Why Clinicians Still Doubt Generic Drugs - And How to Fix It
Over 90% of prescriptions filled in the U.S. are for generic drugs. Yet, nearly 7 out of 10 doctors still worry they’re not as good as brand-name versions. That’s not just outdated thinking - it’s costing patients money, adherence, and health.
Generics aren’t cheaper because they’re lower quality. They’re cheaper because they don’t need to repeat expensive clinical trials. The FDA requires them to have the exact same active ingredient, strength, dosage form, and route of administration as the brand. And they must prove they work the same way in the body through strict bioequivalence testing: the 90% confidence interval for absorption (AUC) and peak concentration (Cmax) must fall between 80% and 125% of the brand. That’s not a guess - it’s science.
The Real Problem Isn’t the Drug - It’s the Misunderstanding
Doctors aren’t ignoring evidence. They’re confused by misinformation. A 2020 survey of over 1,200 prescribers found:
- 45% thought generics had to have identical inactive ingredients (they don’t - and that’s okay)
- 38% believed manufacturing standards were looser for generics (they’re not - same facilities, same inspections)
- 27% thought generics could contain 20-25% less active ingredient (they can’t - it’s 100% identical)
These aren’t minor gaps. They lead to real-world consequences. A patient prescribed a generic blood pressure pill might hear their doctor say, “I know this one’s cheaper, but I’m not sure…” - and suddenly, the patient starts doubting it too. Harvard research shows when providers openly endorse generics, patients are 3.2 times more likely to take them as directed.
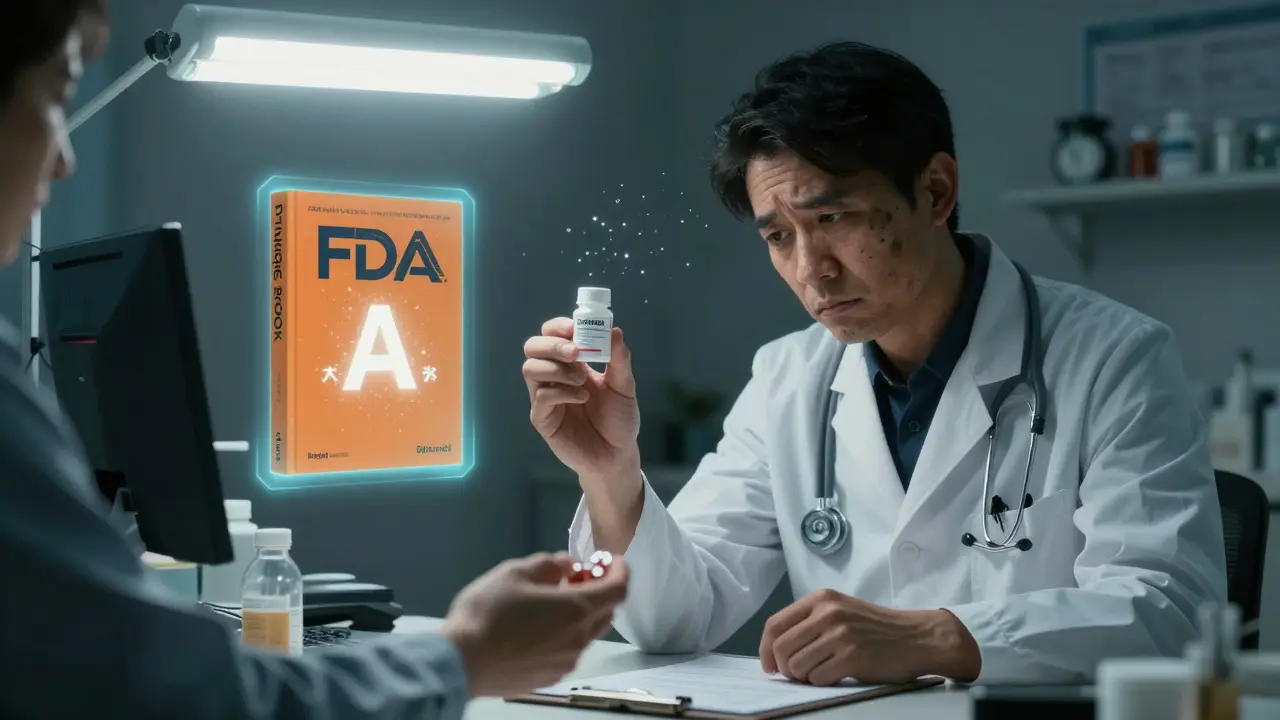
What the FDA Actually Says - And What You Need to Know
The FDA’s Orange Book is the official source for therapeutic equivalence ratings. Look for an “A” rating. That means the generic is interchangeable with the brand. A “B” rating? That’s a red flag - it means the drug isn’t considered equivalent, often because of delivery issues (like extended-release capsules). Most generics you’ll prescribe are “A” rated.
Here’s what’s non-negotiable for FDA approval:
- Same active ingredient - no exceptions
- Same strength and dosage form - tablet, capsule, injection, etc.
- Same route of administration - oral, topical, IV
- Same bioequivalence - proven through clinical testing
- Same manufacturing standards - same inspections, same quality controls
Inactive ingredients? They can differ. That’s why some generics might cause minor differences in taste or color. But they can’t change how the drug works. If they did, the FDA wouldn’t approve it.
How Education Changes Behavior - Real Data
Simply handing out pamphlets doesn’t work. A 2021 study in JAMA Internal Medicine compared two groups of doctors: one got a 10-page PDF. The other got four 90-minute interactive sessions with case studies over six months. At the six-month mark, the interactive group remembered 42% more. They also prescribed generics 29% more often.
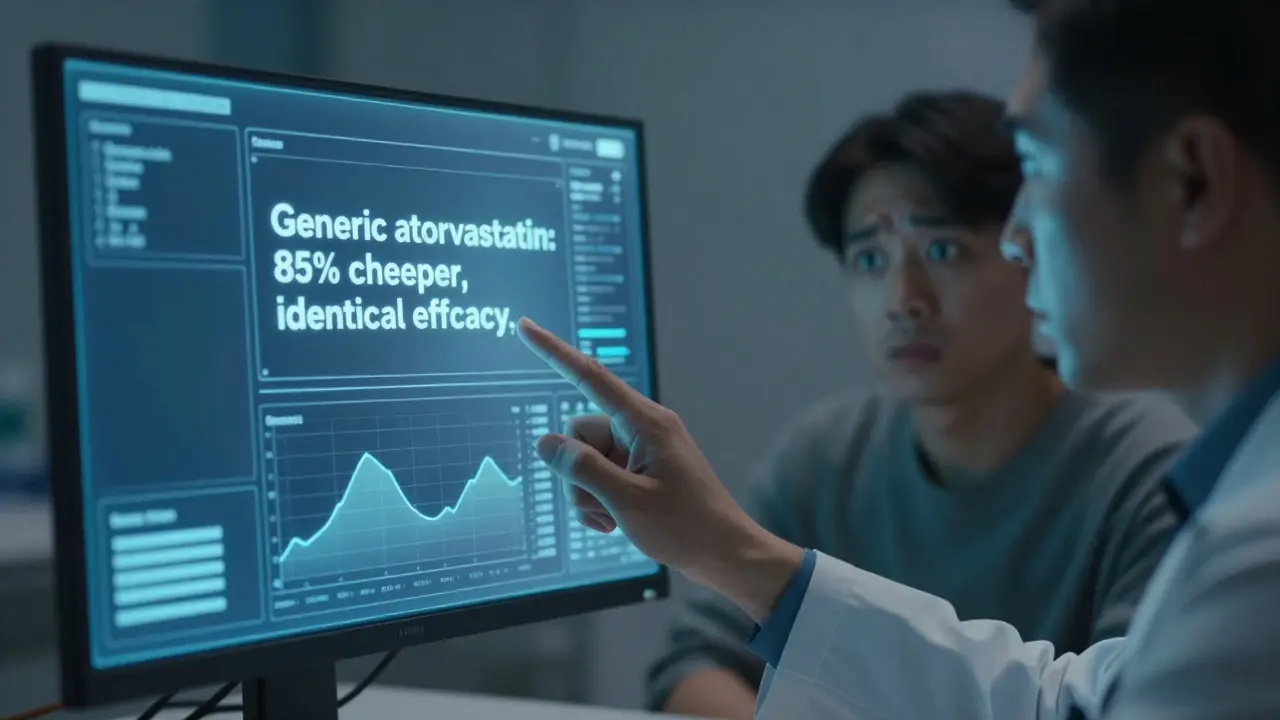
At UCSF Medical Center, they embedded educational prompts into their electronic health record system. When a doctor typed “Lipitor,” a pop-up appeared: “Generic atorvastatin is equivalent and costs 85% less. Confirm or switch?” Within a year, brand-name statin prescriptions dropped 37%.
And it’s not just about cost. In psychiatry, where nocebo effects are strong, patients prescribed generic antidepressants reported fewer side effects - only when their doctor said the generic was just as good. That’s not placebo. That’s trust.
Where Provider Education Falls Short - And Why
Not all programs work. A Tennessee Medicaid initiative spent $1.2 million on generic education in 2020. Result? Only 8% increase in generic use. Why? The materials weren’t tied to the EHR. Doctors didn’t see them when they were prescribing. They were buried in a portal.
Time is another barrier. Eighty-nine percent of physicians say they don’t have time to learn more about generics during the workday. But here’s the twist: spending five minutes explaining why a generic is safe saves hours later dealing with non-adherence, hospitalizations, or refill calls.
Some specialties resist more than others. Neurologists and cardiologists are the most skeptical - 79% and 82% respectively say they hesitate to prescribe generics. Why? Complex conditions. But data shows generics work just as well for epilepsy, hypertension, and heart failure. The issue isn’t the drug - it’s the fear.
What You Can Do Tomorrow - Practical Steps
You don’t need a 10-hour course. Start here:
- Visit the FDA’s Generic Drug Stakeholder Toolkit. Download the prescriber flyer - it’s free, under 2 pages, and has real data.
- Use the Orange Book. Type in the brand name. Check the therapeutic equivalence code. If it’s “A,” you’re good to go.
- When prescribing, say: “This generic is identical to the brand. It’s been tested to work the same way. It’s safe, effective, and will save you money.”
- Ask your pharmacy: “Can you substitute?” If they say no, ask why. Often, it’s not a medical reason.
- Use EHR alerts. If your system doesn’t have them, ask your IT team to add a prompt for high-cost brand drugs.
For ongoing learning, look for CME credits on generic drugs. A 2022 poll of 4,200 physicians showed 63% want more. Internal medicine specialists - who prescribe the most generics - were the most eager.
Biosimilars Are Not Generics - Don’t Confuse Them
Here’s a big one: generics and biosimilars are not the same. Generics are copies of small-molecule drugs - pills you swallow. Biosimilars are copies of large, complex biologic drugs - injections like Humira or Enbrel. They’re not exact copies. They’re “similar enough.”
Only 31% of providers can correctly explain the difference. That’s a problem. If you’re prescribing a biosimilar for rheumatoid arthritis, you need to know it’s not a generic. But you also need to know it’s proven safe and effective. The FDA has a separate approval process for biosimilars - and they’re still cheaper than the brand.
The Bigger Picture: Cost, Adherence, and Outcomes
Over the past decade, generics saved the U.S. healthcare system $2.2 trillion. That’s not a number - it’s millions of patients who could afford their meds. Patients on generics are 35% more likely to start their treatment and stick with it.
By 2025, Medicare’s MIPS program will start measuring how often you prescribe generics. It’ll be a quality metric. The message is clear: prescribing generics isn’t just smart - it’s becoming required.
Final Thought: Your Word Matters More Than You Think
Patients don’t care about FDA regulations. They care about what their doctor says. If you say, “This is just as good,” they believe you. If you say, “I’m not sure,” they don’t take it. Your confidence isn’t just about knowledge - it’s a treatment tool.
Start small. Pick one high-cost brand you prescribe often. Switch to the generic. Explain why. See what happens. You might be surprised - your patients will be.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also prove bioequivalence - meaning they work the same way in the body. Studies show no meaningful difference in effectiveness for over 90% of generic drugs. The only exceptions are a few complex formulations, which the FDA flags with a “B” rating in the Orange Book.
Why do some doctors refuse to prescribe generics?
Many doctors have outdated beliefs - like thinking generics have lower quality or different ingredients. Others worry about patient reactions or recall anecdotal stories. But data shows these concerns are rarely based on evidence. A 2017 study found 68% of physicians had doubts, even though generics meet the same standards. Education and direct experience with patient outcomes reduce these fears.
Can pharmacists substitute generics without the doctor’s permission?
It depends on the state. Thirty-four states allow pharmacists to substitute a generic for a brand without telling the doctor, as long as the drug is rated “A” by the FDA. Sixteen states require the prescriber to write “dispense as written” to block substitution. Always check your state’s law - but know that substitution is legal and safe in most places.
Do generics have more side effects than brand-name drugs?
No. The active ingredient - the part that causes therapeutic effects - is identical. Inactive ingredients (fillers, dyes) can differ, but they’re chosen to be safe and non-interfering. Some patients report side effects after switching, but research shows this is often a nocebo effect - anxiety about the change, not the drug itself. When doctors confidently endorse generics, patient-reported side effects drop by up to 18%.
How can I learn more about generics without spending hours?
Start with the FDA’s free Generic Drug Facts Handout - it’s a two-page PDF with key facts. Then use the Orange Book online to check ratings for drugs you prescribe. For ongoing learning, look for 1-hour CME modules on generic drugs - many are free and count toward your requirements. You don’t need a deep dive. Just enough to speak confidently to patients.
Is there a risk in switching a patient from brand to generic?
For most drugs, no. For stable patients on chronic meds like blood pressure or antidepressants, switching to a generic is safe and often improves adherence. The only exceptions are drugs with narrow therapeutic windows - like warfarin or levothyroxine - where small changes in absorption matter. Even then, studies show generics work fine for most patients. Monitor blood levels if you’re concerned, but don’t assume the generic is the problem.
What Comes Next: AI, EHRs, and the Future of Prescribing
The next wave of change isn’t just education - it’s integration. Health systems are now using AI to flag high-cost brand prescriptions and suggest generics right at the point of care. UnitedHealthcare’s 2024 pilot program targets doctors who rarely prescribe generics and sends them personalized videos and data - and it boosted generic use by 28%.
Virtual reality training is also emerging. The FDA’s new VR module lets doctors practice talking to patients about generics in simulated office visits. Early results show a 41% increase in provider confidence.
By 2026, if you’re not using EHR prompts, CME modules, or patient handouts on generics, you’re falling behind. The system is changing. The data is clear. The savings are real. And your patients are waiting for you to lead the way.


Bradford Beardall
9 January 2026 - 19:14 PM
I've been prescribing generics for years and my patients save hundreds a year. The real issue isn't the drug-it's the fear we unconsciously transmit. When I say 'this is the same thing' with confidence, adherence jumps. Simple as that.
McCarthy Halverson
11 January 2026 - 11:08 AM
FDA standards are non-negotiable. Same active ingredient. Same bioequivalence. Same inspections. If you're still hesitant you're not being evidence-based you're being lazy.
Michael Marchio
12 January 2026 - 20:08 PM
Let's be real here. The pharmaceutical industry doesn't want you to know this but generics are the only reason most people can afford their meds. The brand names are overpriced because they're not competing. The FDA doesn't care about your comfort zone. It cares about science. And science says generics work. Period. If you're still worried you're part of the problem not the solution.
Jake Kelly
14 January 2026 - 11:51 AM
I appreciate this breakdown. Especially the part about EHR prompts. My clinic just added one for statins and we've seen a real drop in brand prescriptions. Small changes make big differences.
Ashlee Montgomery
14 January 2026 - 17:05 PM
The nocebo effect is real and terrifying. Patients believe what they hear. If you say 'I'm not sure' they'll feel worse even if the drug is identical. Your words are medicine too.
neeraj maor
16 January 2026 - 16:42 PM
You think this is about science? Wake up. The FDA is controlled by Big Pharma. They approve generics only after the brand patent expires so they can keep profiting. The 'bioequivalence' testing is a joke. How do you know they didn't manipulate the data? I've seen patients crash after switching. No one talks about it because the system is rigged.
Ritwik Bose
18 January 2026 - 09:17 AM
Thank you for this comprehensive overview. As a physician from India I can confirm that generic access has transformed chronic disease management in low-resource settings. The science is clear. The ethical imperative is even clearer. 🙏
Paul Bear
19 January 2026 - 07:17 AM
It's important to distinguish between therapeutic equivalence and interchangeability. While most generics are rated 'A' by the FDA, pharmacists in some states are legally permitted to substitute without prescriber consent. This creates a liability exposure if the patient experiences an adverse reaction due to excipient variation. You must document your intent clearly in the EHR to mitigate risk. Also, bioequivalence thresholds of 80-125% are statistically valid but clinically heterogeneous in narrow-therapeutic-index drugs. You're not accounting for pharmacokinetic variability across populations.
lisa Bajram
20 January 2026 - 14:32 PM
OMG YES. I switched my mom from brand-name Lipitor to atorvastatin and she was terrified. I showed her the FDA page, told her it was the exact same molecule, and she cried because she finally felt safe taking it. Generics aren't cheap-they're justice. And we're the ones who get to hand that out. 💪
Jaqueline santos bau
21 January 2026 - 12:34 PM
I had a patient who switched to a generic antidepressant and said she felt 'numb' and 'empty'-like her soul was gone. She blamed the generic. But when I asked her what she thought the brand was doing for her? She said 'it made me feel like myself.' So I switched her back. And guess what? She still felt the same. It wasn't the drug. It was the story she told herself. We're not just prescribing pills. We're prescribing hope. And if you undermine that with hesitation? You're the one hurting them.
Kunal Majumder
22 January 2026 - 04:45 AM
In India we use generics daily. No one has time for brand names. But the quality? Spot on. My uncle takes generic metformin for 15 years. Still alive. Still working. Still managing. The system works if you let it.
Aurora Memo
22 January 2026 - 15:42 PM
This is exactly the kind of clarity our field needs. Not more fear. Not more jargon. Just facts. And a reminder that our confidence matters more than we realize. Thank you for writing this.
Christine Milne
23 January 2026 - 12:03 PM
While your assertions are technically correct under FDA guidelines, you completely omit the documented cases of bioequivalence failure in extended-release formulations, particularly those with complex polymer matrices. The 80-125% AUC range is statistically permissible but clinically inadequate for patients with altered GI motility, renal impairment, or polypharmacy. Furthermore, the FDA's Orange Book does not reflect post-marketing surveillance data on adverse event clustering. To suggest that generics are universally interchangeable is not merely misleading-it is dangerously oversimplified. As a board-certified pharmacologist with 28 years of clinical experience, I urge you to reconsider the ethical implications of promoting this narrative without contextual nuance.