Every year, Americans spend over $600 billion on prescription drugs. And yet, most of those prescriptions are for generic medications - the same drugs, at a fraction of the price. If you’ve ever been handed a small white pill with a code stamped on it instead of a flashy brand name, you’ve used a generic. And if you’ve paid less than $10 for it, you’ve saved money - probably hundreds, maybe thousands, over the year.
What Exactly Are Generic Medications?
Generic medications are exact copies of brand-name drugs, approved by the FDA after the original patent expires. They contain the same active ingredients, work the same way in your body, and are held to the same strict standards for safety and effectiveness. The FDA requires generics to be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same rate as the brand version. There’s no difference in how they work.
Think of it like buying store-brand cereal instead of the name-brand version. Same ingredients, same nutrition, different label. The FDA’s Orange Book lists over 12,000 generic drugs with an AB rating - meaning they’re therapeutically equivalent to the brand. About 98% of approved generics fall into this category.
How Much Do Generics Actually Save?
The numbers are staggering. In 2022, generic drugs saved the U.S. healthcare system $408 billion. That’s up from $373 billion the year before. Over the past decade, generics and biosimilars have saved over $2.9 trillion. That’s more than the annual GDP of most countries.
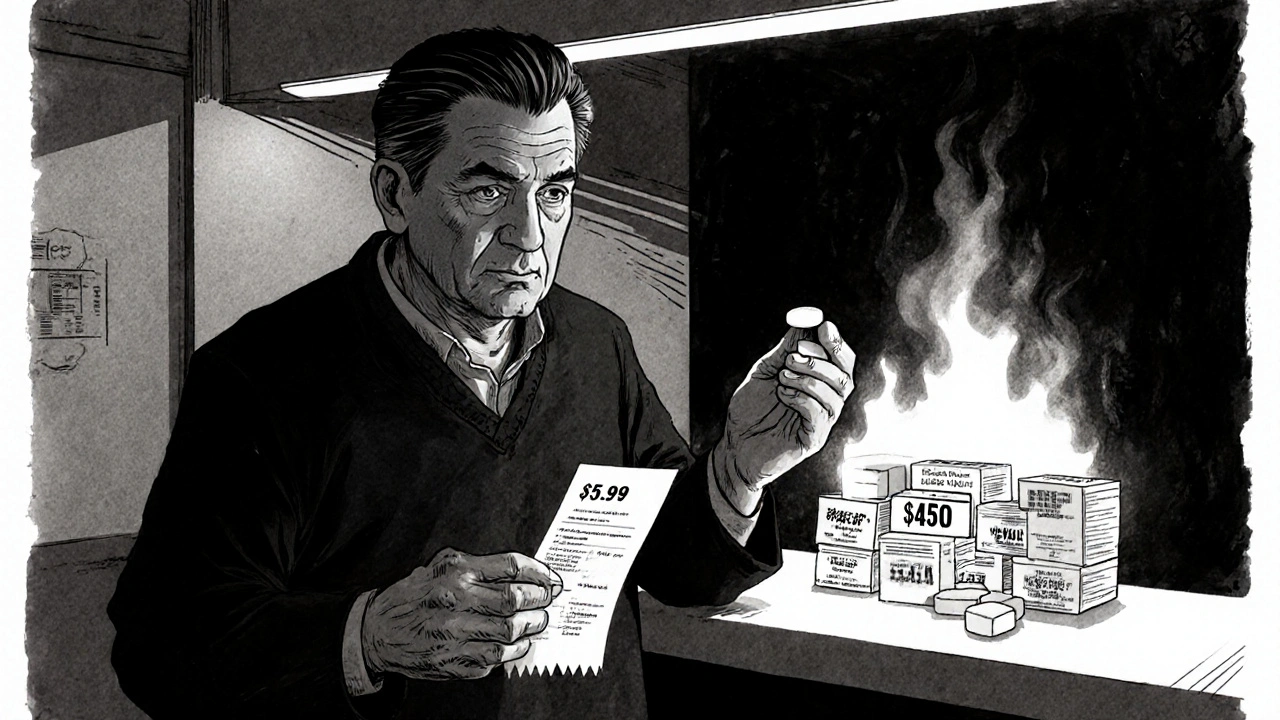
At the pharmacy counter, the difference is even more obvious. The average copay for a generic is $6.16. For a brand-name drug? $56.12. That’s more than nine times more. And 93% of generic prescriptions cost under $20. Only 59% of brand-name prescriptions do.
Take sertraline, the generic version of Zoloft. One patient on Reddit reported paying $9 for the generic versus $450 for the brand. That’s not an outlier - it’s standard. A 2022 study in Colorado found that some high-cost generics were 15.6 times more expensive than other generics treating the same condition. Switching to a lower-cost generic within the same drug class could save 88% on those prescriptions.
Why Are Brand-Name Drugs So Expensive?
Brand-name drugs cost more because of marketing, patents, and profit margins - not because they’re better. Pharmaceutical companies spend billions developing new drugs and recoup those costs by charging high prices during the patent window. Once the patent expires, other companies can make the same drug. That’s when prices drop - often by 80% to 85% within the first year.
Even though generics make up 90% of all prescriptions filled in the U.S., they account for only 1.5% of total drug spending. Brand-name drugs, which make up just 10% of prescriptions, still take up 82% of drug expenditures. That’s not because they’re more effective. It’s because they’re priced that way.
Who Benefits the Most From Generics?
Everyone does - but not everyone feels it equally.
Medicare beneficiaries filled 91% generic prescriptions in 2022, yet 41% still struggled to afford them. Why? Because even though the drug itself costs $5, the copay might be $20 due to how insurance plans are structured. Some plans have high deductibles or don’t count generic copays toward out-of-pocket maximums. That’s why the 2023 Inflation Reduction Act capped Medicare Part D out-of-pocket costs at $2,000 a year - it’s meant to make those savings real for seniors.
Private insurance plans also benefit. In 2022, commercial insurers saved $194 billion thanks to generics. Employers who offer health benefits see lower premiums because drug costs are a major driver of those increases.
And then there are the patients who can’t afford brand-name drugs at all. For people with chronic conditions like high blood pressure, diabetes, or depression, generics aren’t just a cost-saving option - they’re the only way to stay on treatment.
Are There Times When Generics Don’t Work?
Most of the time, yes - they work just as well. But there are exceptions.
Drugs with a narrow therapeutic index - where even a small change in dosage can cause harm - are more carefully monitored. Examples include levothyroxine (for thyroid disease), warfarin (a blood thinner), and some epilepsy medications. A small percentage of patients report feeling different when switching from brand to generic for these drugs. In one Drugs.com survey, 15% of users said they had issues with generic levothyroxine.
That doesn’t mean the generic is unsafe. It means some people are more sensitive to small variations. In those cases, doctors may prescribe the brand - but only after trying the generic and confirming it works. Most patients do fine with the generic.
And while rare, manufacturing quality issues do happen. But the FDA inspects every generic plant - the same way they inspect brand-name ones. The vast majority of generics come from facilities that meet the same standards as the original makers.
How to Get the Most Out of Generic Medications
You don’t have to wait for your doctor to suggest a generic. You can take action right now.
- Ask your doctor: "Is there a generic version of this medication?" If they say no, ask why. Often, it’s just habit - not medical necessity.
- Use the FDA’s Orange Book or the AAM’s online formulary tools to check if a generic exists and if it’s rated AB (therapeutically equivalent).
- Compare prices at different pharmacies. A generic that costs $15 at CVS might be $5 at Walmart or Costco. Many chains offer $4 generic lists for common medications.
- Ask about therapeutic substitution. Sometimes, a different generic drug in the same class - like switching from one statin to another - can be far cheaper and just as effective.
- Don’t assume your insurance will automatically choose the cheapest option. Call your plan and ask which generic is covered at the lowest tier.
Pharmacists are trained to help with this. If you hand them a brand-name prescription, they can often substitute a generic automatically - unless your doctor specifically says "dispense as written." In 49 states, pharmacists can make that switch without asking. In New York, they need the doctor to indicate it’s okay.
The Bigger Picture: Why Generics Matter
The U.S. pays 2.78 times more for prescription drugs than other wealthy countries. That’s not because we’re sicker. It’s because our system allows drug prices to stay high. Generics are one of the few tools we have to push back.
Without generics, millions of people would skip doses, split pills, or go without treatment entirely. A 2022 study from Johns Hopkins found that switching from high-cost generics to lower-cost alternatives could save $15 billion a year - just by choosing smarter options within the generic category.
And it’s not just about money. It’s about access. When a patient can afford their medication, they’re more likely to take it. That means fewer hospital visits, fewer complications, and better health outcomes.
What’s Next for Generic Drugs?
The market is growing. The global generic drug market is expected to hit $665 billion by 2029. In the U.S., companies like Teva, Viatris, and Amneal dominate the market, with thousands of new generics approved every year.
Biosimilars - generic versions of complex biologic drugs - are starting to enter the market. They’re not as simple as a pill you swallow, but they’re already saving billions on cancer and autoimmune treatments. The FDA is pushing to speed up their approval.
But there are threats. Drug shortages are rising - 78% of the 312 active shortages in September 2023 were for generic drugs. Some of that’s due to manufacturing issues, but a big part is patent abuse. Brand-name companies file dozens of patents to delay generic entry - sometimes for drugs that haven’t changed at all.
Still, the trend is clear: generics are here to stay. And as more people learn how much they save - and how reliable they are - the gap between brand and generic will keep shrinking.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for safety, strength, purity, and effectiveness as brand-name drugs. They use the same active ingredients and are tested to ensure they work the same way in your body. Over 98% of generics are rated AB - meaning they’re therapeutically equivalent.
Why do some people say generics don’t work as well?
A small number of patients report differences with drugs that have a narrow therapeutic index - like thyroid medication or blood thinners. This doesn’t mean the generic is faulty. It means their body is sensitive to tiny changes in dosage. In these cases, doctors may stick with the brand - but only after trying the generic and confirming it works. Most patients have no issues at all.
Can I ask my pharmacist to switch me to a cheaper generic?
Yes - and they often will. In 49 states, pharmacists can automatically substitute a generic for a brand-name drug unless the doctor writes "dispense as written." Even if your prescription is for a brand, ask your pharmacist if a cheaper generic is available. Many pharmacies have $4 or $10 generic lists for common medications.
Why is my generic still expensive?
Even if the drug costs $5, your copay might be higher due to your insurance plan’s structure. Some plans don’t count generic copays toward your deductible, or they charge higher copays for non-preferred generics. Call your insurer and ask: "Which generic version of this drug is on my plan’s lowest tier?" You might be able to switch to a cheaper one.
Do generics take longer to work?
No. Generics must be bioequivalent - meaning they enter your bloodstream at the same rate and in the same amount as the brand. If your brand-name drug takes 30 minutes to start working, so will the generic. Any difference in how quickly you feel better is likely due to your body’s response, not the drug itself.



daniel lopez
20 November 2025 - 03:50 AM
Let me tell you something the FDA doesn't want you to know - generics are often made in the same factories as brand names, just with different labels. Big Pharma pays off regulators to delay generics, and then they buy up the generic makers to control the market. You think you're saving money? You're just paying the same company under a different name. And don't get me started on how they manipulate patent laws to block competition for decades. This isn't healthcare - it's a rigged casino.
Nosipho Mbambo
21 November 2025 - 16:51 PM
Wow. Just... wow. I mean, I get it, right? But also, why is this even a thing? Like, why do we let companies charge $450 for a pill that costs $5 to make? It’s not just America. It’s everywhere. And yet, no one does anything. I’m just... tired. 😩
Katie Magnus
23 November 2025 - 10:33 AM
Okay but have you ever tried switching to a generic and felt like a zombie? I did. For three weeks. My doctor said it was 'in my head.' My head wasn't the problem - the generic was. I'm not crazy. I'm just not a lab rat for Big Pharma's profit margins. #BrandNameOnly
King Over
23 November 2025 - 11:22 AM
generics work fine for me
paid $4 for my blood pressure med
no issues
no drama
just take the pill
Johannah Lavin
23 November 2025 - 21:57 PM
Y’ALL. I just want to hug everyone who’s fighting for affordable meds 💕
My mom took generics for her diabetes for 12 years and never missed a dose because she could afford them. That’s not luck - that’s justice. 🙏
And yes, sometimes the generic makes you feel weird - talk to your pharmacist, don’t suffer in silence. You deserve to feel like yourself, not a side effect.
Ravinder Singh
25 November 2025 - 11:30 AM
As someone from India where generics are the norm, I can tell you - they save lives. My uncle survived heart failure because he could afford clopidogrel, not Plavix. The science is solid. The FDA doesn't lie. But I get it - when you’ve been told your life depends on a brand name, it’s hard to trust anything else. Try one. If it works, great. If not, go back. But don’t let fear cost you more than the drug itself. 💪
Russ Bergeman
25 November 2025 - 20:38 PM
Wait - so you’re saying the FDA approves generics? That’s hilarious. They approve everything. Last year, 47% of drug recalls were for generics. And you think that’s fine? You’re literally gambling with your life. And don’t even get me started on the foreign factories - you have no idea what’s in those pills. 😅
Dana Oralkhan
27 November 2025 - 04:26 AM
I just want to say - if you’ve ever had to choose between your medication and groceries, you know how important this is. I used to split my pills because I couldn’t afford the brand. I didn’t feel guilty - I felt angry. But now I know I’m not alone. Thank you for saying this out loud. We need more of this conversation.
Jeremy Samuel
27 November 2025 - 22:52 PM
generics are for losers who cant afford the real thing
if you want to feel good
you gotta pay for the real deal
also i heard generics are made in china
so like... yk
its prob just sugar pills with a stamp
Destiny Annamaria
29 November 2025 - 14:50 PM
My abuela in Puerto Rico takes 7 different generics. She doesn’t speak English, but she knows the names of her pills better than I know my own birthday. She says, ‘Si funciona, no lo cambies.’ If it works, don’t change it. And guess what? It works. She’s 82 and still dancing salsa. 🕺💃 Generics aren’t a compromise - they’re a celebration of smart, simple care.