- New wave of non‑invasive options could cut recovery time.
- Regenerative medicine is moving from labs to clinics.
- Gene‑editing holds promise for lasting fixes.
- Technology‑driven devices may become discreet "smart" solutions.
Millions of men worldwide grapple with Erectile Dysfunction is the inability to achieve or maintain an erection sufficient for sexual activity. While pills like Viagra dominate headlines, researchers are racing to develop next‑generation erectile dysfunction treatment that’s faster, longer lasting, and fewer side effects. This guide walks you through the most promising therapies on the horizon, what science says today, and how you can prepare for the options that may hit the market in the next five to ten years.
Where We Stand Today
First‑line therapy still revolves around Phosphodiesterase type 5 inhibitors is a class of oral medications (e.g., sildenafil, tadalafil) that enhance blood flow by blocking the PDE5 enzyme. They work for about 70% of men with mild to moderate ED, but they require timing, have dietary restrictions, and don’t help men with severe vascular damage.
When pills fail, doctors turn to injection therapy, vacuum erection devices, or penile prosthesis is a surgically implanted device that mimics natural erection by inflating cylinders inside the penis. Implants offer high satisfaction rates but involve surgery and a recovery period.
Non‑Invasive Shockwave Therapy Takes Center Stage
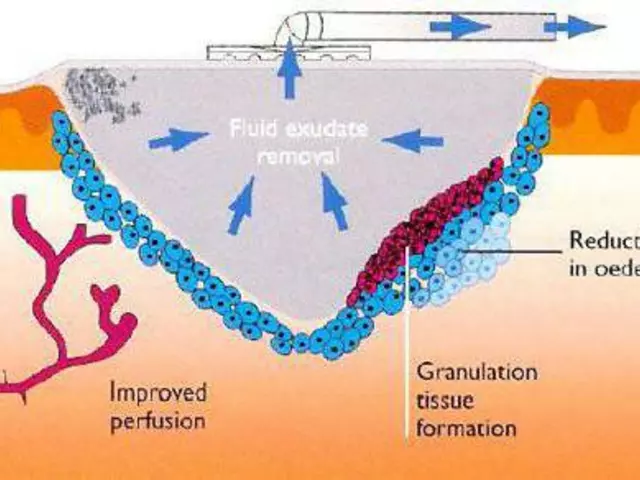
One of the hottest topics is Low‑intensity shockwave therapy is an outpatient procedure that uses acoustic waves to stimulate blood vessel growth and tissue repair in the penis. Early clinical trials report improved erectile function scores in up to 60% of participants after a series of 6‑12 sessions. Because the treatment is painless and doesn’t involve medication, many see it as a bridge between pills and surgery.
Key points to watch:
- Most studies involve men with vasculogenic ED, the most common type.
- Long‑term durability is still under study; some protocols suggest maintenance sessions every 6‑12 months.
- Regulatory approval varies by country-U.S. FDA clearance is pending for specific devices.
Regenerative Medicine: Stem Cells and PRP
Regenerative approaches aim to repair damaged tissue rather than just mask symptoms. Stem cell therapy is the injection of mesenchymal stem cells harvested from bone marrow or adipose tissue to promote angiogenesis and cellular repair in the penile tissue has shown encouraging results in small‑scale trials, with some men reporting erections strong enough for intercourse after just a few months.
Another autologous option is platelet‑rich plasma is a concentration of a patient’s own platelets injected into the penis to release growth factors that stimulate tissue regeneration. PRP is already popular in sports medicine, and early ED studies suggest modest improvements, especially when combined with shockwave therapy.
What patients should keep in mind:
- Procedures are still considered experimental; insurance rarely covers them.
- Standardized dosing and cell preparation protocols are not yet universal.
- Potential risks are low, but the long‑term safety profile is still forming.
Gene Therapy: Rewiring the Biology
Imagine a one‑time treatment that fixes the underlying cause of ED at the genetic level. Researchers are experimenting with viral vectors that deliver the gene for nitric oxide synthase directly into penile smooth muscle cells. This enzyme is essential for producing nitric oxide-a key molecule that triggers vasodilation during sexual arousal.
Animal studies have shown restored erectile function after a single injection, and early‑phase human trials are slated to start by 2027. If successful, gene therapy is a technique that introduces, removes, or modifies genetic material within a patient’s cells to treat disease could become a permanent solution for men whose ED stems from endothelial dysfunction.
Challenges remain:
- Delivery vectors must avoid immune reactions.
- Regulatory pathways for sexual health applications are still evolving.
- Long‑term off‑target effects need rigorous monitoring.
Next‑Gen Devices: Smart Implants and Wearables
Traditional penile prostheses are mechanical, but engineers are designing “smart” implants equipped with sensors and Bluetooth connectivity. These devices could auto‑adjust rigidity based on real‑time feedback, sync with smartphone apps for discreet control, and even log usage data for doctors to fine‑tune settings.
Meanwhile, wearable technology-think vibration rings or external ultrasound patches-aims to trigger erection without any internal hardware. Early prototypes use low‑frequency vibrations to stimulate pelvic nerves, offering a drug‑free option that can be used on demand.
Potential consumer benefits include:
- Reduced invasiveness compared to surgical implants.
- Personalized data that helps clinicians customize therapy.
- Greater discretion for users concerned about stigma.

Lifestyle, Digital Health, and Prevention
Even the most advanced therapies work best when paired with healthy habits. lifestyle modification is a set of changes including exercise, diet, smoking cessation, and stress management that improve vascular health and hormonal balance remains a cornerstone of ED management.
Digital platforms now offer AI‑driven coaching apps that track activity, sleep, and nutrition, providing alerts when patterns that could worsen ED emerge. Some apps integrate with wearable devices to monitor blood flow in the penile arteries, giving users real‑time feedback on how lifestyle tweaks affect performance.
Key takeaways:
- Regular aerobic exercise can boost nitric oxide levels by up to 30%.
- Mediterranean‑style diets rich in antioxidants correlate with lower ED prevalence.
- Alcohol moderation and quitting smoking can reverse early vascular damage within months.
Choosing the Right Path: What to Watch For
When new options reach the market, consider these practical questions:
- Evidence level: Look for PhaseIII trial data or FDA approval.
- Invasiveness: Non‑surgical routes (shockwave, PRP) generally have quicker recovery.
- Cost & insurance: Emerging therapies are often out‑of‑pocket; check if your provider offers reimbursement.
- Side‑effect profile: Even minimally invasive procedures can cause bruising or infection.
- Long‑term durability: Some treatments may need repeat sessions; others aim for permanence.
Discuss any new therapy with a urologist who stays current on clinical trials. A personalized plan-combining medication, minimally invasive procedures, and lifestyle tweaks-usually yields the best results.
Comparison of Emerging ED Therapies
| Therapy | Mechanism | Invasiveness | Clinical Stage (2025) | Typical Efficacy | Common Side Effects |
|---|---|---|---|---|---|
| Low‑intensity shockwave | Acoustic‑induced angiogenesis | Outpatient, non‑invasive | PhaseIII (US pending) | 50‑65% improved IIEF scores | Mild bruising, transient pain |
| Stem cell injection | Cell‑mediated tissue regeneration | Minimally invasive (needle) | PhaseII trials | 30‑45% reported improvement | Injection site discomfort, infection risk |
| PRP therapy | Growth‑factor release | Minimally invasive (needle) | PhaseII/III pilot studies | 25‑40% modest improvement | Bruising, rare allergic reaction |
| Gene therapy (NOS gene) | Viral delivery of nitric‑oxide synthase | Single injection | Pre‑clinical/early PhaseI | Potential for lasting effect | Immune response, off‑target effects |
| Smart penile prosthesis | Sensor‑driven hydraulic cylinders | Surgical implant | Prototype / limited market release | >90% patient satisfaction | Infection, mechanical failure |
Next Steps for Readers
1. Schedule a urologic evaluation to pinpoint the cause of your ED-vascular, hormonal, neurological, or psychological.
2. Ask your doctor about eligibility for clinical trials; many universities list open studies on their websites.
3. Start or refine a lifestyle modification is targeted changes in diet, exercise, and stress management that improve overall vascular health. Small tweaks often boost response to any medical therapy.
4. Keep a symptom diary. Tracking erections, medication timing, and any side effects helps clinicians tailor the right combination of treatments.
Frequently Asked Questions
Is low‑intensity shockwave therapy safe?
Current studies report a low incidence of serious adverse events. Most men experience mild bruising or temporary discomfort that resolves within a few days. Long‑term safety data are still being collected, but the procedure is considered safe for most healthy adults.
How do stem cell treatments differ from PRP?
Stem cells are living cells capable of differentiating into new tissue, while PRP is a concentrate of platelets that releases growth factors. Stem cells aim to rebuild damaged structures, whereas PRP mainly accelerates the body's natural healing processes. Both are injected into the penis, but stem cell therapy is more complex and currently less widely available.
Will gene therapy cure erectile dysfunction permanently?
The goal of gene therapy is a long‑lasting fix, but most trials are still early‑stage. Success depends on delivering the gene safely and ensuring it stays active without causing unwanted effects. If the technology matures, a single treatment could potentially replace lifelong medication, but we’re likely several years away from a definitive answer.
Are smart penile implants covered by insurance?
Most insurers cover traditional prostheses when medically necessary, but the newer “smart” versions are often classified as experimental. Coverage will depend on FDA approval status and whether the device is listed as a standard of care.
Can lifestyle changes alone improve erectile function?
Yes, especially for men with early‑stage vascular issues. Regular aerobic exercise, a balanced diet low in processed sugars, quitting smoking, and managing stress can improve blood flow and hormone levels, leading to noticeable improvements in many cases.




Michael AM
28 September 2025 - 05:56 AM
Hope this helps anyone looking into new options.
Rakesh Manchanda
1 October 2025 - 17:16 PM
While the excitement around low‑intensity shockwave is understandable, it’s worth noting that the evidence, though promising, is still evolving. The therapy offers a non‑pharmacological pathway which some patients find appealing. Yet, the need for multiple sessions and uncertain durability temper expectations. Ultimately, discussing it with a urologist will clarify if it aligns with one’s health profile.
Erwin-Johannes Huber
5 October 2025 - 04:36 AM
There’s a real benefit in staying updated on emerging therapies, especially as many are moving toward tissue regeneration rather than symptomatic relief. Keeping an eye on clinical trial registries can give early access to cutting‑edge options. Collaboration between patients and physicians ensures a tailored approach. Remember, lifestyle modifications remain a cornerstone that can augment any advanced treatment.
Tim Moore
8 October 2025 - 15:56 PM
Esteemed colleagues, the progression from invasive prosthetic solutions to regenerative modalities reflects a commendable shift in urological practice. One must appraise each innovation through the lens of rigorous clinical validation. The regulatory landscape, particularly within the United States, will ultimately dictate accessibility. Continuous professional education is paramount to integrate these advances responsibly.
Erica Ardali
12 October 2025 - 03:16 AM
Behold, the avant‑garde of masculine vitality prowls at the horizon, cloaked in the mystique of gene editing and smart implants. It is as if Prometheus himself whispered the secret of eternal vigor into the veins of modern science. Yet, amid this technocratic renaissance, we must ask whether we are chasing salvation or merely fashioning a new form of hubris. The promise of a single injection to rewrite destiny is intoxicating, but the specter of unforeseen consequences looms large. In the grand theater of human desire, the plot thickens with each CRISPR‑laden chapter.
Justyne Walsh
15 October 2025 - 14:36 PM
Oh, wonderful, another miracle gadget promising discreet erections-because nothing says confidence like a Bluetooth‑enabled prosthesis. Surely the regulatory agencies are just lining up to endorse every shiny new doodad. Meanwhile, the average Joe can’t even afford the latest prescription pill, let alone a smart implant. Maybe we should all just stick to the basics and stop glorifying techno‑fantasies.
Callum Smyth
19 October 2025 - 01:56 AM
Hey folks, if you’re considering stem‑cell or PRP treatments, remember that the science is still early but the community feedback is encouraging 😊. It’s important to choose a clinic with proper credentials and transparent protocols. Combining these therapies with lifestyle changes can magnify benefits. Don’t hesitate to ask your doctor about ongoing clinical trials.
Xing yu Tao
22 October 2025 - 13:16 PM
The epistemic shift towards regenerative urology invites a profound reevaluation of what constitutes therapeutic success. One must contemplate not merely the restoration of function but the restoration of agency within the patient’s existential narrative. Such considerations demand a multidisciplinary discourse encompassing bioethics, virology, and patient autonomy. It is incumbent upon us to navigate these waters with both scientific rigor and philosophical humility.
Adam Stewart
26 October 2025 - 00:36 AM
For those navigating this evolving landscape, it can feel overwhelming; take it one step at a time. Begin by cataloguing your personal health parameters and discussing them openly with a trusted urologist. Explore reputable sources and consider enrolling in a trial if you meet the criteria. Patience and persistence often yield the most sustainable outcomes.
Selena Justin
29 October 2025 - 10:56 AM
Indeed, the integration of digital health platforms with traditional therapy offers a synergistic avenue for management. Continuous monitoring can alert clinicians to subtle physiological shifts before they manifest clinically. Moreover, data‑driven insights empower patients to make informed lifestyle adjustments. It is advisable to select applications that adhere to stringent privacy standards.
Bernard Lingcod
1 November 2025 - 22:16 PM
What intrigues me most about low‑intensity shockwave is its potential to stimulate angiogenesis without pharmacological intervention. Could repeated sessions eventually render medication obsolete for certain cohorts? The mechanistic pathways merit deeper exploration, perhaps through interdisciplinary collaboration. I look forward to seeing longitudinal data emerge.
Raghav Suri
5 November 2025 - 09:36 AM
Listen, the hype around gene therapy is real, but the delivery vectors still pose immune challenges. Until we nail down a safe, repeatable method, it’s a gamble you don’t want to take lightly. Focus on proven options like shockwave or PRP while waiting for the tech to mature. Stay informed, stay skeptical.
Dean Gill
8 November 2025 - 20:56 PM
When evaluating the next wave of erectile dysfunction interventions, it is essential to adopt a holistic perspective that encompasses not only the physiological mechanisms but also the psychosocial dimensions of sexual health. The emergence of low‑intensity shockwave therapy represents a paradigm shift from pharmacotherapy toward mechanical stimulation of vascular growth, a concept that has been validated in limited but promising clinical cohorts. Moreover, the integration of regenerative medicine, particularly stem‑cell and platelet‑rich plasma modalities, offers a tantalizing opportunity to repair endothelial damage at its source rather than merely mask its symptoms. However, these approaches are still encumbered by variability in preparation techniques, dosing regimens, and a paucity of large‑scale, double‑blind studies. Gene‑editing technologies, notably CRISPR‑based delivery of nitric oxide synthase genes, push the frontier further into the realm of potential curative treatments, yet they also raise profound ethical and safety considerations that must be rigorously addressed. Smart penile prostheses equipped with Bluetooth connectivity and sensor feedback could eventually provide real‑time customization, blending surgical reliability with digital flexibility. Wearable ultrasound patches and vibration rings add to the tapestry of non‑invasive options, targeting neural pathways to elicit erections without internal hardware. Lifestyle interventions-regular aerobic exercise, Mediterranean diet, smoking cessation, and stress reduction-remain the foundational pillars that augment any advanced therapy’s efficacy. Digital health platforms now harness artificial intelligence to deliver personalized coaching, track biomarkers, and even predict performance fluctuations based on sleep and activity data. The convergence of these technologies suggests a future where treatment plans are dynamically adjusted in response to real‑time physiological feedback. Insurance coverage, however, lags behind innovation, often relegating emerging therapies to out‑of‑pocket expenses for patients. Clinicians must therefore remain vigilant in counseling patients about realistic expectations, potential side effects, and the importance of evidence‑based decision making. In summary, the therapeutic horizon is expanding rapidly, but the onus remains on both providers and patients to navigate this complexity with discernment and caution. Ultimately, a multimodal strategy that combines cutting‑edge modalities with proven lifestyle modifications is likely to yield the most durable outcomes.
Royberto Spencer
12 November 2025 - 08:16 AM
One could argue that the pursuit of a permanent biochemical fix borders on the philosophical desire to control nature itself. Yet, we must ask whether such mastery is ethically defensible or merely an expression of hubristic ambition. The balance between innovation and humility should guide our clinical decisions. Let us not lose sight of the human element amidst the technocratic allure.
Annette van Dijk-Leek
15 November 2025 - 19:36 PM
Wow!!! The sheer volume of emerging treatments is astounding, and it’s clear that we’re standing on the brink of a revolutionary era, isn’t it??? From shockwave to gene therapy, each option brings its own set of promises and pitfalls, demanding careful consideration!!! Patients should feel empowered, yet also cautious, as they navigate this complex landscape!!! Remember, knowledge is power, and staying informed is the best defense against speculation!!!
Katherine M
19 November 2025 - 06:56 AM
Indeed, the trajectory of erectile dysfunction therapeutics reflects a broader sociocultural shift toward personalized medicine 🌐. While we celebrate technological breakthroughs, we must also interrogate the implications for patient autonomy and informed consent 🤔. The ethical discourse should evolve in parallel with scientific progress, ensuring equity and transparency 📚. Together, these forces will shape a future where innovation serves humanity responsibly 🌟.
Bernard Leach
22 November 2025 - 18:16 PM
It is evident that the field is moving beyond simple phosphodiesterase inhibition towards interventions that aim to restore underlying vascular integrity the promise of stem cell therapy lies in its capacity to differentiate and promote angiogenesis yet the logistical challenges of cell sourcing dosing and regulatory approval remain significant the integration of low‑intensity shockwave offers a non‑pharmacologic avenue that stimulates neovascularization however durability of response is still under investigation the advent of gene therapy targeting nitric oxide pathways could, in theory, provide a durable solution but concerns about vector safety and off‑target effects cannot be ignored the rise of smart implants equipped with Bluetooth connectivity exemplifies the melding of bioengineering with digital health yet cost and insurance coverage pose barriers the convergence of lifestyle optimization, digital monitoring, and regenerative techniques suggests a future where treatment is highly individualized however the disparity in access to cutting‑edge care threatens to widen health inequities it is incumbent upon clinicians to stay abreast of emerging data and to guide patients through nuanced risk‑benefit analyses while advocating for broader coverage policies that reflect the evolving standard of care
Mark Eaton
26 November 2025 - 05:36 AM
Keep pushing forward, folks-every new study brings us closer to better solutions! Stay curious, stay proactive, and don’t settle for the status quo. Your health journey is worth the effort.
Alfred Benton
29 November 2025 - 16:56 PM
It is no coincidence that the rush to approve smart prosthetic devices aligns with broader surveillance initiatives. Hidden agendas often lurk behind the veneer of innovation, seeking data collection rather than genuine patient benefit. Scrutinize the funding sources and regulatory pathways before embracing such technology. Vigilance is essential to protect personal autonomy.
Susan Cobb
3 December 2025 - 04:16 AM
Contrary to popular belief, the hype around wearable ultrasound patches is largely a marketing ploy with limited clinical backing. The underlying physics simply cannot generate sufficient penile blood flow in most cases. I advise readers to invest in proven therapies rather than chasing flash trends. Critical appraisal should always precede adoption.