When you prescribe a generic drug, you might think you’re doing the right thing-saving patients money, following guidelines, making care more accessible. But in 2026, that simple act carries more legal risk than ever before. A patient takes a generic medication you prescribed, suffers a severe reaction, and the manufacturer can’t be sued. So who’s left? Physician liability is no longer just about dosing errors or missed diagnoses. It’s now deeply tied to the rise of generic drugs and a legal system that has quietly shifted blame onto doctors.
Why Generic Drugs Changed Everything
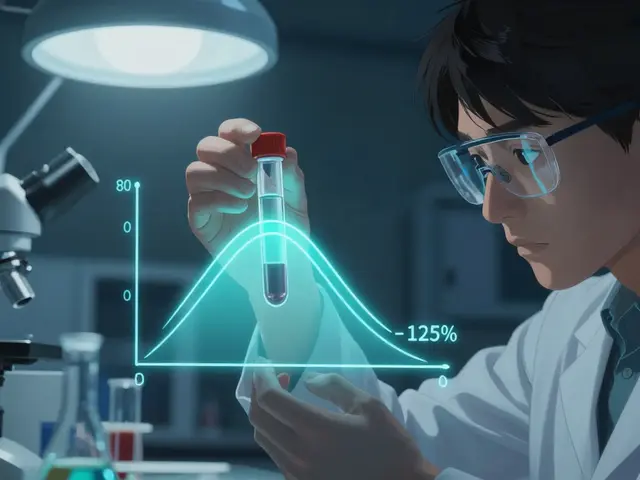
In 2011 and 2013, the U.S. Supreme Court made two decisions that rewrote the rules of drug liability. In PLIVA v. Mensing and Mutual Pharmaceutical v. Bartlett, the Court ruled that generic drug makers can’t be held responsible for failing to update warning labels. Why? Because federal law forces them to copy the brand-name label exactly-they can’t change it on their own. So if a generic drug causes harm, the manufacturer walks away. No lawsuits. No settlements. No accountability. That left patients with nowhere to turn. And over time, more and more of them started suing the doctors who prescribed those drugs. The numbers don’t lie. Between 2014 and 2019, physician-targeted lawsuits involving generic drugs jumped 37%. In 2022, a survey of 1,200 doctors found that 68% felt more anxious about prescribing generics. Nearly half admitted they sometimes choose the more expensive brand-name drug-not because it’s better, but because they’re scared of being sued.What Makes a Doctor Liable?
You’re not automatically liable just because you prescribed a generic. But if a patient is harmed, the legal system will look at three things:- Duty: Did you have a doctor-patient relationship? (Yes, if you prescribed it.)
- Dereliction: Did you fail to meet the standard of care?
- Direct cause: Did your decision directly lead to the harm?
State Laws Vary-And That’s a Problem
Forty-nine states allow pharmacists to substitute generics unless you write “dispense as written” on the prescription. But here’s where it gets messy:- In 32 states, pharmacists must notify you within 72 hours if they swap a drug.
- In 17 states, they don’t have to tell you at all.
Brand-Name Manufacturers Aren’t Your Shield
You might think, “If I prescribe a brand-name drug, and the patient gets a generic, the brand company should be liable.” That’s what one Alabama court thought in 2014. But the state legislature shut that down in 2015 with SB80, which explicitly says brand-name makers aren’t responsible for injuries caused by generics. In other words: Even if you pick the brand-name drug, you can’t count on the manufacturer to take the blame if the pharmacy substitutes it. The legal system doesn’t see it that way. The only person who’s consistently on the hook is the prescriber.What You’re Doing Now Might Be Putting You at Risk
Most doctors still treat generic prescribing like it’s 2005. They check the box, say “medication discussed,” and move on. But that’s not enough anymore. A 2023 report from Medical Risk Management found that doctors who document specific discussions about generic substitution risks reduce their liability exposure by 58%. That’s huge. What does “specific” mean? It means writing down:- The exact medication and its potential side effects
- Whether it’s a generic or brand
- Any warnings about driving, alcohol, or other activities
- Whether you instructed “dispense as written”
Insurance Costs Are Rising-And So Are Premiums
Your malpractice insurance isn’t ignoring this. The American Professional Agency reports a 7.3% premium surcharge for physicians who routinely authorize generic substitutions without proper counseling documentation. And it’s not just premiums. Between 2013 and 2022, average malpractice premiums for primary care physicians rose 22.7%. A lot of that is tied to the rise in generic-related claims. One doctor in Massachusetts told a forum: “I now add 15 to 20 minutes to every visit just to document substitution risks. It’s exhausting. But I’d rather spend the time than get sued.”What You Should Do Today
You can’t control what the pharmacist does. But you can control what you document and how you prescribe. Here’s your action plan:- Use ‘dispense as written’ for drugs with narrow therapeutic indices: levothyroxine, warfarin, phenytoin, lithium, cyclosporine, and certain anti-seizure meds.
- Document specific counseling in your EHR. Don’t just say “medication discussed.” Name the drug, the risk, the advice given.
- Know your state’s substitution rules. If your state doesn’t require pharmacist notification, assume you won’t be told. That means you need to be more cautious.
- Don’t assume generics are always interchangeable. For some patients, even tiny differences can trigger reactions. Trust your clinical judgment.
- Review your malpractice policy. Ask your insurer: “Does my coverage include claims related to generic drug prescribing?”
The Bigger Picture
Generic drugs are essential. They save billions. They make care affordable. No one’s arguing against them. But the legal system hasn’t caught up. The Supreme Court’s rulings created a gap-patients hurt by generics have no recourse against manufacturers. So they sue the doctor. And with 90% of all prescriptions filled as generics, this isn’t a niche issue. It’s the new normal. Legal scholars predict physician-targeted lawsuits involving generics will rise another 45% by 2027. If you’re not changing how you document and prescribe today, you’re playing Russian roulette with your license. This isn’t about fear. It’s about responsibility. The law has shifted. You have to shift with it.Can I be sued if a pharmacist substitutes a generic without my knowledge?
Yes. In most states, if you didn’t write ‘dispense as written,’ the pharmacist is legally allowed to substitute. But you’re still the prescriber. Courts hold you responsible for the outcome, not the pharmacist. That’s why documenting your intent and counseling is critical.
Are generic drugs less safe than brand-name drugs?
No. Generic drugs meet the same FDA standards for safety and effectiveness. But they can have different inactive ingredients or slight formulation differences. For drugs with narrow therapeutic windows-like levothyroxine or warfarin-those differences can matter. That’s why you need to know which ones require extra caution.
Should I stop prescribing generics altogether?
No. That’s not practical or ethical. Generics save patients money and improve access. Instead, be strategic. Use ‘dispense as written’ for high-risk drugs. Document counseling clearly. Know your state’s laws. Don’t avoid generics-manage the risk.
What if a patient insists on the brand-name drug?
That’s fine. But don’t just write the brand name. Document the patient’s request, your discussion about cost and alternatives, and your final decision. This protects you if they later claim you didn’t inform them about cheaper options.
Has anything changed since the 2023 Johnson v. Teva ruling?
Yes. The 9th Circuit ruled that if a brand-name manufacturer updates its warning label and the generic manufacturer doesn’t follow, the generic maker can be held liable for failing to update. This is a narrow exception, but it’s the first crack in the Mensing/Bartlett wall. It doesn’t change your liability-but it means you should still pay attention to FDA safety alerts.




Kristina Felixita
7 January 2026 - 21:17 PM
Okay but like… why are we still pretending generics are just as safe? I’ve had patients come in with wild rashes from generic levothyroxine-same active ingredient, sure, but the fillers? Totally different. And no one talks about that. I mean, c’mon. If your body’s sensitive to corn starch or lactose, and the generic uses it? You’re screwed. And then you get blamed for not ‘counseling’ enough? Like, I don’t have time to write a novel on every script. This system is broken.
Ken Porter
8 January 2026 - 02:39 AM
Doctors are getting sued because the pharma industry got a free pass. That’s it. Supreme Court made it legal to avoid accountability. Now the doc takes the fall. Fix the law. Don’t punish the people trying to keep costs down.
Dave Old-Wolf
8 January 2026 - 13:30 PM
I get the fear. But I also see patients who can’t afford brand-name meds and end up skipping doses. That’s way more dangerous than a generic swap. I always check the label, ask if they’ve had reactions before, and write ‘dispense as written’ for anything with a narrow window. It’s not that hard. Just don’t rush it.
Prakash Sharma
10 January 2026 - 09:57 AM
USA is falling apart. Pharma companies get rich, doctors get hunted, patients get confused. In India, we don’t have this mess. Pharmacies don’t substitute without permission. Doctors are respected. Why can’t America just fix its own system instead of blaming the ones on the front lines?
Donny Airlangga
10 January 2026 - 12:24 PM
My mom had a bad reaction to a generic antiseizure med. She didn’t even know it was switched. The pharmacist never called. The doctor never asked. Now she’s on disability. I don’t blame the doc-but I blame the system that lets this happen without warning.
Molly Silvernale
11 January 2026 - 09:16 AM
It’s not about generics… it’s about control. Who holds power when the medicine is no longer a product but a liability? The manufacturer? The pharmacist? The state? Or the poor soul holding the pen? We’ve turned healing into a legal minefield-and now we wonder why burnout is at 87%? The soul of medicine is being buried under paperwork, fear, and federal loopholes. We’re not just documenting prescriptions-we’re documenting survival.
Joanna Brancewicz
11 January 2026 - 15:35 PM
Therapeutic equivalence ≠ clinical equivalence. Especially for warfarin. INR fluctuations are real. Documenting ‘dispense as written’ + specific counseling reduces risk. EHR templates now enforce it. Use them. Or get sued.
swati Thounaojam
11 January 2026 - 17:49 PM
in india we dont have this problem. pharmacist ask before swap. doctor know. patient know. simple. why usa so complicated?