Why So Many Pills Are Dangerous for Older Adults
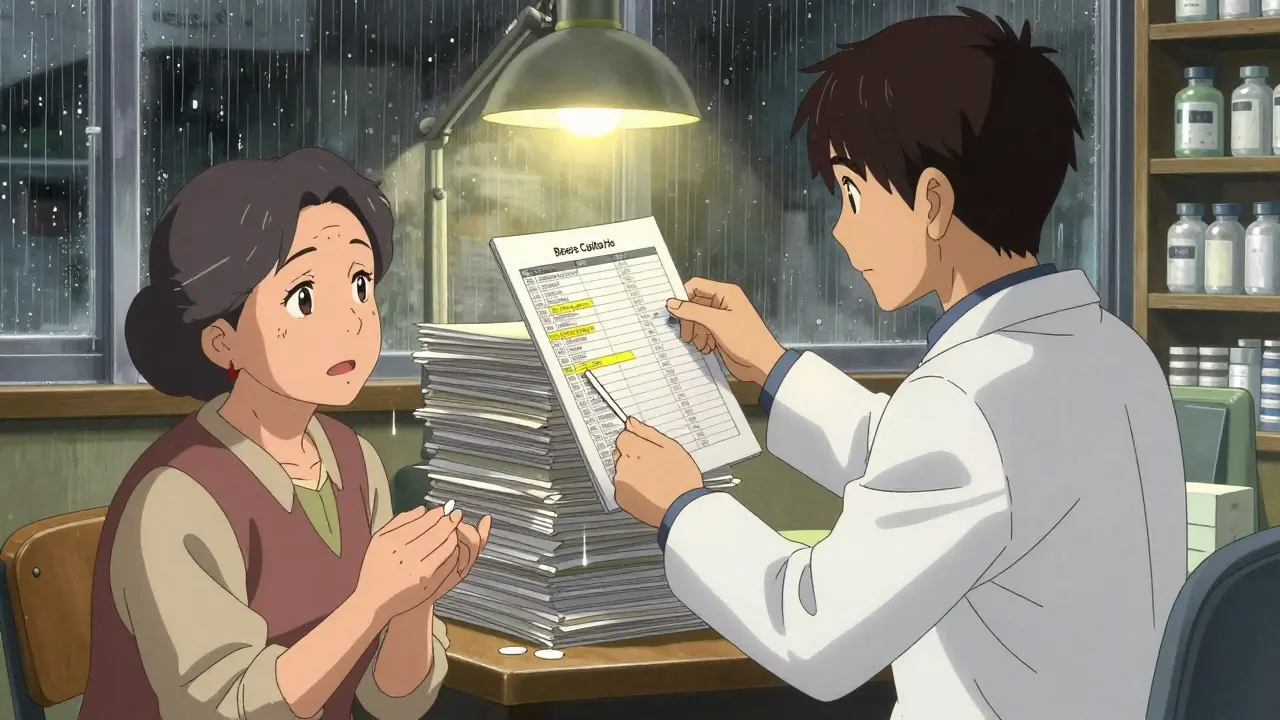
Imagine taking 10 different pills every day. Some for blood pressure, others for arthritis, a few for sleep, maybe one for acid reflux, and another for cholesterol. Sounds like a routine? For nearly half of adults over 65 in the U.S., it is. This isn’t just common-it’s risky. When someone takes five or more medications at once, it’s called polypharmacy. And while each drug might be prescribed for a real condition, together they can create a hidden storm of side effects, interactions, and confusion.
The problem isn’t that doctors are careless. It’s that medicine has become fragmented. A cardiologist prescribes one thing. A rheumatologist prescribes another. A psychiatrist adds a third. No one sees the full picture. And when you add in over-the-counter painkillers, herbal supplements, and as-needed sleep aids, the list grows even longer. Studies show that 44% of older Americans take five or more medications. For those in nursing homes? That number jumps to 80%. And the trend is still rising.
How Drug Interactions Turn Safe Meds Into Hazards
Each extra pill doesn’t just add another benefit-it multiplies the risk. With two medications, the chance of a harmful interaction is about 6%. With five, it’s 50%. With seven or more? It’s nearly certain. Why? Because aging changes how your body handles drugs.
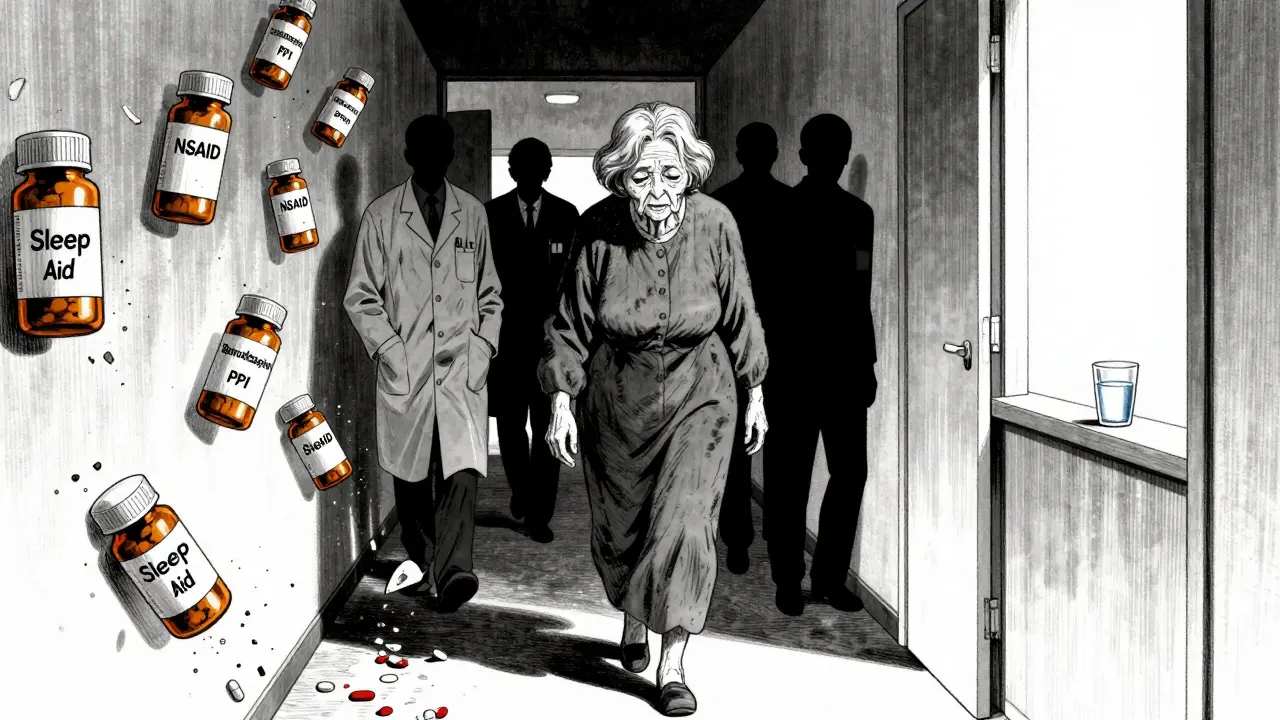
Your kidneys and liver don’t clear medications as quickly as they used to. That means drugs stick around longer, building up to dangerous levels. Your brain also becomes more sensitive to certain drugs-especially sedatives, anticholinergics, and painkillers. A common example: an older adult takes a sleep aid for insomnia. It causes dizziness. The doctor then prescribes a blood pressure pill to treat the dizziness. But the real problem? The sleep aid. This is called a prescribing cascade: one drug causes a side effect, and another drug is added to fix it-making the problem worse.
Some combinations are especially dangerous. Taking an NSAID (like ibuprofen) with blood thinners can cause internal bleeding. Mixing benzodiazepines (like Xanax) with opioids increases the risk of respiratory failure. Even common antihistamines, often used for allergies or sleep, can cause confusion, urinary retention, and falls in older adults. The American Geriatrics Society Beers Criteria® lists dozens of medications that should be avoided or used with extreme caution in people over 65. Yet many are still prescribed routinely.
Deprescribing Isn’t Stopping Meds-It’s Smart Medicine
Deprescribing doesn’t mean quitting pills cold turkey. It’s the careful, step-by-step process of removing medications that no longer help-or that do more harm than good. Think of it like decluttering your medicine cabinet. Not every pill you’ve taken for years is still necessary.
Some medications lose their value over time. Take statins, for example. If you’re 85 and have never had a heart attack, the benefit of taking a cholesterol-lowering drug for prevention is tiny. But the risk of muscle pain, liver stress, or even diabetes? It’s real. Or consider proton pump inhibitors (PPIs) for heartburn. Many people take them for years-even though guidelines say they should be used for only 4-8 weeks. Long-term use raises the risk of bone fractures, kidney disease, and infections.
Deprescribing works. In one study, older adults who had their benzodiazepines slowly tapered off had 22% fewer falls. Another showed fewer ER visits and better sleep after stopping unnecessary sleep aids. The key? It’s done slowly, with monitoring, and with the patient’s input. You don’t just stop a medication-you replace it with safety.
Who Should Be Leading the Conversation?
Too often, the person who knows the most about your meds isn’t your doctor-it’s your pharmacist. Pharmacists are trained to spot interactions, review entire medication lists, and flag high-risk combinations. Yet in most clinics, they’re not part of the routine visit.
Medication Therapy Management (MTM) programs, led by pharmacists, have shown real results. In one program, pharmacists reviewed the meds of 500 older adults and identified 1,200 potential issues. They stopped 300 unnecessary drugs. No one got worse. Many felt better. But these programs are still rare outside of big hospitals or Medicare Advantage plans.
Primary care doctors are stretched thin. A 15-minute appointment doesn’t leave time to untangle a 12-drug list. That’s why tools like the STOPP/START criteria exist. STOPP flags inappropriate prescriptions (like using an anticholinergic for an older adult with dementia). START flags missing prescriptions (like forgetting a bone-strengthening drug in someone with a fracture). These aren’t just checklists-they’re decision guides built on decades of research.
What You Can Do Right Now
You don’t need to wait for your doctor to bring this up. You can start today.
- Write down every pill, patch, capsule, and supplement you take-including aspirin, melatonin, glucosamine, and herbal teas.
- Ask yourself: Why am I taking this? What is it supposed to do? When was the last time my doctor reviewed this list?
- Bring this list to your next appointment-not just the paper, but the questions. Say: "I’m worried about taking too many drugs. Can we look at which ones I still need?"
- Ask if any of your meds are on the Beers Criteria list. If you’re on one, ask if there’s a safer alternative.
- Ask your pharmacist for a free medication review. Most pharmacies offer this at no cost.
Don’t stop anything on your own. But do start asking. Many older adults fear that stopping a pill will make their condition worse. But sometimes, the pill is what’s making them worse.
The Hidden Costs of Too Many Pills
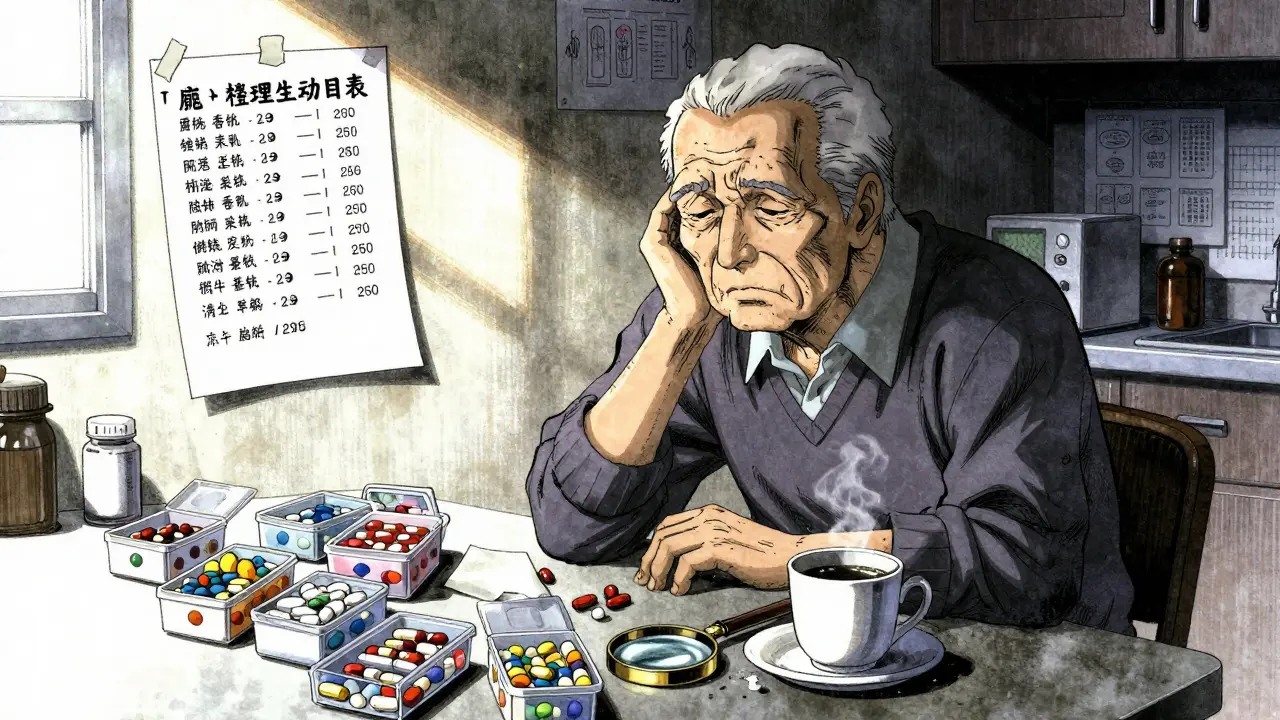
Polypharmacy doesn’t just hurt your body-it hurts your wallet and your peace of mind. A 2023 study found that older adults taking 10 or more medications spend an average of $1,800 a year just on co-pays. For those on fixed incomes, that’s food, heat, or medicine.
And then there’s the mental toll. Confusion over when to take what. Pills missed. Double doses. Caregivers overwhelmed. One woman in Texas told her nurse: "I have seven different pillboxes. I don’t know which one is for my heart, which is for my nerves, and which one I’m supposed to take on Tuesdays."
That’s not just inconvenient. It’s dangerous. And it’s preventable.
What’s Changing-and What’s Still Holding Us Back
Some progress is happening. Electronic health records now flag dangerous interactions. AI tools are being tested to predict which patients are at highest risk for polypharmacy harm. Pharmacist-led clinics are expanding in states like Minnesota and Oregon. Medicare is slowly starting to pay for comprehensive medication reviews.
But the system still rewards volume, not safety. Doctors get paid for prescribing, not for reviewing. Insurance doesn’t cover time spent talking about stopping meds. And many patients still believe: "If the doctor gave it to me, it must be necessary."
Real change means shifting from a "more is better" mindset to a "less is safer" one. It means training doctors in deprescribing. It means giving pharmacists a seat at the table. It means listening to patients-not just prescribing to them.
When to Be Concerned
Here are red flags that your or a loved one’s medication list may be too heavy:
- Frequent falls or dizziness
- Confusion or memory lapses that started after a new drug was added
- Unexplained fatigue, nausea, or loss of appetite
- Taking more than five regular medications
- Using multiple drugs for the same symptom (e.g., two sleep aids, three painkillers)
- Not knowing why you’re taking half your pills
If any of these sound familiar, it’s time to ask for a medication review. Not next year. Not when you’re next sick. Now.
Is polypharmacy always bad?
No. Some older adults need multiple medications to manage serious conditions like heart failure, diabetes, or kidney disease. The problem isn’t the number of pills-it’s whether each one is still necessary, safe, and working as intended. Polypharmacy becomes dangerous when drugs are added without review, when side effects are ignored, or when no one looks at the full list.
Can I just stop a medication if I think it’s not helping?
Never stop a medication on your own. Some drugs, like blood pressure pills, antidepressants, or steroids, can cause serious withdrawal effects if stopped suddenly. Always talk to your doctor or pharmacist first. They can help you taper off safely-or decide if the drug is even worth keeping.
What’s the difference between Beers Criteria and STOPP/START?
The Beers Criteria focuses on medications that are risky for older adults and should usually be avoided. STOPP/START is broader: STOPP finds inappropriate prescriptions (like giving an anticholinergic to someone with dementia), and START finds prescriptions that are missing (like forgetting a flu shot or a bone-strengthening drug). Together, they give a complete picture of what to stop and what to start.
Are herbal supplements safe to take with prescription drugs?
Not always. Many supplements interact dangerously with medications. St. John’s Wort can make blood thinners, antidepressants, and birth control pills less effective. Garlic and ginkgo can increase bleeding risk when taken with aspirin or warfarin. Even common vitamins like vitamin K can interfere with blood thinners. Always tell your doctor about every supplement you take-even if you think it’s "natural."
How often should my meds be reviewed?
At least once a year, and every time you see a new specialist or start a new drug. If you’re on five or more medications, ask for a full review every six months. Don’t wait for a crisis. Regular reviews catch problems before they cause falls, hospital stays, or worse.
Next Steps: Start Simple
Don’t try to fix everything at once. Pick one pill. Ask: "Why am I taking this?" Then ask your pharmacist or doctor to check if it’s still needed. Keep a log. Note how you feel after stopping or reducing something. Many people report better sleep, clearer thinking, and more energy once unnecessary drugs are gone. Safety isn’t about having fewer pills-it’s about having the right ones.





Becky Baker
26 December 2025 - 23:45 PM
I swear, my grandma takes 14 pills a day and still says she's fine. Then she falls down and we act surprised. Wake up, America. This isn't medicine, it's a pharmacy-funded circus.
Amy Lesleighter (Wales)
27 December 2025 - 06:42 AM
i used to be scared to ask my doc about cutting meds. then i stopped the sleep aid i'd been on for 8 years. slept better. walked better. didn't feel like a zombie. sometimes less is just... more.
Sandeep Jain
27 December 2025 - 08:23 AM
my dad in india takes 6 meds for blood pressure, diabetes, and his knees. but he also takes ashwagandha and turmeric powder every day. no one ever asks him about the herbs. they just add more pills. this is broken.
Sophia Daniels
27 December 2025 - 15:22 PM
Ohhh sweet jesus. Another one of these "you’re taking too many pills" rants. Let me guess-next you’ll tell me sunlight cures cancer and we should all be drinking lemon water with Himalayan salt? 🙄
My 82-year-old aunt takes 11 meds. She’s still gardening, traveling, and roasting her grandkids at Thanksgiving. You think she’d be better off if you took away her statin and her blood thinner? She’d be in a body bag by Christmas. Not all polypharmacy is dumb. Some of us actually know what we’re doing.
Steven Destiny
28 December 2025 - 15:27 PM
Stop being afraid of asking questions. Your pharmacist doesn’t care if you look dumb-they care if you live. Go right now. Print your list. Walk in. Say: "I’m tired of being a pill vending machine." They’ll thank you.
Fabio Raphael
30 December 2025 - 12:13 PM
I work in a geriatric clinic. One of our patients had 17 medications. We tapered her off 8 over 6 months. She went from barely walking to dancing at her granddaughter’s wedding. No magic. Just listening. And courage.
Natasha Sandra
31 December 2025 - 16:31 PM
I’m so glad this is getting attention!! 💖 I made my mom bring her pill organizer to her last appointment and we found THREE duplicates and a blood pressure med she hadn’t needed since 2019. She cried. I cried. We both felt so much lighter. 🙏
Sumler Luu
2 January 2026 - 09:32 AM
I’ve seen this too many times. A doctor adds a new med for a side effect of another med. It’s like building a Jenga tower with your health. One wrong move and everything crashes. I wish more doctors were trained in deprescribing. It’s not neglect-it’s precision.
Nikki Brown
4 January 2026 - 09:24 AM
I’m sorry, but if you’re over 65 and still taking NSAIDs daily, you’re not just at risk-you’re being negligent. And if you think melatonin is "natural" so it’s harmless, you clearly haven’t read the studies. This isn’t about being told what to do. It’s about being responsible enough to ask. If you don’t care enough to review your meds, don’t blame the system when you fall.
Rajni Jain
5 January 2026 - 09:23 AM
my aunt in delhi stopped her sleeping pill after we talked. she started yoga and tea at night. now she wakes up without grogginess. no one told her it was okay to try without meds. we need more gentle voices like this.
roger dalomba
5 January 2026 - 18:03 PM
Ah yes, the classic "just ask your pharmacist" solution. Because clearly, the real problem is that we haven’t yet weaponized customer service.
sakshi nagpal
7 January 2026 - 03:19 AM
In India, we often rely on family to manage medications. My grandmother’s list was written on a napkin by her neighbor. We had to take it to a pharmacist who translated it into English, then cross-checked with her doctor. It took weeks. But we removed three unnecessary drugs. She smiles more now. This isn’t just American. It’s global.
Erwin Asilom
7 January 2026 - 08:23 AM
I’m not a doctor. But I’ve watched my father take 9 pills a day for 10 years. Last year, we cut his antihistamine. He stopped feeling foggy. He started reading again. It wasn’t dramatic. It was quiet. And it mattered.