Ever wondered whether a drug that’s meant to stop seizures could actually make you feel down? That’s the dilemma many patients face when they’re prescribed valproic acid. In this article we break down what the science says, who’s most at risk, and what you can do if mood changes start to creep in.
What Is Valproic Acid?
Valproic Acid is an anticonvulsant and mood‑stabilizing medication that’s been on the market since the 1960s. It’s approved for treating epilepsy, generalized seizures, and bipolar disorder. Chemically it’s a short‑chain fatty acid that crosses the blood‑brain barrier easily, allowing it to act on neurons throughout the central nervous system.
Typical brand names include Depakote, Depakene, and Stavzor, but the active ingredient is always the same molecule. Doctors usually start patients on a low dose and increase it gradually while monitoring blood levels - a practice called therapeutic drug monitoring.
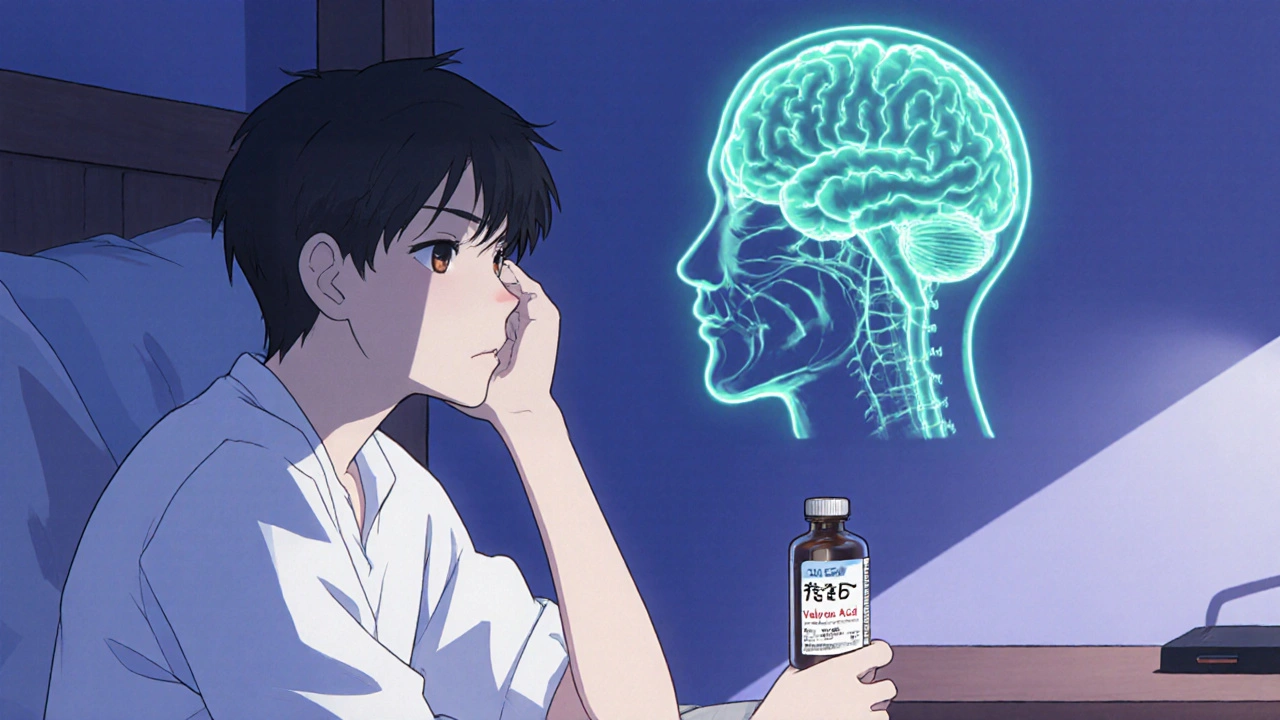
How Valproic Acid Works in the Brain
The drug’s primary action is to boost the availability of gamma‑aminobutyric acid (GABA), the main inhibitory neurotransmitter in the brain. By enhancing GABA, valproic acid dampens the excessive electrical firing that triggers seizures.
At the same time, this GABA boost can interfere with other neurotransmitter systems, especially serotonin and dopamine pathways that regulate mood. In simple terms, while the medication is turning down the volume on “seizure‑noise,” it can also mute the “feel‑good” signals that keep us emotionally balanced.
Researchers have identified several secondary mechanisms, such as inhibition of voltage‑gated sodium channels and modulation of histone deacetylase (HDAC) activity. These effects contribute to the drug’s mood‑stabilizing reputation, but they also add layers of complexity when side‑effects emerge.
Depression - A Quick Overview
Depression is a mood disorder characterized by persistent sadness, loss of interest, and a range of physical symptoms that can last weeks or months. The World Health Organization estimates that more than 260 million people worldwide live with depression, making it a leading cause of disability.
Biologically, depression is linked to reduced serotonin, norepinephrine, and dopamine activity, as well as inflammation and dysregulated stress hormones. Because many of these pathways overlap with the ones valproic acid touches, it’s not surprising that clinicians have reported mood changes in a subset of patients.
Clinical Evidence: Does Valproic Acid Trigger Depression?
Large‑scale studies paint a mixed picture. A 2021 meta‑analysis of 18 randomized controlled trials involving 3,200 patients with bipolar disorder found that 12 % of those on valproic acid reported new‑onset depressive symptoms, compared with 7 % on placebo. The relative risk was 1.7, indicating a moderate increase.
On the other hand, a 2023 longitudinal cohort of 1,150 epilepsy patients showed no statistically significant rise in depression scores after six months of therapy, provided the drug level stayed within the therapeutic range (50-125 µg/mL).
What’s consistent across studies is that the risk spikes when two conditions coexist: a history of mood disorders and high plasma concentrations of the drug. In practical terms, a patient with bipolar II who already struggles with low mood is more vulnerable than a teenager using valproic acid solely for seizure control.
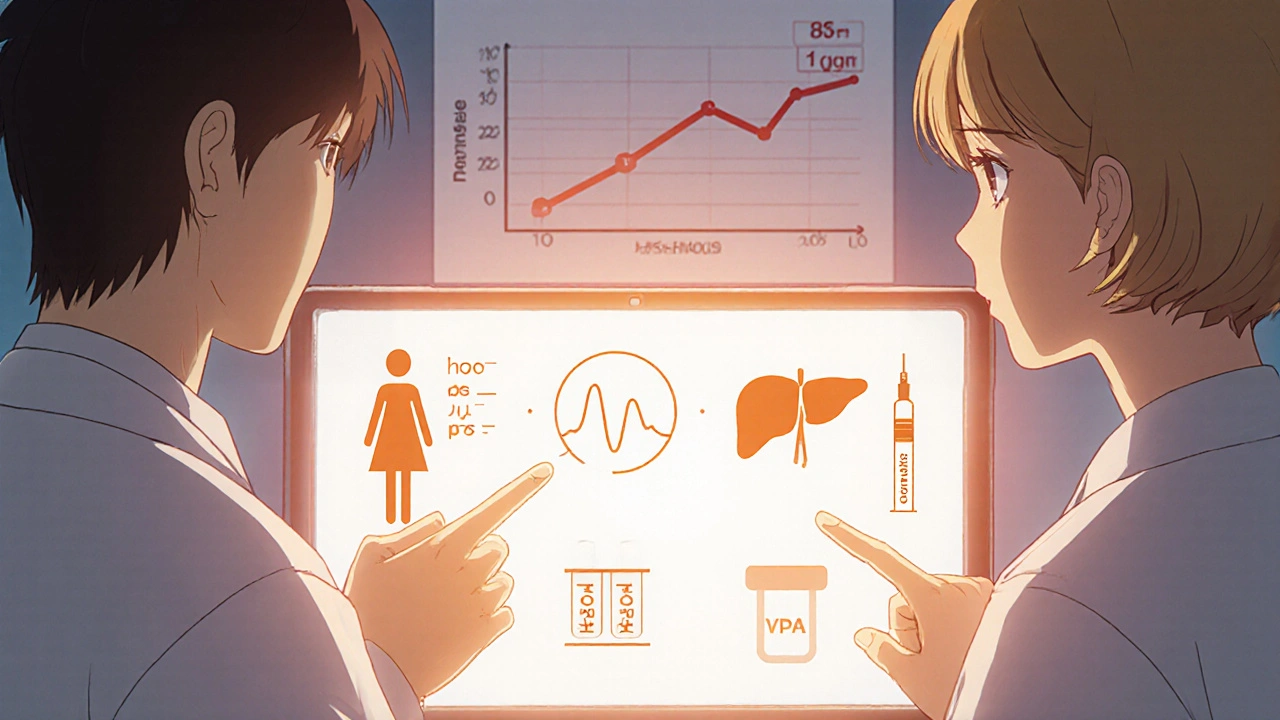
Who Is Most Likely to Experience Mood Changes?
- Bipolar disorder patients: The drug is used as a mood stabilizer, but paradoxically it can precipitate depressive episodes in up to 15 % of users.
- Women of child‑bearing age: Hormonal fluctuations can amplify mood swings, and valproic acid’s teratogenicity (risk of birth defects) adds stress that may manifest as depression.
- Individuals with liver enzyme abnormalities: Valproic acid is metabolized by the liver; impaired function can lead to higher blood levels and more side‑effects.
- People taking selective serotonin reuptake inhibitors (SSRIs) or other antidepressants: Drug‑drug interactions can alter serotonin pathways, sometimes worsening depressive symptoms.
Other risk markers include rapid dose escalation, poor medication adherence, and a family history of major depressive disorder.
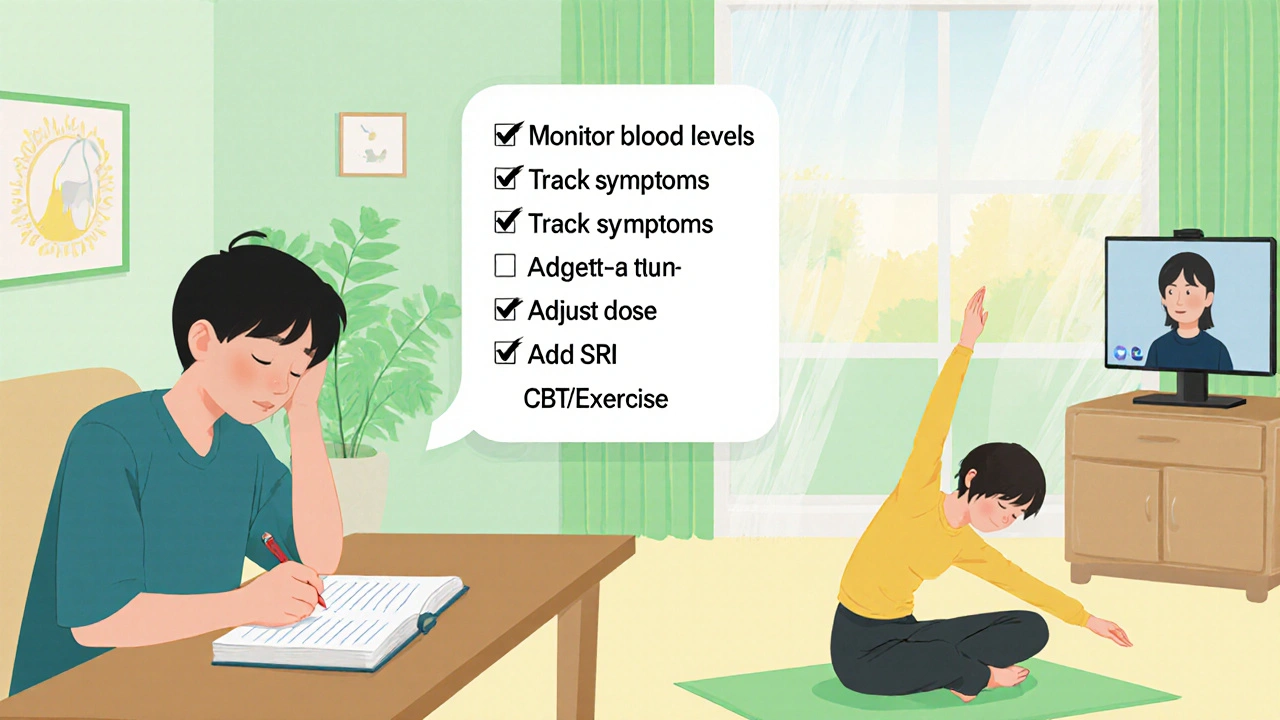
Managing Mood Changes While on Valproic Acid
- Regular monitoring: Schedule blood tests every 2-4 weeks after a dose change. Keep the level in the lower therapeutic window if you have a history of mood issues.
- Track symptoms: Use a simple mood diary or a mobile app to log daily feelings, sleep quality, and appetite. Patterns often emerge before a full‑blown depressive episode.
- Adjust the dose: If depressive symptoms appear, discuss a modest dose reduction with your clinician. Sometimes a 10-20 % cut can restore balance without sacrificing seizure control.
- Add or switch medications: Adding an SSRI (e.g., sertraline) can offset low serotonin, but be aware of interaction warnings. In some cases, switching to another mood stabilizer-such as lamotrigine or lithium-provides better mood coverage.
- Non‑pharmacologic support: Cognitive‑behavioral therapy (CBT), regular exercise, and consistent sleep schedules are proven to lower depression risk.
Never make changes on your own. A coordinated approach between neurologist, psychiatrist, and primary‑care provider yields the safest outcomes.
Comparison of Valproic Acid with Other Mood Stabilizers
| Medication | Primary Use | Depression Risk (%) | Key Advantages | Major Drawbacks |
|---|---|---|---|---|
| Valproic Acid | Epilepsy, Bipolar II | 12‑15 | Effective for rapid‑cycling bipolar, broad seizure coverage | Weight gain, teratogenic, liver toxicity |
| Lamotrigine | Bipolar I & II (depressive phase) | 3‑5 | Strong antidepressant effect, low sedation | Risk of Stevens‑Johnson rash, slower titration |
| Lithium | Classic mood stabilizer | 5‑8 | Reduces suicide risk, well‑studied | Kidney & thyroid impact, narrow therapeutic window |
| Carbamazepine | Partial seizures, bipolar III | 9‑11 | Good for mixed episodes | Induces liver enzymes, drug interactions |
The table shows that while valproic acid isn’t the highest risk option, it sits in the middle of the pack. For patients already prone to depression, lamotrigine often becomes the first‑line choice.
Quick Checklist for Patients and Clinicians
- Confirm baseline depression screening before starting valproic acid.
- Set a target plasma level (50-100 µg/mL for mood stabilization).
- Schedule mood check‑ins at weeks 2, 4, and 8 after dose changes.
- Review all concurrent meds for serotonin or liver‑enzyme interactions.
- Document any new depressive symptoms promptly; consider dose adjustment or adjunct therapy.
Following this checklist reduces surprise mood swings and helps keep treatment goals on track.
Frequently Asked Questions
Can valproic acid cause depression in everyone?
No. Most users tolerate the drug without mood changes. The risk is higher in people with a prior history of depression, bipolar disorder, or high blood levels of the medication.
How long does it take for depressive symptoms to appear?
Symptoms can emerge within a few weeks of starting therapy or after a rapid dose increase. Some patients notice changes only after several months when the drug accumulates.
Is it safe to combine valproic acid with an SSRI?
Generally it’s considered safe, but clinicians watch for serotonin syndrome and increased plasma levels. Starting the SSRI at a low dose and monitoring mood closely is the usual strategy.
Should I stop valproic acid if I feel sad?
Don’t stop abruptly. Sudden discontinuation can trigger seizures. Talk to your doctor first - they may lower the dose, add an antidepressant, or switch to another mood stabilizer.
Are there lab tests that predict depression risk?
While no test guarantees prediction, high liver enzymes (ALT, AST) and plasma valproic acid levels above 100 µg/mL correlate with more side‑effects, including mood disturbances.
Got more questions? Talk to your neurologist or psychiatrist - they can tailor the treatment plan to your unique situation.



eko lennon
25 October 2025 - 18:46 PM
When I first heard that valproic acid could be a double‑edged sword, I imagined a tiny pharmacist in my brain juggling tiny beakers, one labeled "seizure control" and the other "mood dampener." The reality is far more tangled, though. Valproic acid ramps up GABA, the brain's natural brake, which shuts down the hyper‑excitable neurons that cause seizures. At the same time, that increased inhibition can mute the dopamine and serotonin fireworks that keep us feeling motivated and upbeat. Clinical trials have shown roughly a dozen percent of patients develop depressive symptoms, a figure that jumps to nearly twenty percent in those with a pre‑existing mood disorder. It’s not just a coincidence; the drug also messes with voltage‑gated sodium channels and even the epigenetic landscape via HDAC inhibition. Those mechanisms can alter gene expression patterns linked to mood regulation. Blood levels matter, too-when concentrations creep above the therapeutic window, the risk of side‑effects spikes dramatically. Women of child‑bearing age face added stress because of teratogenic concerns, which can compound depressive feelings. Liver function is another hidden factor; impaired metabolism can let the drug linger longer, amplifying its mood effects. Some physicians recommend a cautious titration schedule, adding a slow ramp‑up over weeks rather than a sudden jump. Others suggest pairing valproic acid with a low‑dose SSRI as a safety net, but that requires careful monitoring for serotonin syndrome. Lifestyle tweaks-regular exercise, sleep hygiene, and CBT-can provide a valuable buffer against mood swings. If depression does set in, the first step is never to quit cold turkey; tapering under medical supervision is crucial to avoid seizure breakthrough. Switching to lamotrigine or lithium may be advisable for those who are particularly vulnerable. Ultimately, the decision to stay on valproic acid balances its seizure‑preventing power against the personal cost of mood disturbances, and that balance is different for every patient.
Sunita Basnet
31 October 2025 - 12:40 PM
Hey folks, just want to add that the GABAergic boost from valproic acid can be a real game‑changer for seizure control, but it also nudges the serotonergic axis downstream. In practice, keeping plasma levels in the lower therapeutic range (around 50‑100 µg/mL) often mitigates mood dip risk while preserving efficacy. Regular blood work and a simple mood diary can catch subtle shifts before they snowball.
Melody Barton
6 November 2025 - 07:33 AM
Bottom line: if you notice yourself feeling down after the dose goes up, talk to your doc right away. A small reduction or adding a gentle antidepressant can bring things back into balance without losing seizure protection.
Justin Scherer
12 November 2025 - 02:26 AM
Valproic acid does its job well for seizures, but it's wise to watch for mood changes, especially if you have a history of depression. Keeping an eye on blood levels and noting any shifts in sleep or appetite can be helpful.
Pamela Clark
17 November 2025 - 21:20 PM
Oh great, another “miracle drug” that also moonlights as a mood‑killer. Because what we really needed was another reason to over‑prescribe meds and then blame the patient when they feel crappy.
Diane Holding
23 November 2025 - 16:13 PM
Mood diaries are essential.
Cheyanne Moxley
29 November 2025 - 11:06 AM
Honestly, if you’re a woman of child‑bearing age and you’re willing to risk a future baby’s health for a drug that might make you depressed, you need to re‑evaluate your priorities. It's not just about you; it's about the next generation.
Kevin Stratton
5 December 2025 - 06:00 AM
We are all just neurochemical travelers, drifting through synaptic seas; valproic acid is but a tide that can lift or drown. 🌊🤔
Manish Verma
11 December 2025 - 00:53 AM
Look, in our country we pride ourselves on top‑notch healthcare, yet we still push drugs like valproic acid without fully warning patients about the mood fallout. It's high time our med boards step up and give the full picture.
Donal Hinely
16 December 2025 - 19:46 PM
Imagine a kaleidoscope of brain chemistry where each twist of valproic acid paints new shades-some bright, some haunting. That’s the beauty and the horror of neuropharmacology.
christine badilla
22 December 2025 - 14:40 PM
Drama alert: the drug that saves you might also steal your smile!