In a significant development in the ongoing battle against the novel coronavirus, a recent study has suggested that certain commonly used antihistamine medications might have the potential to prevent the virus responsible for COVID-19 from infecting cells. The study examined the effects of three particular antihistamines: hydroxyzine, diphenhydramine, and azelastine, in laboratory conditions and found promising results that could open new avenues in COVID-19 treatment modalities.
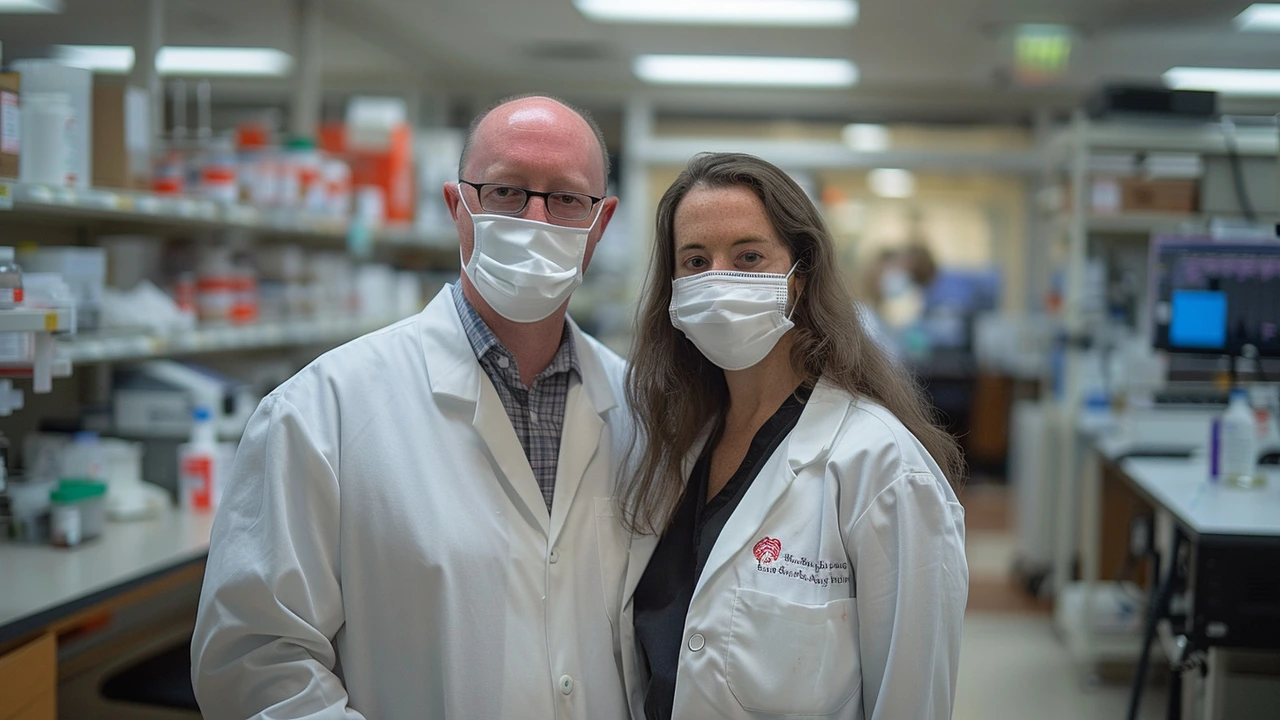
Leah Reznikov, Ph.D., an Assistant Professor of Physiological Sciences at the University of Florida (UF) College of Veterinary Medicine, alongside David A. Ostrov, Ph.D., Associate Professor of Immunology and Pathology at the UF College of Medicine's Department of Pathology, Immunology, and Laboratory Medicine, spearheaded this groundbreaking research. Their collaborative efforts were primarily focused on identifying currently authorized medications that could potentially interfere with the infectious mechanism of the SARS-CoV-2 virus, the pathogen behind COVID-19.
The researchers embarked on this journey by leveraging healthcare databases to investigate if individuals taking specific antihistamines exhibited lower infection rates. Their analysis included medical records of around 240,000 Californians, which revealed that people aged 61 and over who were on specific antihistamines seemed to have reduced chances of contracting COVID-19 compared to those who weren't. These findings laid the groundwork for subsequent experiments that combined human and primate cells to assess the antiviral efficiency of these drugs against the virus.
In the laboratory, the team tested the antivirus capacity of the medications and found that hydroxyzine, diphenhydramine, and azelastine effectively inhibited the virus's ability to infect cells. Notably, hydroxyzine and azelastine require prescriptions for use, whereas diphenhydramine can be easily procured over-the-counter and is widely known by its brand name, Benadryl, often used to treat cold and allergy symptoms. The potency of these drugs against SARS-CoV-2 in the cell tests is a promising step forward; however, it is imperative to conduct clinical trials to confirm their effectiveness and safety in preventing, treating, or serving as an adjunct therapy in severe COVID-19 scenarios.
The precise mechanisms through which these antihistamines exert their inhibitory effect on the SARS-CoV-2 virus are not yet fully understood. This emphasizes the need for further research to decipher exactly how these drugs interact with the virus and potentially disrupt its replication process. A key area of interest in this ongoing investigation is the role of sigma receptors. These proteins play crucial parts in cellular communication networks and might be involved in the process by which the virus replicates inside human cells. Understanding this interaction could unlock new therapeutic strategies against COVID-19.
While the study's results are indeed promising, they also come with a note of caution. The observed correlation between antihistamine usage and reduced infection rates does not establish a direct cause-and-effect relationship. As such, the research community urges the public to refrain from self-medicating with these drugs as a preventative or treatment measure for COVID-19 without proper clinical evidence supporting their efficacy in such contexts. Self-medication could potentially lead to adverse effects or interfere with existing medical conditions, underscoring the importance of conducting comprehensive clinical trials.
As the world continues to face the challenges posed by the COVID-19 pandemic, discoveries like these offer a glimmer of hope. The possibility that medications already available and widely used for other conditions could be repurposed to fight this devastating virus is an exciting prospect. It highlights the importance of innovative scientific inquiry and the potential to find solutions in unexpected places. The journey from laboratory findings to clinical application is complex and requires rigorous testing and validation, but the path is now set for further exploration. Researchers are eager to continue their work, delving deeper into how these antihistamines could contribute to the global effort to manage and eventually overcome COVID-19.




Nathan Hamer
5 October 2025 - 16:57 PM
Wow, what a dazzling revelation! 🌟 The notion that everyday antihistamines could slam the doors shut on SARS‑CoV‑2 feels like a plot twist worthy of a blockbuster 🎬; the science is humming with promise, and the possibilities are practically bursting at the seams!!! Imagine, a simple over‑the‑counter pill stepping onto the battlefield of a pandemic, wielding its modest chemistry like a seasoned warrior 🛡️; the sheer elegance of repurposing what we already trust is nothing short of poetic. Yet, let us not be blinded by the sparkle-this is still a laboratory whisper, a delicate echo that must be amplified through rigorous trials, lest we rush headlong into uncharted waters. The researchers have opened a door, but the hallway beyond is lined with cautionary signs, reminding us that correlation does not equal causation! 🧐 The data from 240,000 Californians hints at a protective veil for those over 60, but we must ask: are there hidden confounders lurking in the shadows? Could concurrent medications, lifestyle factors, or even genetic quirks be the true guardians? The cell‑culture triumphs with hydroxyzine, diphenhydramine, and azelastine are thrilling, yet the human body is a far more intricate stage where many actors compete. Let us champion the optimism while anchoring it in prudence, urging the scientific community to sprint toward well‑designed clinical trials. In the meantime, let’s keep the conversation alive, spread the word responsibly, and celebrate this glimpse of hope without succumbing to premature self‑medication 🚫💊. The future may yet reward this curiosity with a new tool in our antiviral arsenal, but for now, we watch, we wait, and we hope with measured enthusiasm!!!
Tom Smith
6 October 2025 - 15:10 PM
Well, look at that-another "breakthrough" that sounds great on paper but will need a lot of real‑world testing. The sarcasm is real, but the data is still early, so keep your expectations in check.
Kyah Chan
7 October 2025 - 13:23 PM
The authors have presented an intriguing hypothesis, yet the rigor of their epidemiological analysis leaves much to be desired. One must consider potential selection bias inherent in such database studies. Moreover, the in‑vitro efficacy does not automatically translate to clinical relevance. It would be prudent to await peer‑reviewed randomized trials before drawing definitive conclusions.
Ira Andani Agustianingrum
8 October 2025 - 11:37 AM
Great to see some optimism, but let’s stay grounded. The lab results are promising, yet we need solid human data. Until then, keep using antihistamines as directed for allergies.
James Higdon
9 October 2025 - 09:50 AM
While we admire innovative thinking, we must not abandon safety for novelty. Any off‑label use without clinical backing risks harm. Ethical responsibility demands thorough trials before recommending these drugs for COVID‑19.
Wanda Smith
10 October 2025 - 08:03 AM
It’s fascinating how quickly the narrative shifts from "safe and common" to a potential hidden agenda. Are we sure these studies aren’t being steered by pharmaceutical interests? Remember, every new treatment may come with unseen strings attached.
Bridget Jonesberg
11 October 2025 - 06:17 AM
The prospect of repurposing antihistamines is certainly compelling, yet the discourse surrounding it must remain measured. While the cellular assays demonstrate inhibition, the pharmacokinetic parameters in humans could differ substantially. Moreover, the interaction with sigma receptors, though hypothesized, lacks definitive mechanistic elucidation. It would be remiss to overlook the necessity for dose‑response studies that align therapeutic windows with safety margins. One should also contemplate the broader implications for patients already dependent on these medications for chronic conditions.
Marvin Powers
12 October 2025 - 04:30 AM
Isn't it just wonderful when a simple allergy pill might moonlight as a viral blocker? Of course, the reality is a bit messier-clinical validation is the name of the game. Still, kudos to the team for thinking outside the box and giving us something to talk about over coffee. 🙂
Randy Pierson
13 October 2025 - 02:43 AM
Colorful news! The notion that antihistamines could double‑duty as antiviral agents paints a vibrant picture of medical ingenuity. Yet, the canvas remains largely unfilled until robust trials color in the details. Let’s stay hopeful but keep a critical eye on the evolving palette.
Bruce T
14 October 2025 - 00:57 AM
Look, I'm all for new ideas, but self‑medicating based on a lab test is just reckless. Wait for proper studies before you pop pills for COVID.
Darla Sudheer
14 October 2025 - 23:10 PM
This is interesting. Let's see the results when they actually test it on people.
Elizabeth González
15 October 2025 - 21:23 PM
The philosophical implications of drug repurposing are profound, yet the empirical evidence must guide our conclusions. We should await the outcomes of rigorously designed trials before integrating these antihistamines into therapeutic protocols.
chioma uche
16 October 2025 - 19:37 PM
Our nation deserves the best, not foreign experiments. This is a chance to prove our own scientific might.
Satyabhan Singh
17 October 2025 - 17:50 PM
It is intellectually stimulating to contemplate the intersection of receptor pharmacology and viral replication. Nonetheless, the sanctity of methodological rigor must be upheld. I look forward to seeing peer‑reviewed data that substantiate these preliminary observations.
Keith Laser
18 October 2025 - 16:03 PM
Well, if an antihistamine can give us a fighting chance, why not give it a whirl? Still, we shouldn’t abandon the hard‑won vaccines and proven treatments. Let’s keep a balanced view and push for fast‑track trials.
Winnie Chan
19 October 2025 - 14:17 PM
Sounds promising, but don’t start hoarding Benadryl yet.
Kyle Rensmeyer
20 October 2025 - 12:30 PM
They don’t tell you the hidden side effects :) the pharma push is real
Rod Maine
21 October 2025 - 10:43 AM
this is like a level up for the meds, but idk if it works in real life lol
Othilie Kaestner
22 October 2025 - 08:57 AM
National pride should trump all critiques.