Every year, over 1.3 million people in the U.S. are injured because of medication errors - and many of those happen right at the pharmacy counter. You pick up your prescription, glance at the label, and walk out. But what if the pill bottle has the wrong name? Or the dosage is off by half? Or the drug interaction wasn’t checked? These aren’t rare mistakes. They’re preventable - and you have more power to stop them than you think.
Why Your Pharmacy Visit Needs a Checklist
Pharmacists are trained professionals. They work hard. But they’re also juggling 20+ prescriptions an hour, dealing with insurance delays, and managing automated systems that sometimes glitch. Even the best pharmacies make mistakes. A 2023 study found that one in every 15 prescriptions filled in community pharmacies had at least one error - from wrong dosage to wrong patient name. You can’t control the pharmacy’s workload. But you can control what happens when you walk up to the counter. A simple personal safety checklist turns you from a passive recipient into an active safety partner. It’s not about doubting your pharmacist. It’s about adding a layer of protection that even the best systems miss.Step 1: Bring Your Complete Medication List
Before you even leave the house, make a list. Not just what you’re picking up today - everything. Include:- All prescription drugs (name, dose, frequency)
- All over-the-counter meds (ibuprofen, antacids, sleep aids)
- Vitamins, supplements, and herbal products (even if you think they’re "harmless")
- Any recent changes - new prescriptions, stopped meds, dosage tweaks
Step 2: Verify the Prescription Before You Leave
When the pharmacist hands you the bottle, don’t just take it. Stop. Look. Ask.- Check the name on the label - Is it yours? Not your spouse’s? Not your neighbor’s?
- Compare the drug name - Does it match what your doctor told you? If your doctor prescribed "Metformin 500 mg," but the bottle says "Metformin 1000 mg," speak up.
- Confirm the dosage - "Take one pill twice a day" - is that what’s written? Many errors happen because of confusing abbreviations like "BID" or "QD." Ask them to say it in plain English.
- Check the quantity - If you were supposed to get 30 pills, but you got 60, that’s a problem. Too many can lead to accidental overdose.
Step 3: Ask About New Medications
If it’s a drug you’ve never taken before, don’t walk away without asking three questions:- "What is this for?" - Make sure it matches why your doctor prescribed it.
- "What are the side effects I should watch for?" - Some side effects are normal. Others mean you need to call your doctor immediately.
- "Can this interact with anything else I’m taking?" - Especially if you’re on blood pressure meds, diabetes drugs, or blood thinners. Even grapefruit juice can be dangerous with some prescriptions.

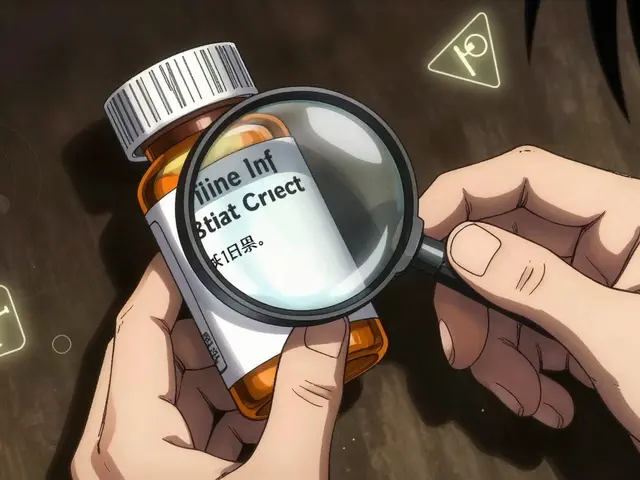
Step 4: Check the Pill Appearance
Many people don’t realize that pills change shape, color, or size depending on the manufacturer. That doesn’t mean it’s wrong - but it can be confusing.- Compare the new pills to your last refill. Are they the same shape, color, and imprint code? (The letters/numbers on the pill.)
- If they look different, ask: "Is this the same medication I got last time?"
- Use the National Library of Medicine’s Pill Identifier tool (on your phone) to search by imprint, shape, or color. If the pharmacy’s pill doesn’t match the official image, question it.
Step 5: Confirm the Instructions
Read the label. Then ask the pharmacist to repeat the instructions out loud.- Is it "take with food" or "take on an empty stomach"?
- Do you take it in the morning or at night?
- Is it okay to crush or split the pill?
Step 6: Take a Photo of the Label
This is the step most people skip - and it’s the easiest to forget. Before you leave the pharmacy, take a clear photo of the prescription label. Include:- The patient name
- The drug name and dose
- The quantity
- The directions
- The pharmacy name and phone number
Step 7: Report Suspicious Errors
If you catch a mistake - even a small one - report it. Not to complain. To protect others.- Ask to speak with the pharmacist-in-charge.
- Say: "I noticed this error. I’d like to report it so it doesn’t happen to someone else."
- Write down the date, time, drug name, and what went wrong.

What to Do If You’ve Already Taken the Wrong Medication
If you realize you took the wrong pill - even just one - don’t panic. But act fast.- Call your pharmacist immediately. They know the drug and can tell you if it’s dangerous.
- If you feel sick, dizzy, or have chest pain, call 911 or go to the ER.
- Keep the pill bottle and the wrong pill. Bring it with you.
- Don’t take another dose until you’ve talked to a professional.
Real Example: How a Checklist Saved a Woman’s Life
In 2023, a 68-year-old woman in Austin picked up a new blood thinner. The label said "Warfarin 5 mg." She’d been on 2 mg for years. The pharmacist had accidentally filled the wrong bottle. She noticed the pill looked different - bigger, paler. She pulled out her phone, checked her photo of last month’s bottle, and asked for a review. The pharmacist found the error: another patient’s prescription had been swapped. If she hadn’t checked, she could have suffered a brain bleed within days. She didn’t know she was "supposed" to do this. She just trusted her gut - and had the habit of comparing labels.Final Tip: Make It a Habit
You don’t need to memorize a 10-step checklist. Just remember this: Stop. Look. Ask. - Stop before you walk away. - Look at the label, the pill, your list. - Ask one question if anything feels off. Do this every single time - even if you’ve been going to the same pharmacy for 10 years. Systems fail. People get tired. But your eyes? Your memory? Your voice? Those never fail you.Do pharmacists always catch their own mistakes?
No. Even the best pharmacies have error rates. A 2023 study found that 6% of prescriptions filled had errors - and many of those were caught only because the patient noticed something wrong. Pharmacists rely on double-checks, but those aren’t foolproof. Your involvement adds a critical layer of safety.
Can I ask for a printed copy of the prescription details?
Yes. You have the right to request a printed copy of your prescription label, dosage instructions, and any counseling notes. Most pharmacies will provide it. If they say no, ask to speak to the manager. This is part of your right to informed consent.
What if the pharmacy refuses to check my medication?
If a pharmacist dismisses your concerns or refuses to verify your prescription, leave. Take your business elsewhere. Your safety matters more than convenience. You can also report the incident to your state’s Board of Pharmacy - they investigate complaints about dispensing errors.
Are generic drugs less safe than brand names?
No. Generic drugs are required by the FDA to have the same active ingredient, strength, and effectiveness as brand-name drugs. The only differences are in inactive ingredients (like fillers) or appearance. But if the pill looks drastically different from your last refill, still ask - it could be a different generic manufacturer, or a mistake.
Should I use a pill organizer?
Yes - but only after you’ve verified the right pills are going in. A pill organizer helps you take the right dose at the right time. But if you put the wrong pill in, it becomes a danger. Always double-check each pill against your list or photo before loading it into the organizer.


Chloe Hadland
23 January 2026 - 10:49 AM
I started doing the photo thing after my grandma almost got the wrong blood pressure med. Best habit ever. Just snap it, save it, forget it until you need it. Easy.
Seriously, why do we wait until something goes wrong to care?
Michael Camilleri
25 January 2026 - 05:50 AM
People think safety is about checklists but its really about accountability. The system is broken because we outsource our responsibility to people who are overworked and underpaid. You want safety? Stop treating pharmacists like robots and start treating yourself like the adult who's supposed to be in charge of their own body.
This isn't a guide. Its a wake up call.
lorraine england
26 January 2026 - 20:22 PM
I love that you included the pill appearance check. My mom took a new med last year and thought it was the same because the bottle looked familiar. Turned out it was a different generic. She got dizzy for three days. Now we always compare pills.
Also taking photos? Genius. I keep mine in a folder called "Don't Die Because I Was Lazy" lol.
Himanshu Singh
27 January 2026 - 08:47 AM
You know what's wild? Most people don't even know what their meds are for. I coach my elderly neighbors to say "why am I taking this?" out loud when they pick it up. It forces them to engage.
And if they say "the doctor said so"? That's not an answer. That's a red flag.
You're not just a patient. You're the CEO of your own health. 😊
Izzy Hadala
27 January 2026 - 22:47 PM
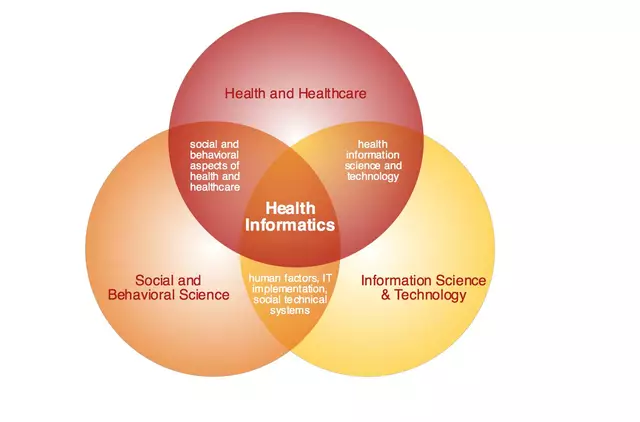
The empirical data cited in this post is statistically significant and aligns with CDC pharmacovigilance reports from Q3 2023. The 6.7% error rate in community pharmacy dispensing is corroborated by the National Association of Boards of Pharmacy. However, the proposed checklist methodology lacks standardization and may introduce cognitive load bias. A structured, digital verification protocol integrated with EHR systems would be more scalable.
blackbelt security
29 January 2026 - 07:42 AM
This isn't just advice. This is survival training. You think your pharmacist has time to babysit your meds? They're running on fumes.
If you don't verify, you're gambling with your life. And you don't get a second chance.
Do the checklist. Every. Single. Time.
Patrick Gornik
30 January 2026 - 11:54 AM
The entire premise is a neoliberal fantasy. You're supposed to be a safety net for a system that deliberately underfunds healthcare workers? That's not empowerment. That's exploitation dressed up as self-help.
The real solution? Universal healthcare with capped workloads and mandatory double-checks. Not you taking photos of your pill bottles while the system burns.
But hey, keep your checklist. It makes you feel like you're doing something. Meanwhile, the real problem? Corporate greed.
Karen Conlin
31 January 2026 - 07:52 AM
I teach this to my senior yoga class every month. One woman said she didn't think she "had the right" to ask questions. I told her: you have the right to live.
We make flashcards now. One card per step. Keep 'em in your wallet.
And yes, I've caught three errors in six months. One was a 10x overdose. The pharmacist cried. So did I. We're all just trying to get through this.
asa MNG
1 February 2026 - 13:08 PM
omg i did this last week and my med was totally wrong like the pill was orange and last time it was blue and i was like wait a sec and i called and they were like oh crap sorry its for someone else lmao
i almost took it and now i have a photo folder called "dont be an idiot" lol
Amelia Williams
3 February 2026 - 08:00 AM
I used to think I was being annoying asking questions. Then my dad had a stroke because he took the wrong blood thinner. He’s fine now but we had to relearn how to talk.
Now I do the checklist. Every. Single. Time. Even for my vitamins.
It’s not paranoia. It’s love. For yourself.
Sharon Biggins
4 February 2026 - 04:17 AM
i always forget the photo thing but i do the look and ask. even if i’ve been going to the same pharmacy for 15 years. last month they gave me the wrong dose and i said "this looks different" and they fixed it.
you don’t have to be loud. just be steady.
Kevin Waters
4 February 2026 - 17:11 PM
I'm a pharmacist. I see this every day. Most of us want to help. We just get slammed.
When a patient brings a list and asks a question? It makes our job easier. And safer.
Thank you for doing this. We notice. We appreciate it.
Kat Peterson
6 February 2026 - 12:38 PM
I'm crying. Not because it's sad. Because it's so simple and no one talks about it.
I used to be the girl who just grabbed the bottle and left. Then my aunt died from a drug interaction no one checked.
Now I have a ritual. I take a breath. I check the label. I ask one question.
And I never, ever walk away without it. 💔💊