Bone Nutrition Calculator
Assess Your Bone Health Nutrition
Enter your daily nutrient intake to see if you're meeting bone-strengthening targets.
Want to keep your skeleton sturdy as you age? Learning how to build stronger bones and stop damage before it starts is easier than you think. Below you’ll find a step‑by‑step guide that covers nutrition, movement, and habits that protect your bone health for the long run.
Understanding Bone Structure
Bones aren’t static; they’re living tissue that constantly remodels itself. Two main processes drive this:
- Bone formation - new bone is laid down by cells called osteoblasts.
- Bone resorption - old bone is broken down by osteoclasts.
When formation outpaces resorption, density improves. The opposite leads to thinning and a higher risk of fractures.
Key Nutrients for Strong Bones
Certain minerals and vitamins act as the building blocks for the remodeling cycle. Below are the most vital ones, each introduced with schema markup for easy reference.
Calcium is the primary mineral that gives bones their rigidity. Adults need about 1,000mg daily, rising to 1,200mg after age50. Sources include dairy, fortified plant milks, leafy greens, and sardines.
Vitamin D helps the gut absorb calcium efficiently. A blood level of 30ng/mL is considered sufficient. Sunlight exposure (10‑15minutes a day) plus foods like fatty fish and egg yolks usually cover the 600‑800IU recommended for most adults.
Magnesium works together with calcium and vitamin D to activate the enzymes that build bone matrix. The RDA is 310‑420mg, found in nuts, seeds, whole grains, and dark chocolate.
Vitamin K2 directs calcium to the skeleton instead of soft tissues. Fermented foods like natto, cheese, and sauerkraut are rich sources.
Protein provides the collagen framework that mineral deposits attach to. Aim for 0.8g per kilogram of body weight daily, choosing lean meats, legumes, and dairy.
Best Foods to Boost Bone Nutrition
Pairing calcium‑rich and vitamin‑D‑rich foods in the same meal maximizes absorption. The table below compares popular options.
| Calcium‑rich (mg per serving) | Vitamin‑D‑rich (IU per serving) |
|---|---|
| Greek yogurt (200g) - 250mg | Salmon (100g) - 560IU |
| Collard greens (1 cup cooked) - 266mg | Fortified orange juice (1 cup) - 100IU |
| Almonds (30g) - 76mg | Egg yolk (1 large) - 41IU |
| Sardines with bones (90g) - 325mg | Mushrooms (½ cup, UV‑treated) - 400IU |

Exercise Strategies that Strengthen Bones
Physical stress signals the body to lay down more mineral, much like a builder adds extra support when a bridge bears weight. Two exercise categories are most effective:
- Weight‑bearing exercise - activities where you support your own weight, such as walking, jogging, dancing, and hiking.
- Resistance training - lifting weights or using resistance bands to apply direct load to bones.
Aim for at least 150 minutes of moderate weight‑bearing activity weekly, plus two sessions of resistance training focusing on major muscle groups (squats, deadlifts, push‑ups). Balance drills like tai‑chi also reduce fall risk, a key factor in preventing fractures.
Lifestyle Habits to Avoid Bone Damage
Even with perfect nutrition and workouts, certain habits erode bone density over time.
- Smoking reduces calcium absorption and accelerates bone loss. Quitting can regain up to 2% of lost bone density within a year.
- Excess alcohol (more than 2 drinks/day) interferes with vitamin D metabolism.
- High‑salt diets increase calcium excretion in urine; keep sodium below 2,300mg per day.
- Prolonged sedentary periods (e.g., sitting over 8hours/day) signal the body to ramp up resorption.
Supplements & When to Use Them
If you struggle to meet nutrient targets through food, supplements can fill gaps-but they’re not a free pass.
- Calcium citrate - better absorbed on an empty stomach; limit total supplemental dose to 500mg at a time.
- Vitamin D3 - 1,000‑2,000IU daily for most adults; higher doses (4,000IU) may be prescribed after a blood test.
- Magnesium glycinate - gentle on the gut, 200‑300mg split across meals.
- Vitamin K2 (MK‑7) - 100µg daily, especially if you’re on a calcium supplement.
Always discuss with a healthcare provider before starting any regimen, especially if you take blood thinners or have kidney disease.
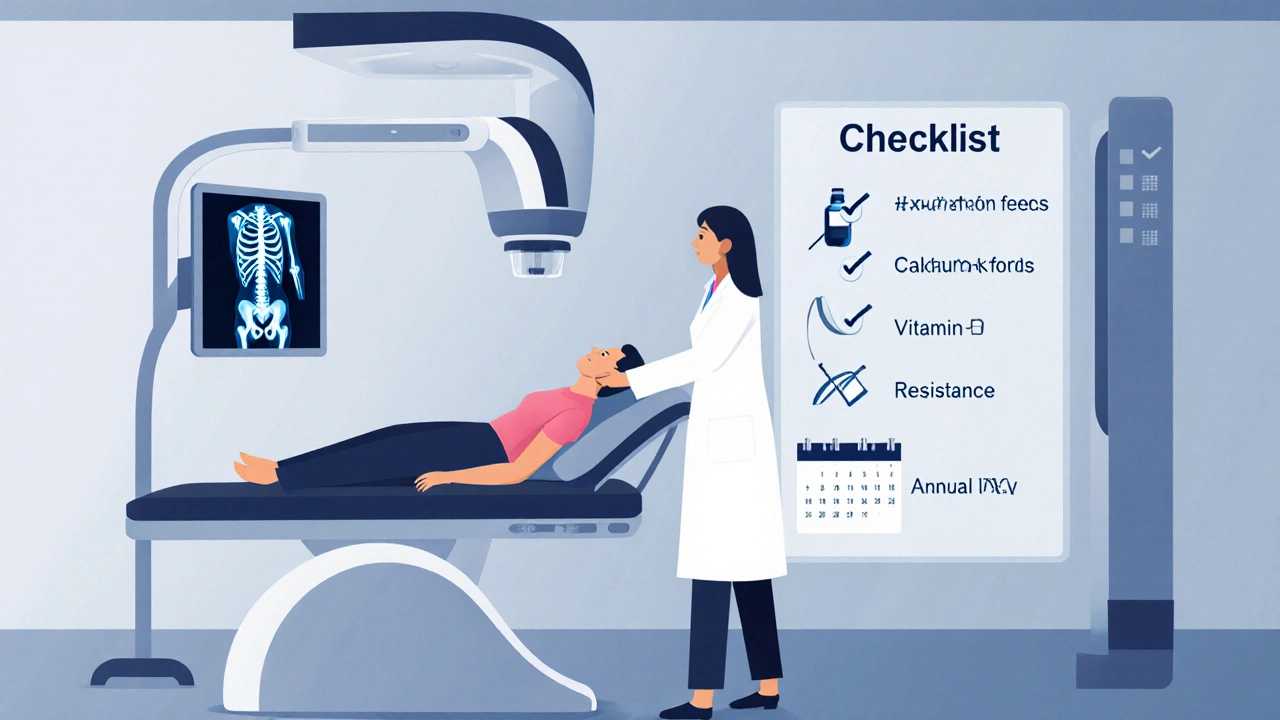
Monitoring Bone Health
The most reliable way to track progress is a bone density scan (DXA). It measures bone mineral density (BMD) at the hip and spine, reporting results as a T‑score:
- ‑1.0 or above: normal
- ‑1.0 to ‑2.5: low bone mass (osteopenia)
- ‑2.5 or below: osteoporosis
Women should start screening at age65 (or earlier if risk factors exist). Men are advised to begin at 70. Repeat every 2‑3years unless you have a condition that accelerates loss.
Quick Checklist for Stronger Bones
- Consume 1,000‑1,200mg calcium daily from dairy, leafy greens, or fortified foods.
- Get 600‑800IU vitaminD from sunlight, diet, or supplements.
- Include magnesium (300‑420mg) and vitaminK2 weekly.
- Do 150min of weight‑bearing activity + two resistance sessions each week.
- Limit smoking, alcohol, and high‑salt foods.
- Schedule a DXA scan at recommended ages or after a fracture.
Frequently Asked Questions
How much calcium is too much?
Adults shouldn’t exceed 2,500mg per day (3,000mg for women over 50). Excess calcium can raise kidney stone risk and may interfere with heart health.
Can vegans get enough vitamin D?
Yes. UV‑treated mushrooms, fortified plant milks, and a daily 1,000‑2,000IU D3 supplement (vegan‑derived) usually cover needs.
Is weight‑bearing exercise safe for people with arthritis?
Low‑impact options like brisk walking, stair climbing, and water‑based aerobics provide bone stimulus while sparing joints. Start slowly and increase intensity under a physiotherapist’s guidance.
What’s the best time of day to take calcium supplements?
Split doses and take them with meals to improve absorption. Avoid taking calcium with iron or high‑dose zinc supplements.
Can I reverse early osteoporosis without medication?
Lifestyle changes-adequate calcium, vitaminD, weight‑bearing activity, and quitting smoking-can halt progression and modestly improve BMD. Medication may still be needed for higher‑risk cases.



Brian Rice
12 October 2025 - 22:13 PM
Your post overstates the importance of supplements at the expense of real nutrition.
Stan Oud
13 October 2025 - 00:26 AM
I guess the calcium recommendation is fine but the vitamin D emphasis feels… overblown??
Ryan Moodley
13 October 2025 - 03:46 AM
Bones are not just inert rods, they are living factories constantly remodeling themselves.
When you think about that process, you realize it mirrors the way our habits shape our lives.
The article correctly mentions osteoblasts and osteoclasts, but it glosses over the hormonal orchestra that conducts them.
For instance, parathyroid hormone spikes when calcium dips, calling osteoclasts to the frontline.
Simultaneously, estrogen acts like a diplomat, calming the resorption crew and encouraging formation.
That is why post‑menopausal women experience accelerated bone loss without hormonal balance.
The nutrient list-calcium, vitamin D, magnesium, K2-forms a quartet, yet the article treats them as soloists.
Vitamin D is the backstage manager that makes calcium absorbable; without it, even a dairy binge won’t help.
Magnesium, often ignored, is the unsung co‑factor that activates the enzymes turning raw material into bone matrix.
K2, the traffic controller, directs calcium to the skeleton instead of the arteries, reducing vascular calcification.
Exercise, especially weight‑bearing and resistance work, sends mechanical signals that activate the same pathways as hormones.
The body perceives the load as a call to reinforce, depositing more mineral where stress is greatest.
However, the article neglects the role of chronic inflammation-think high‑sugar diets-that can tip the balance toward resorption.
Smoking and excessive alcohol act as accelerants, eroding bone at a molecular level, which the guide mentions only in passing.
In short, a holistic approach that synchronizes diet, movement, and lifestyle is the true prescription for bone longevity.
carol messum
13 October 2025 - 05:10 AM
Eating a mix of dairy, leafy greens, and getting a bit of sun each day is a solid start for bone health.
aarsha jayan
13 October 2025 - 06:16 AM
Great points! To make those ideas actionable, try pairing a calcium‑rich snack like yogurt with a short walk outdoors-your body will thank you.
Rita Joseph
13 October 2025 - 07:06 AM
Don’t forget to sprinkle some nuts for magnesium and consider a vitamin D supplement in winter; consistency beats occasional intensity.
Abhishek Vora
13 October 2025 - 07:48 AM
While dairy is a convenient calcium source, fortified plant milks can match or exceed the content, and absorption rates are comparable when vitamin D status is adequate.
Lily Saeli
13 October 2025 - 08:46 AM
We often forget that bones are a reflection of the choices we make every day, not just occasional supplements.
Joshua Brown
13 October 2025 - 09:20 AM
Exactly!; the synergy of nutrition, movement, and lifestyle creates a resilient skeletal framework; without it, we risk fragile foundations.
andrew bigdick
13 October 2025 - 10:35 AM
Balance is key-no single food or exercise will do the whole job alone.
sachin shinde
13 October 2025 - 11:25 AM
Indeed, the phrase “balance is key” is colloquial; a more precise formulation would be “homeostasis of mineral metabolism and mechanical loading is essential for maintaining bone density.”
Leon Wood
13 October 2025 - 13:05 PM
Let’s keep the momentum going and hit those weight‑bearing workouts three times a week-your future self will thank you.
Shivaraj Karigoudar
13 October 2025 - 14:28 PM
From a biomechanical perspective, the osteogenic stimulus generated during repetitive impact activities initiates mechanotransduction pathways that upregulate the Wnt/β‑catenin signaling cascade, thereby enhancing osteoblast proliferation; concurrently, resistance training imposes tensile stress on the periosteum, prompting periosteal apposition and increasing cortical thickness, which collectively mitigates age‑related porosity, improves moment‑of‑inertia, and reduces fracture risk across the skeletal system.
Moreover, integrating progressive overload ensures that the skeletal adaptation doesn't plateau, while proper recovery periods prevent microfracture accumulation.
Nutrition should mirror this effort: calcium citrate taken in divided doses maximizes intestinal uptake, whereas vitamin D3 supplementation maintains serum 25‑OH levels within the optimal range.
Finally, periodic DXA scans provide quantitative feedback, allowing you to calibrate training intensity and dietary intake for sustained bone health.
Matt Miller
13 October 2025 - 15:35 PM
Short walks and a glass of milk can be a surprisingly effective bone‑boosting combo.
Fabio Max
13 October 2025 - 16:25 PM
True, the simplicity of that routine removes barriers; just remember to keep the milk low‑fat if you’re watching calories, and aim for at least 30 minutes of brisk walking to trigger the mechanosensory response in your femur and tibia.