Liver disease: signs, causes, testing and what you can do
Your liver does a lot — filters blood, makes bile, stores nutrients. When it starts to fail, things change slowly or fast. This page gives clear, practical steps to spot problems, understand common causes, and know what to do next.
Common causes include viral hepatitis (A, B, C), alcohol-related liver disease, nonalcoholic fatty liver disease (NAFLD), and medication or toxin damage. Many people also have genetic or autoimmune conditions that affect the liver. If you take multiple medications, herbals, or drink heavily, mention that to your doctor — it matters.
Key symptoms to watch for
Liver issues often start quietly. Look for persistent fatigue, yellowing of the skin or eyes (jaundice), dark urine, pale stools, abdominal pain or swelling, itchy skin, unexplained weight loss, or easy bruising. Don’t ignore ongoing digestive problems, nausea, or chronic bloating—these can be early signs.
None of these symptoms prove liver disease on their own, but together they raise the chance. If symptoms last more than a week or get worse, see a clinician for testing rather than guessing online.
How testing and diagnosis work
Your doctor will usually start with a simple blood panel called liver function tests (LFTs). These check enzymes like ALT, AST, alkaline phosphatase, and bilirubin. Abnormal results may lead to imaging like ultrasound, CT, or MRI, and sometimes a liver biopsy to check tissue directly. Viral hepatitis tests and autoimmune markers can narrow down the cause.
Treatment depends on the cause. For viral hepatitis there are effective antiviral drugs. For NAFLD, weight loss, exercise, and controlling diabetes or cholesterol help. Alcohol-related liver disease requires stopping alcohol and medical support. Some drug-induced injuries get better after stopping the offending medicine. In advanced cases, transplant may be discussed.
You can take practical steps now: avoid binge drinking, keep vaccines up to date (hepatitis A and B), maintain a healthy weight, and ask your doctor about medication side effects. Be careful with supplements and herbal pills — many people assume natural means safe, but some herbs can harm the liver.
When managing medicines, use one pharmacy if possible and show your full medication list to healthcare providers. Tools like price apps and pharmacist advice can help you get needed drugs safely and affordably. If you need tests or prescriptions, ask about cheaper options or assistance programs.
If you have abnormal lab results, get a second opinion when unsure. Liver disease can be managed well when caught early. Act sooner rather than later — small changes now can prevent big problems later.
Regular monitoring matters if you already have liver disease. Most doctors ask for blood tests every 3–6 months, and imaging once a year for people at higher risk of scarring or cancer. Keep a simple log of symptoms and meds between visits so you can spot trends. If you develop swelling, confusion, or bleeding, go to the emergency room — those are signs of advanced disease that need urgent care. Get care early often.
Chronic Hepatitis C and Alcohol: Risks You Need to Know
Learn how alcohol worsens chronic hepatitis C, impacts liver health, and reduces treatment success. Get clear guidelines to protect your liver and improve cure rates.
Read More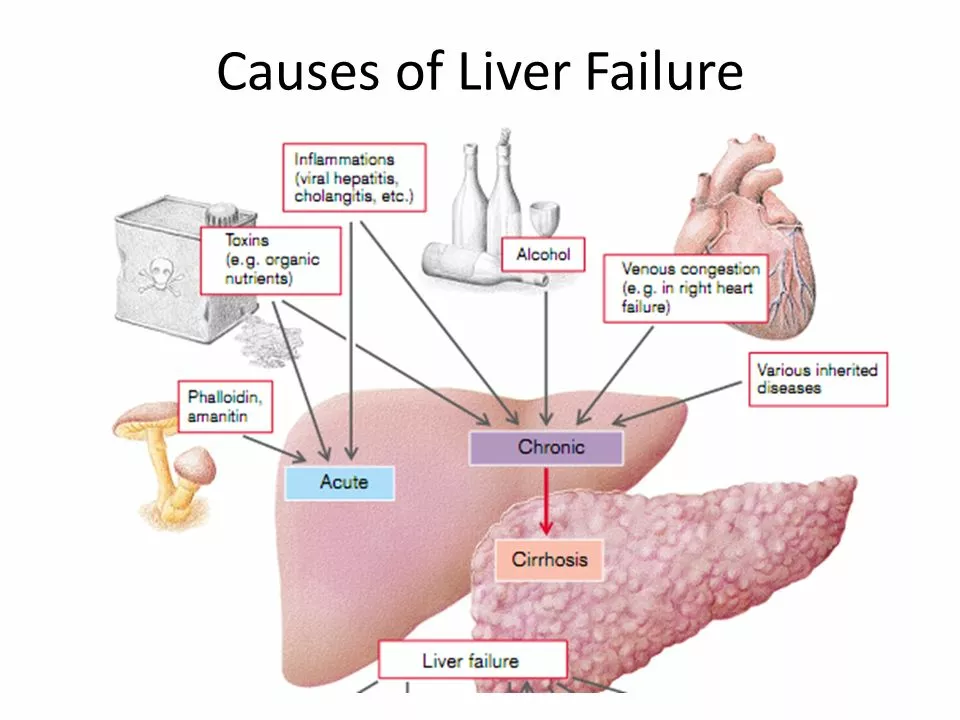
Heparin sodium and liver disease: What patients need to know
As someone who's been researching heparin sodium and liver disease, I feel it's important to share some key information with fellow patients. Heparin sodium is a blood-thinning medication often prescribed to prevent blood clots. However, individuals with liver disease should be cautious, as their ability to metabolize and eliminate the drug may be compromised. This could lead to increased risk of bleeding or other complications. Always consult your doctor before starting any new medications, and be sure to discuss your liver disease and any potential concerns.
Read More