 AM
Cardiac rehab? Ha! That’s just the pharmaceutical-industrial complex’s latest money-grab. They don’t care if you live-they care if you keep buying beta-blockers, statins, and fancy wearable monitors that cost more than your car. I did 30 minutes of brisk walking every morning for 6 months-no heart rate monitor, no fancy program-and my troponin levels dropped. No one told me that was possible. The system wants you dependent. Don’t be a sheep.
Frank Drewery
25 December 2025 - 16:49 PM
I was terrified to move after my heart attack. Thought I’d die if I walked too fast. But the rehab nurse said, 'Your heart isn't broken-it's just out of shape.' That changed everything. I started with 5 minutes a day. Now I hike on weekends. It’s not about being strong. It’s about being consistent. And yeah, it’s okay to have bad days. Just show up.
Ryan van Leent
26 December 2025 - 10:26 AM
why do people even need a program for this? just walk. everyone knows you don't lift heavy after a heart attack. this article is just padding. i did zero rehab and i'm fine. stop making people feel guilty for not joining some expensive class. real life isn't a clinical trial
Sajith Shams
27 December 2025 - 17:15 PM
You people are wasting time talking about walking. The real issue is the sodium in your diet. That's what kills you not lack of exercise. I had a heart attack at 42 and I stopped eating salt completely. No meds. No rehab. Just no salt. My BP dropped 30 points in two weeks. You're being manipulated by the American Heart Association. They get paid by food companies to push exercise. Look up the funding sources. It's all connected.
Adrienne Dagg
29 December 2025 - 11:22 AM
OMG this is so needed!! 🙏 I started rehab after my angioplasty and honestly? It saved my mental health too. I was so scared to even hold my toddler. Now I carry her up the stairs like a champ 😭💪 The talk test? Life-changing. And yes, the insurance thing is real-Medicare covered ALL 36 sessions. Just ask your doc!!
Chris Davidson
29 December 2025 - 15:59 PM
Exercise after cardiac event is beneficial. Supervised rehabilitation reduces mortality. This is established medical fact. The data is robust. The phases described are consistent with ACC/AHA guidelines. Those who disregard professional guidance increase risk. End of discussion.
Glen Arreglo
31 December 2025 - 11:19 AM
I’ve seen too many people push too hard after a heart event. I lost my brother to a cardiac arrest while he was trying to 'get back in shape.' He ignored the talk test. He thought he was being tough. He wasn’t. He was dying. This guide? It’s not just advice-it’s a lifeline. If you’re reading this and you’re scared? You’re supposed to be. That means you’re listening.
benchidelle rivera
1 January 2026 - 11:36 AM
I run a cardiac rehab group for women over 60. Most of them never thought they’d walk again after their stents. One woman, 78, started with 3 minutes of walking and now hikes with her church group. Progress isn’t about speed. It’s about showing up. And yes, you can do this. You’re not broken. You’re rebuilding. One step. One day. One breath at a time.
holly Sinclair
2 January 2026 - 14:43 PM
It’s fascinating how the body adapts. After a cardiac event, the heart doesn’t just heal-it reorganizes. The capillary density increases, mitochondrial efficiency improves, and even the autonomic nervous system recalibrates. But what’s rarely discussed is the psychological rewiring. The fear of movement becomes a conditioned response, and rehab isn’t just about physical capacity-it’s about unlearning terror. We treat the heart like a machine, but it’s a living system shaped by trauma, memory, and hope. The talk test? It’s not just a metric-it’s a conversation between your body and your mind. And when you finally hear it whisper, 'I’m safe,' that’s when true recovery begins.