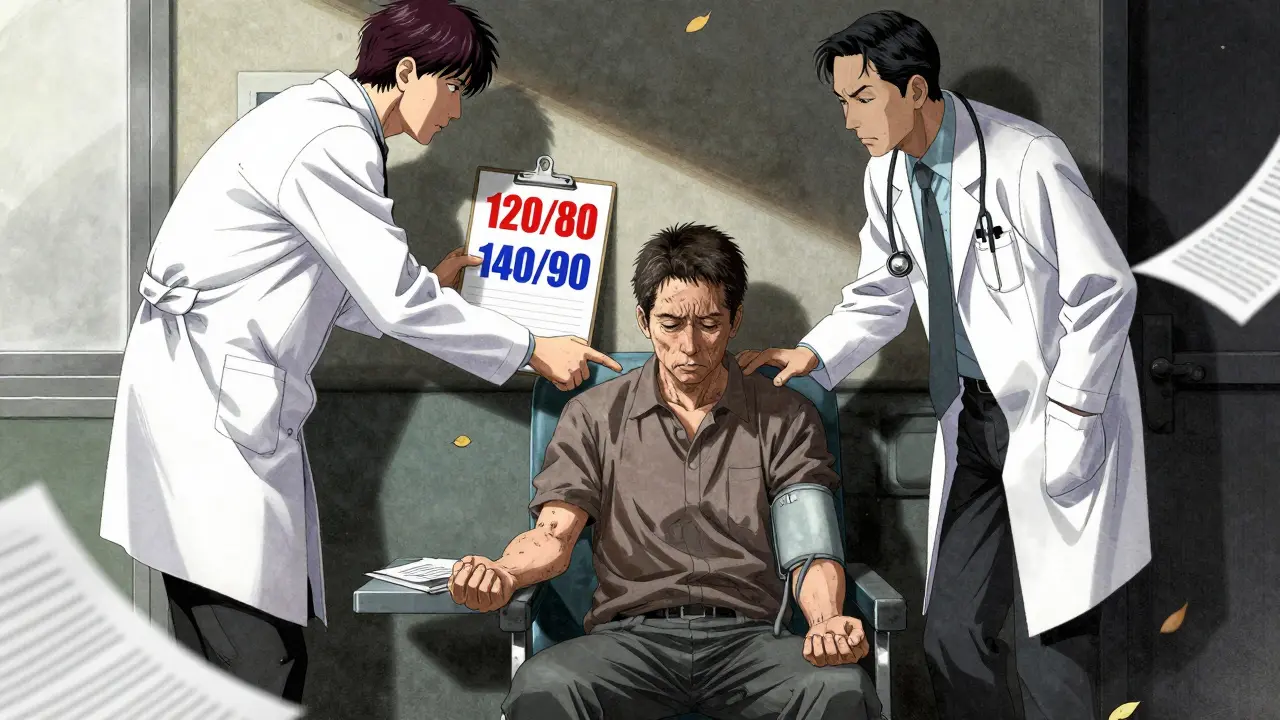
For years, doctors have told people to keep their blood pressure below 120/80 mm Hg - the so-called "ideal" number. But if you’ve been told that lately, you might be confused. Some doctors still say 140/90 is fine. Others push hard for 130/80. And some say it depends on you. So what’s really going on? Why do guidelines keep changing? And which one should you trust?
Why 120/80 Became the Gold Standard
The push for 120/80 didn’t come out of nowhere. It came from the SPRINT trial, a major study published in 2015 that followed over 9,000 adults with high blood pressure. Half were told to get their systolic pressure below 140. The other half were pushed to get it below 120. After about four years, the group with the lower target had 25% fewer heart attacks, strokes, and heart failure cases. Their risk of dying from any cause dropped by 27%. That was huge. It changed everything. By 2017, the American Heart Association and American College of Cardiology updated their guidelines to say: if your blood pressure is 130/80 or higher, you have hypertension. No more "pre-hypertension." Just hypertension. And the goal? Below 130, ideally below 120. That’s where we stand today for most major U.S. heart groups. But here’s the catch: SPRINT wasn’t your typical patient. Participants were carefully selected. They didn’t have diabetes. They weren’t over 75 with a history of falls. They weren’t on multiple medications already. They were healthy enough to handle aggressive treatment. That’s why some doctors - especially those seeing everyday patients - aren’t convinced 120/80 should be the universal target.The Other Side: Why 140/90 Still Makes Sense
The American Academy of Family Physicians (AAFP) took a different look at the same data. They didn’t ignore SPRINT. They asked: "What does this mean for someone who’s 72, has arthritis, takes five pills a day, and already gets dizzy standing up?" Their 2022 review found that lowering systolic pressure from 140 to 120 gave only a tiny extra benefit - reducing heart attacks by about 1 in 137 people over nearly four years. But it came with a cost: one in 33 people had serious side effects like fainting, kidney problems, or dangerously low blood pressure. That’s not a small trade-off. They concluded: for most people, especially older adults or those with multiple health issues, 140/90 is just as safe and just as effective at preventing death. And it means fewer pills, fewer doctor visits, and less risk of falling or getting sick from medication. It’s not that they’re against lower numbers. It’s that they’re against one-size-fits-all. If you’re 45, active, and otherwise healthy? Sure, aim for 120. But if you’re 80, live alone, and have trouble walking? Maybe 130-140 is the right balance.What the Rest of the World Is Doing
The U.S. isn’t alone in this debate. Japan’s 2025 guidelines went further than any major country: everyone with high blood pressure - no matter their age, diabetes, or fall risk - should aim for below 130/80. Their reasoning? A massive global analysis showed that for every 5 mm Hg drop in systolic pressure, the risk of heart attack or stroke drops by 10%. That held true even in people over 80. But here’s the key: Japan’s system is built for it. Almost everyone has access to frequent checkups. Home blood pressure monitors are standard. Pharmacies are everywhere. If your pressure drops too low, you’re seen within hours. In the U.S., where many people wait weeks for a doctor’s appointment, that’s not realistic. Europe takes a middle path. The European Society of Hypertension says:- Under 65: aim for 120-129/70-79
- 65-79: aim for 130-139
- 80+: aim for 140-150

Who Should Aim for 120/80?
If you’re under 65 and have any of these, you’re likely a good candidate for the lower target:- Diabetes
- Chronic kidney disease
- History of heart attack or stroke
- 10-year heart disease risk of 7.5% or higher (calculated using the PREVENT tool)
- Already on two or more blood pressure medications
What About Lifestyle? It’s Still the First Step
No matter which target you’re aiming for, lifestyle changes are non-negotiable. Medication helps - but it doesn’t replace diet, movement, and sleep.- Reduce sodium to under 2,300 mg a day (ideally 1,500)
- Get 150 minutes of walking or cycling per week
- Limit alcohol to one drink a day for women, two for men
- Manage stress - meditation, deep breathing, even gardening helps
- Get 7-8 hours of sleep. Poor sleep raises blood pressure.

The Real Issue: Monitoring and Safety
The biggest problem with pushing for 120/80 isn’t the goal. It’s the follow-up. If you’re on aggressive treatment, you need to check your pressure regularly - not just at the doctor’s office. Home monitoring is essential. Many people don’t realize their pressure drops too low after taking meds, especially in the morning or after standing up. Symptoms like dizziness, blurred vision, confusion, or fainting aren’t "just aging." They’re red flags. If you feel this way, tell your doctor. Your target might need to rise - even if it’s "supposed" to be 120. The Japanese guidelines stress careful monitoring. That’s smart. But in the U.S., where most people see their doctor once a year, that’s not enough. You need to be your own advocate.What Should You Do?
Don’t pick a number based on a headline. Pick a plan based on your life. Ask your doctor:- What’s my 10-year heart risk? (Ask for the PREVENT calculator)
- Am I at risk for falls or dizziness from meds?
- How many pills am I on now? Can we avoid adding more?
- Can we start with lifestyle changes before adding drugs?
- What symptoms should I watch for?
What’s Coming Next?
The NIH just launched SPRINT-2 - a new trial with over 8,000 people, including those with diabetes and higher fall risk. This will show whether the 120/80 target works for real-world patients, not just the healthy ones in the original study. Meanwhile, tools are emerging that use AI to predict how you’ll respond to different drugs based on your genes, diet, and lifestyle. In the next five years, your blood pressure target might be customized not just by age or disease - but by your unique biology. For now, the best advice is simple: know your number. Talk to your doctor. Don’t let fear of "high" numbers push you into a treatment that hurts more than it helps.High blood pressure is serious. But so are the side effects of trying to fix it too hard.
Is 120/80 blood pressure too low for older adults?
For many older adults - especially those over 75 - 120/80 can be too low. It increases the risk of dizziness, falls, kidney problems, and fainting. The goal for this group is often 130-140 systolic, as long as they feel well and aren’t having symptoms. Lower isn’t always better if it means losing independence.
Why do different doctors give different blood pressure targets?
Because they follow different guidelines. Cardiologists often follow the AHA/ACC, which recommends 130/80 or lower. Family doctors often follow the AAFP, which says 140/90 is safer for most people. The difference comes down to who they treat: specialists see higher-risk patients; primary care sees the full population.
Can I lower my blood pressure without medication?
Yes - and it’s the first step for everyone. Losing 10 pounds, cutting salt, walking 30 minutes a day, and sleeping well can drop systolic pressure by 5-10 mm Hg. For some, that’s enough to avoid meds entirely. Even if you take pills, lifestyle changes make them work better and reduce side effects.
Should I buy a home blood pressure monitor?
Yes - especially if you’re on treatment. Office readings can be misleading due to "white coat hypertension." Home monitoring gives a clearer picture. Look for an upper-arm, automated cuff with validation from the American Heart Association. Write down readings and bring them to your appointments.
What if I feel fine but my blood pressure is high?
High blood pressure often has no symptoms - that’s why it’s called the "silent killer." Feeling fine doesn’t mean your heart and arteries aren’t being damaged. Even if you feel great, untreated high pressure raises your risk of stroke, heart failure, and kidney disease over time. Treatment isn’t about how you feel - it’s about protecting your future health.


Kinnaird Lynsey
18 December 2025 - 00:56 AM
Wow, finally someone wrote this without sounding like a pharmaceutical ad. I’m 72, take three meds, and my BP drops to 98/60 if I so much as stand up too fast. My doctor just shrugged and said, 'You’re fine.' I’m not fine-I’m dizzy-but at least I’m not in the ER.
Glen Arreglo
19 December 2025 - 14:47 PM
Look, the SPRINT trial was great-but it was a lab experiment with healthy people. Real life isn’t a clinical trial. I’m a family doc in rural Ohio. My patients are working two jobs, skipping meds because they can’t afford them, and their BP is 145/92. Should I push them to 120? Or should I help them eat better and get some sleep? The latter actually works.
shivam seo
20 December 2025 - 16:07 PM
US guidelines are a joke. We’re so obsessed with ‘targets’ we forget people are humans. Japan’s got it right-lower is better, period. If you’re too old or frail to handle 120/80, maybe you shouldn’t be alive. That’s just biology. Stop coddling seniors with sugar-coated medicine. My grandpa died at 82 because his doc was too scared to treat his BP. He’d still be here if they’d just pushed harder.
benchidelle rivera
22 December 2025 - 15:36 PM
There is no one-size-fits-all approach to hypertension. This is not a math problem. It is a human problem. I have worked with elderly patients who, after being aggressively treated to 120/80, fell, fractured their hip, and never recovered. The goal is not to hit a number-it is to preserve function, autonomy, and dignity. Medication is a tool, not a trophy.
Connie Zehner
24 December 2025 - 12:45 PM
Okay but have you heard about the BIG LIE? The pharmaceutical companies paid off the AHA to push 120/80 so they could sell MORE pills. I know a nurse who said they get bonuses for pushing patients to more meds. My uncle’s BP was 135/85 and they put him on FOUR drugs. He started passing out in the shower. Then they blamed it on ‘aging.’ I’m telling you-this is all a scam. Wake up people!! 🤡💊
Vicki Belcher
26 December 2025 - 12:33 PM
YES YES YES. I’m 58, active, no meds, and my BP is 118/76. I eat clean, walk daily, and sleep like a log. But my mom, 81, has 138/82 and feels great. She doesn’t need more pills. She needs more hugs and less pressure (literally 😊). The goal isn’t perfection-it’s peace. Your body knows what it needs. Listen to it.
Alex Curran
28 December 2025 - 01:58 AM
Home monitors are non negotiable. I got mine after my doc said I was fine but I kept feeling faint. Turns out my BP was 102/60 after my morning pill. I stopped taking it for a day and wrote down readings. Took it to my doc. They lowered the dose. No drama. Just data. Everyone should do this. It’s free and saves lives.
Lynsey Tyson
28 December 2025 - 05:06 AM
I think the real issue is that doctors don’t have time to talk about this stuff. I had a 7-minute appointment where they just handed me a script for a new pill. No questions asked. No ‘how do you feel?’ Just ‘take this.’ I get why guidelines get messy-because the system is broken.
Edington Renwick
30 December 2025 - 04:22 AM
They’re all wrong. The truth is, blood pressure is a scam. The whole medical industry is built on fear. You don’t need to ‘control’ your BP. You need to stop eating processed food, get off the couch, and stop stressing about numbers. The body heals itself if you just let it. I’ve been off meds for 5 years. My BP is 122/78. No pills. No fear. Just freedom.
Laura Hamill
30 December 2025 - 08:32 AM
They’re hiding the truth. The FDA and Big Pharma are in bed together. That SPRINT trial? It was funded by Merck. They wanted more pills sold. That’s why they picked only healthy people. Real people? They get dizzy. They fall. They die. And they blame it on ‘old age.’ But I know the truth. They don’t want you to know that you can live fine with 140/90. They want you dependent. Wake up. 🚨🩸