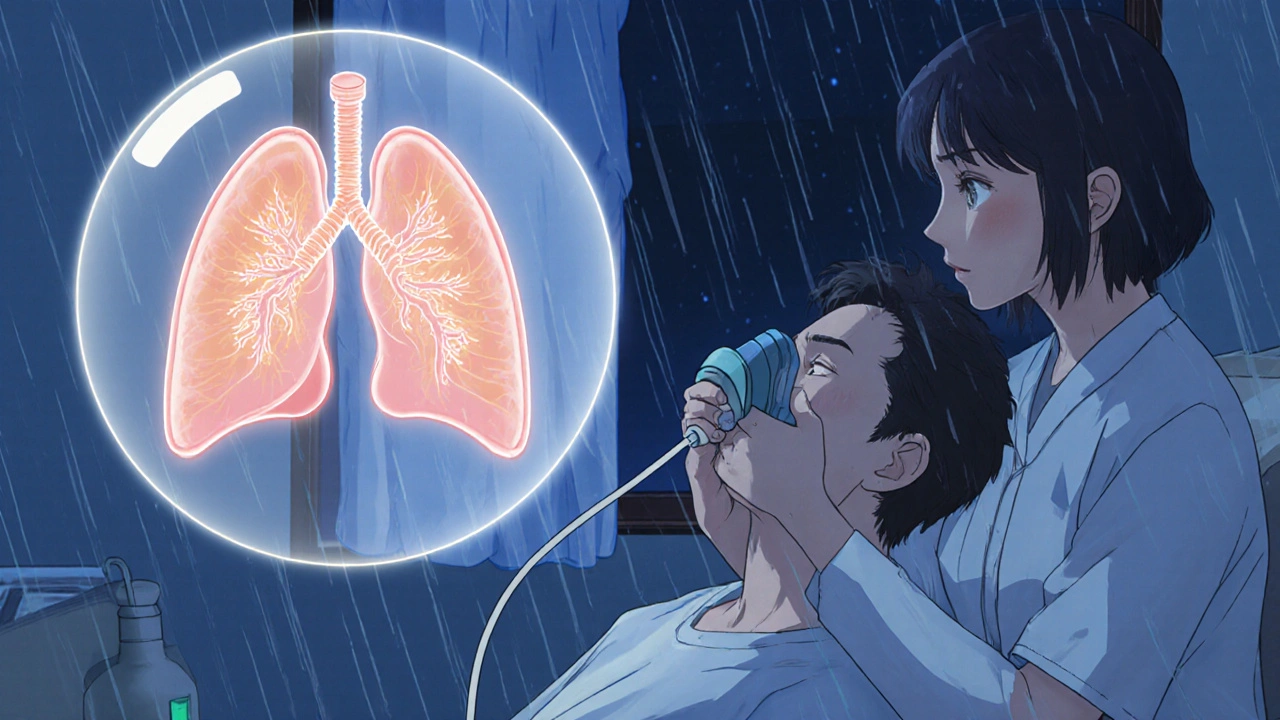
If you’ve been coughing up mucus every day for months - or years - and it’s getting harder to breathe during simple tasks like walking to the mailbox or climbing stairs, you might be dealing with chronic bronchitis. It’s not just a bad cold that won’t go away. This is a serious, long-term lung condition that affects millions in the U.S., and the biggest cause? Smoking.
What Chronic Bronchitis Really Feels Like
Chronic bronchitis isn’t defined by a single symptom. It’s a pattern: a daily cough that brings up mucus, lasting at least three months a year for two years in a row. You’re not imagining it. The airways in your lungs are swollen, irritated, and producing way too much mucus. That thick, sticky phlegm clogs your breathing tubes, making it harder to get air in and out.Most people with chronic bronchitis also feel short of breath during activity - 82% do, according to the Mayo Clinic. You might notice wheezing, chest tightness, or just constant fatigue. These aren’t minor inconveniences. They limit your life. Many patients say they stop going to family gatherings, skip walks with friends, or avoid even light housework because they’re afraid they’ll run out of breath.
And it gets worse. People with chronic bronchitis are over three times more likely to get serious lung infections like pneumonia. Each infection can send you to the hospital and speed up the damage to your lungs. The good news? You can stop the cycle - and it starts with one thing: quitting smoking.
Why Smoking Is the Main Culprit - and Why Quitting Changes Everything
Over 90% of people diagnosed with chronic bronchitis have smoked - or used to smoke. That’s not a coincidence. Cigarette smoke doesn’t just irritate your lungs; it destroys the tiny hair-like structures (cilia) that normally sweep mucus out of your airways. Without them, mucus builds up. The constant irritation turns your bronchial tubes into inflamed, overactive mucus factories.But here’s the most powerful fact: quitting smoking is the only treatment proven to slow down the disease. A 30-year study found that current smokers had a 42% chance of developing chronic bronchitis. Former smokers? Only 26%. And if you quit after diagnosis, your disease progression slows by 60% compared to those who keep smoking, according to Dr. John Walsh of the COPD Foundation.
It’s not about willpower alone. Most people who try to quit on their own fail. But when they get help - counseling, nicotine patches, or medications like varenicline - their success rate jumps from 7% to 45% in just six months. And it’s not just about breathing better. Quitting reduces your risk of lung infections, heart disease, and early death. Your lungs don’t fully heal, but they stop getting worse. That’s huge.
What Treatments Actually Work - And What Doesn’t
There’s no cure for chronic bronchitis. But there are treatments that help you live better. Not all of them are right for everyone.Bronchodilators - usually inhaled - are the first line of defense. They relax the muscles around your airways, letting more air flow. Short-acting versions work in 15 minutes and last 4-6 hours. Long-acting ones are used daily to keep symptoms under control. These are widely recommended and effective.
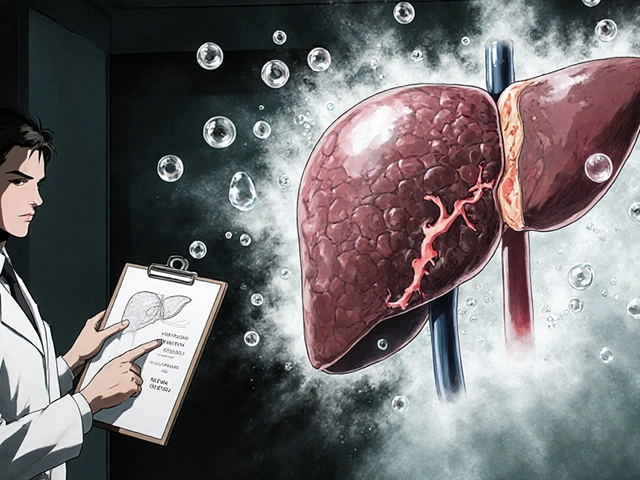
Inhaled steroids can reduce inflammation, but they come with risks. Long-term use increases your chance of osteoporosis by 23%, high blood pressure by 18%, and diabetes by 15%. Many patients regret using them without knowing these side effects. One 65-year-old patient on PatientsLikeMe developed two broken spine bones after 18 months on steroids, even with calcium supplements.
Mucolytics like N-acetylcysteine help thin mucus so it’s easier to cough up. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends them. But the American College of Chest Physicians says there’s not enough proof they help in stable patients. So it’s a gray area - talk to your doctor about whether it’s right for you.
Antibiotics are only for bacterial infections - not for daily cough. If you’re coughing more than usual, with yellow or green mucus and a fever, you might have an infection. Amoxicillin-clavulanate works in 82% of these cases, according to clinical guidelines.
Oxygen therapy is life-saving for those with very low oxygen levels. If your blood oxygen drops below 88%, using oxygen 15+ hours a day can increase your 5-year survival by 21%. But many patients don’t use it as prescribed - only 62% stick with it.
Pulmonary Rehabilitation: The Secret Weapon Most People Skip
If you’ve never heard of pulmonary rehab, you’re not alone. But it’s one of the most effective tools you have.This isn’t just exercise. It’s a full program: breathing techniques, nutrition advice, education about your condition, and supervised physical training. Patients who complete it walk 78 meters farther in six minutes on average. Hospital visits drop by 37%. And 78% of participants report feeling more confident doing daily tasks.
Dr. MeiLan Han from the University of Michigan says pulmonary rehab should be standard for every chronic bronchitis patient - no matter how mild or severe their symptoms. Yet only a small fraction get referred to it. Ask your doctor. If they don’t mention it, ask again. It’s covered by Medicare and most insurance plans.
Smoking Cessation Support: Why You Need More Than Willpower
Quitting smoking is the most important step - but it’s also the hardest. That’s why professional support makes all the difference.Patients who get structured help - like counseling, nicotine replacement, and medication - have a 68% success rate in quitting, according to the COPD Foundation. Those who try alone? Only 22% succeed.
Here’s what works:
- Nicotine patches or gum - helps reduce withdrawal cravings.
- Varenicline (Chantix) - reduces both cravings and the pleasure you get from smoking.
- Behavioral counseling - even a few sessions with a counselor increases your odds of staying quit.
- Combining methods - using medication plus counseling gives the best results.
Many people think they’ve failed if they relapse. But quitting is often a process. Most people try several times before they succeed. The key is not to give up - and to get help every time you try.

What to Watch Out For
Managing chronic bronchitis isn’t just about meds and quitting smoking. Daily habits matter too.- Inhaler technique - 38% of patients use their inhalers wrong. That means they’re not getting the full dose. Ask your respiratory therapist to watch you use it. You might need 4-5 sessions to get it right.
- Vaccinations - get the flu shot every year. It cuts your risk of flare-ups by 42%. Also get the pneumococcal vaccine every 5-7 years to prevent pneumonia.
- Avoid irritants - secondhand smoke, strong cleaning fumes, air pollution, and dust can trigger flare-ups. Use air purifiers indoors and wear a mask outdoors on bad air days.
- Stay active - even walking 10 minutes a day helps. Home exercise programs have a 41% dropout rate, so find someone to do it with - a friend, family member, or online group.
The Big Picture: Costs, Research, and Hope
Chronic bronchitis costs Medicare $32.1 billion a year. But investing in prevention pays off. Every $1 spent on smoking cessation programs saves $5.60 in healthcare costs within two years.New treatments are coming. In 2023, the FDA approved ensifentrine - a new inhaled drug that improved breathing and reduced flare-ups in clinical trials. Researchers are also studying gene variants that affect mucus clearance, which could lead to personalized treatments.
But the most powerful tool hasn’t changed. Quitting smoking. Getting pulmonary rehab. Sticking with your plan. These aren’t optional extras - they’re the foundation of living longer and better with chronic bronchitis.
What’s Next? Start Here
If you have chronic bronchitis:- Ask your doctor for a referral to pulmonary rehabilitation.
- Set a quit date for smoking - and sign up for a cessation program today.
- Learn how to use your inhaler correctly - don’t guess, get trained.
- Get your flu and pneumonia vaccines if you haven’t already.
- Join a support group - online or in person. You’re not alone.
If you’ve never smoked but have a chronic cough and mucus - see a doctor. It could be chronic bronchitis, and early action makes a difference.
Is chronic bronchitis the same as COPD?
Chronic bronchitis is one type of COPD - along with emphysema. COPD is the umbrella term for lung diseases that cause blocked airflow. If you have chronic bronchitis with airflow obstruction, you have COPD. Not everyone with a long-term cough has COPD - but if your lungs aren’t clearing air properly, you likely do.
Can I still live a normal life with chronic bronchitis?
Yes - but it takes effort. Many people with chronic bronchitis live for decades after diagnosis, especially if they quit smoking, do pulmonary rehab, and follow their treatment plan. One 58-year-old former smoker said after six months of rehab and quitting, he could walk to the end of his street without stopping - something he hadn’t done in three years. Your life doesn’t have to end with this diagnosis.
Do I need oxygen therapy forever?
Not necessarily. Oxygen is prescribed only if your blood oxygen levels are consistently low. Some people need it 24/7, others only during sleep or exercise. If you quit smoking and improve your lung function through rehab, your oxygen needs may decrease over time. Your doctor will retest you regularly.
Why do I still cough after quitting smoking?
Your lungs are cleaning themselves. After years of smoke damage, the cilia (tiny cleaners in your airways) start to recover - and they begin pushing out years of built-up mucus. This can cause a temporary increase in coughing for weeks or months. It’s a good sign - your lungs are healing.
Is it too late to quit if I’ve smoked for 40 years?
It’s never too late. Even people who quit after age 60 reduce their risk of death from lung disease by 30-50%. Your lungs won’t return to how they were at 20, but they will stop deteriorating as fast. You’ll breathe easier, have fewer infections, and feel more energy. Quitting at any age adds years - and better quality - to your life.


Dana Dolan
20 November 2025 - 17:38 PM
I’ve had this for 8 years now. Quit smoking 2 years ago and my cough is still there, but at least I can walk to the store without stopping. The mucus is less thick too. My doctor said my lungs are healing, even if it’s slow.
Still hate the inhaler. Can’t get the technique right no matter how many times they show me.
Reema Al-Zaheri
22 November 2025 - 07:01 AM
Chronic bronchitis is not a death sentence, but it is a lifelong management condition. The data presented here is statistically sound, particularly regarding pulmonary rehabilitation’s impact on six-minute walk distance and hospitalization rates. I commend the inclusion of GOLD and ACCP guidelines, as they reflect evidence-based practice. However, the omission of long-term corticosteroid effects on adrenal suppression is concerning.
Michael Salmon
23 November 2025 - 00:12 AM
Oh wow, another ‘quit smoking and you’ll be fine’ fairy tale. You know what? I’ve been smoking for 45 years and I’m still running marathons. Your ‘90% of patients are smokers’ stat ignores the fact that 20% of non-smokers get COPD too. You’re scaring people into guilt trips, not helping them.
Also, pulmonary rehab? That’s just expensive cardio with a clipboard. My gym trainer does better.
Joe Durham
24 November 2025 - 19:24 PM
Michael, I hear you. I’ve known people who smoked for decades and stayed active. But for most of us, the damage adds up quietly. I lost my dad to this, and he never thought it would get this bad. He didn’t want to quit because he thought it was too late. But he would’ve had more good days if he’d tried.
It’s not about blame. It’s about giving people options. Even if you’re skeptical, the rehab stats are real. I saw a guy at my clinic go from needing oxygen to walking his dog again. That’s not magic. That’s medicine.
Derron Vanderpoel
26 November 2025 - 15:36 PM
OMG I JUST QUIT AFTER 30 YEARS AND MY COUGH IS WORSE???!?!?!
I thought quitting would make it stop but now I’m coughing up black stuff like a steam engine. Is this normal?? I’m scared. I feel like my lungs are trying to claw their way out. I’m watching YouTube videos of people coughing up phlegm and now I’m crying. I didn’t sign up for this.
Is this the healing? I thought I’d feel better right away. Why is my chest so tight??
Timothy Reed
27 November 2025 - 07:38 AM
It’s completely normal to experience increased coughing after quitting smoking. The cilia in your airways, which were paralyzed by smoke, are now regaining function and actively clearing decades of accumulated mucus and debris. This phase typically lasts 4–12 weeks and is a sign of recovery, not deterioration.
Hydration, steam inhalation, and controlled breathing exercises can help manage the discomfort. Consider reaching out to a pulmonary rehab program - they offer specific techniques for this transition. You’re not alone in this.
Christopher K
27 November 2025 - 11:09 AM
Oh great. Another government-funded guilt trip disguised as medical advice. Quit smoking? Yeah, sure. Like I’m supposed to listen to some doctor who got paid by Big Pharma to push Chantix.
Meanwhile, my neighbor smokes 2 packs a day and still lifts weights at 70. Maybe the real problem is that people are too lazy to breathe on their own anymore. Why are we treating lungs like fragile porcelain?
harenee hanapi
29 November 2025 - 10:50 AM
Everyone says quit smoking but no one talks about how lonely it is. I tried to quit three times and every time I felt like everyone was watching me, judging me. My husband laughed when I said I wanted to stop. My kids act like I’m a criminal now. I’m not a bad person. I just like the way it feels. Why is everyone so mean?
And now I have to go to ‘rehab’? Like I’m a drug addict? I’m just trying to breathe. Why can’t anyone just be kind?
Christopher Robinson
30 November 2025 - 20:32 PM
Hey, I just want to say you’re not alone 🤍
I’ve been in your shoes. Coughing up black gunk after quitting? That’s your lungs doing a deep clean. It’s gross, it’s weird, but it’s GOOD.
I started using a humidifier and sipping warm tea with honey. Also, I joined a Reddit group for ex-smokers with COPD - it saved my sanity. You’re healing. Keep going. One day at a time 💪
James Ó Nuanáin
1 December 2025 - 01:45 AM
It is, of course, an incontrovertible fact that the British National Health Service has demonstrated superior outcomes in pulmonary rehabilitation adherence rates compared to U.S. models, primarily due to centralized care coordination and universal access. The notion that ‘it’s never too late to quit’ is empirically validated in the 2021 Lancet longitudinal cohort study, which demonstrated a 41% reduction in all-cause mortality among smokers who ceased after age 65. That said, the overreliance on pharmacological interventions such as varenicline remains questionable, given its association with neuropsychiatric side effects in 8.3% of users. A more holistic approach - incorporating mindfulness, respiratory physiotherapy, and nutritional optimization - is preferable.
Nick Lesieur
1 December 2025 - 02:04 AM
So let me get this straight - I’m supposed to believe that some guy in a lab coat wrote this whole thing to help me? Nah. I’ve seen these ‘miracle cures’ before. First they tell you to quit, then they sell you a $300 inhaler, then they want you to pay for ‘rehab’ like it’s a spa retreat.
Meanwhile, my cousin’s brother-in-law’s dog has better lung function than me - and that dog doesn’t even have lungs. Just saying.
Angela Gutschwager
1 December 2025 - 05:39 AM
I quit. Cough got worse. Now I’m scared. What if I’m dying?