Brand Name Drugs: What They Are, How They Differ from Generics, and What You Need to Know
When you hear brand name drugs, original medications developed and marketed by pharmaceutical companies under a proprietary name. Also known as proprietary drugs, they’re the first version of a medicine to hit the market after years of research and clinical trials. These are the pills you see advertised on TV—like Rybelsus, Ozempic, or Elavil—sold under a specific brand and protected by patents. They’re not just names on a bottle; they represent years of investment, legal protection, and controlled supply. But here’s the thing: once that patent runs out, the same exact drug can be sold for a fraction of the price under a different name. That’s where generic drugs, medications containing the same active ingredient as brand name drugs, approved by the FDA after patent expiration come in.
Why do brand name drugs cost so much more? It’s not because they work better. It’s because the company that made them had to pay for research, testing, FDA approval, and marketing—all of which can cost over a billion dollars. Once the patent expires, other companies can copy the formula without repeating those costs. That’s why patent expiration, the legal end of exclusive rights to sell a drug, allowing competitors to enter the market is such a big deal. It’s when prices drop, sometimes by 80% or more. But here’s what most people don’t realize: even after patents expire, brand name versions often stay on the market, sometimes with minor tweaks to extend exclusivity. This is called “evergreening,” and it keeps prices high even when generics are available.
And it’s not just about cost. Brand name drugs are often the first to be studied in large populations, which means doctors have more long-term data on them. But generics? They’re held to the same FDA standards for safety and effectiveness. The only differences are the inactive ingredients—fillers, colors, shapes—which rarely affect how the drug works. Still, some patients report feeling different on a generic, and that’s worth talking to your doctor about. It’s not always the drug—it could be your body adjusting to a new filler.
So when you’re choosing between a brand name drug and its generic version, ask yourself: is the higher price giving you something real, or just a familiar label? The truth is, for most people, the generic is just as safe and just as effective. But if you’re on a complex treatment plan—like with carbamazepine or anticoagulants—where small differences in absorption matter, your doctor might recommend sticking with the brand. That’s where understanding drug pricing, the cost structure of medications shaped by patents, competition, and market control and pharmaceutical patents, legal protections that give companies exclusive rights to sell a drug for a set period helps you make smarter choices.
Below, you’ll find real-world guides on how these systems affect what you pay, what you get, and how to protect yourself when switching between brand and generic. Whether you’re trying to save money on diabetes meds, understand why your painkiller suddenly changed, or figure out why some drugs never get cheaper—this collection has the answers you won’t find on a pharmacy shelf.
Addressing Patient Concerns About Generic Medications: Common Questions Answered
Get clear, factual answers to common concerns about generic medications. Learn why generics are just as safe and effective as brand-name drugs, how they're regulated, and when to ask your doctor about switching.
Read More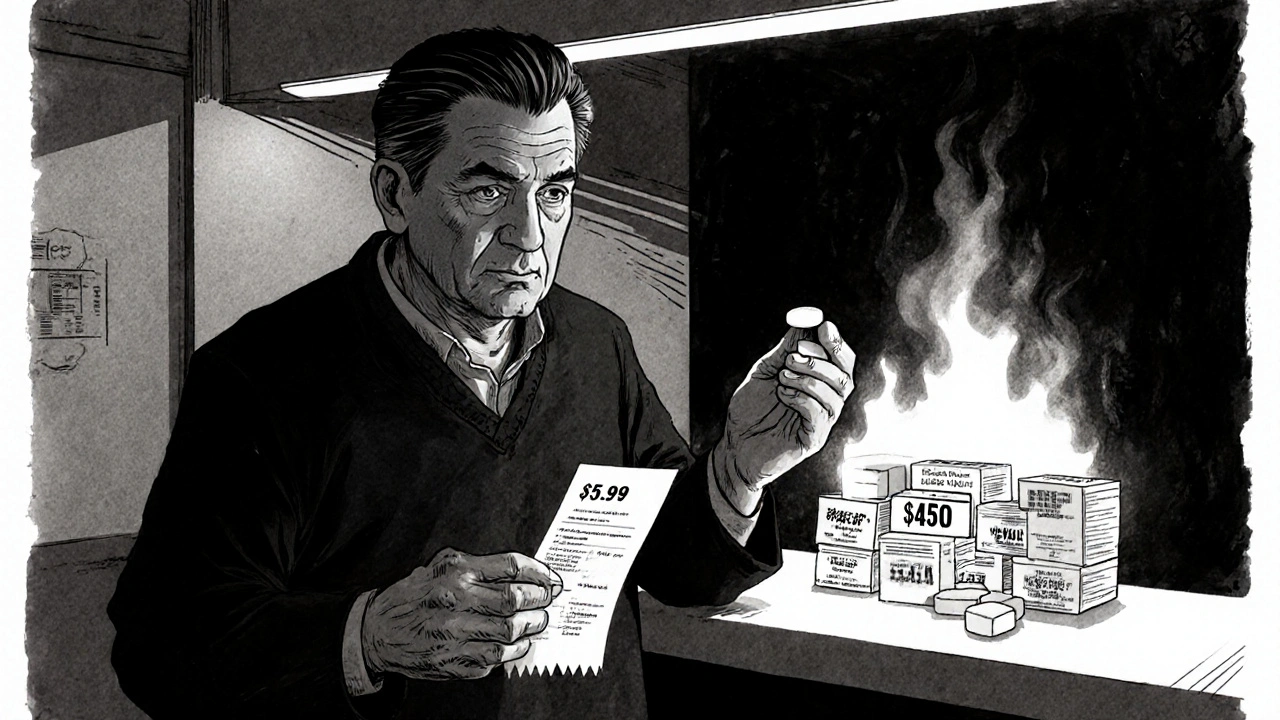
How Generic Medications Save Thousands on Healthcare Costs
Generic medications save billions annually in the U.S. healthcare system, offering the same effectiveness as brand-name drugs at up to 90% lower cost. Learn how generics work, where to find the best prices, and why they’re essential for affordable care.
Read More