Every year, millions of people wear contact lenses without a second thought. They’re convenient, discreet, and for most, safe. But if you wear contacts-especially overnight-you’re taking a risk most people don’t even know about. Corneal ulcers are one of the most dangerous complications, and they can blind you in days if ignored.
What Exactly Is a Corneal Ulcer?
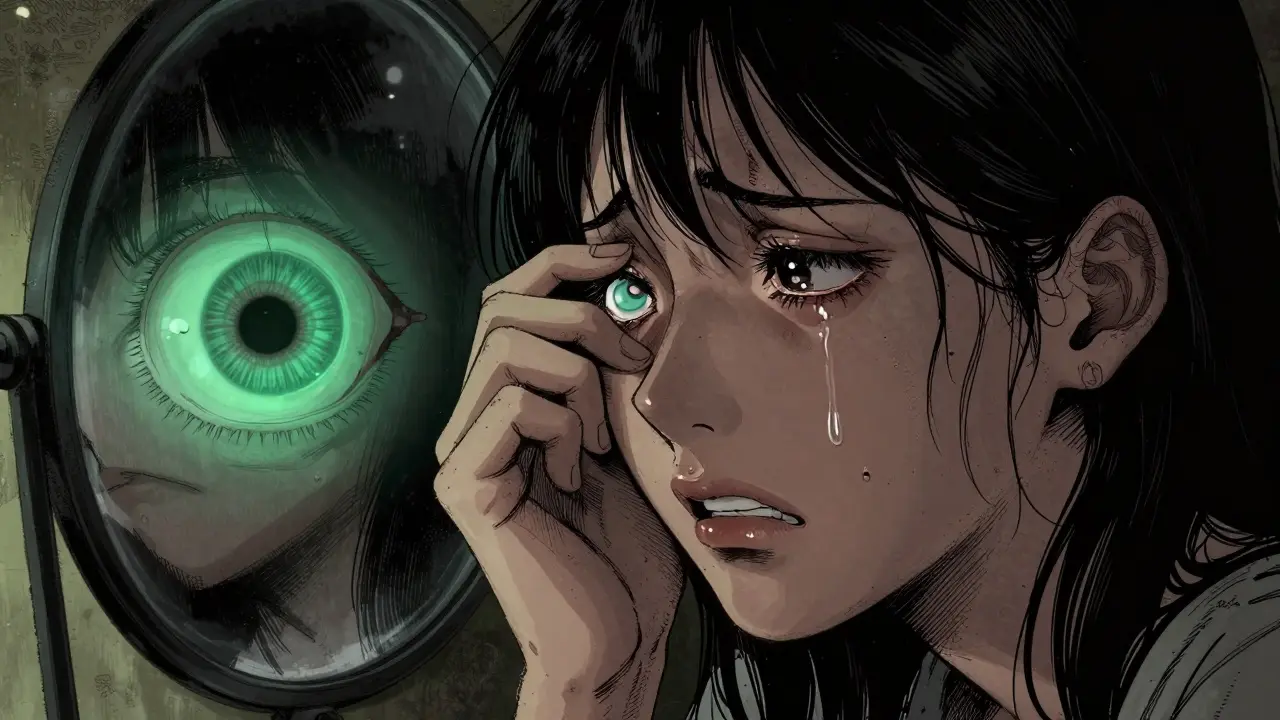
A corneal ulcer isn’t just a scratch or irritation. It’s an open sore on the clear front surface of your eye-the cornea. Think of it like a deep wound on your skin, but inside your eye. This isn’t something that heals on its own. It’s caused by infection, usually bacteria, fungi, or even a tiny amoeba called Acanthamoeba, that gets trapped under your contact lens and starts eating away at the corneal tissue. The difference between a corneal abrasion and a corneal ulcer matters. An abrasion is a surface scratch. It’s painful, but it usually heals in a day or two. A corneal ulcer? It’s tissue loss. It can spread. It can scar. And if it reaches the center of your cornea, your vision could be permanently damaged.Why Contact Lenses Are the Top Culprit
You’re about 10 times more likely to get a corneal ulcer if you wear contacts than if you don’t. That number jumps to 100 times higher if you sleep in them. That’s not a typo. Sleeping in contacts cuts off oxygen to your cornea, creates a warm, moist pocket where germs thrive, and traps dirt, bacteria, and even saliva from your pillow under the lens. Soft contact lenses, especially extended-wear types designed for overnight use, are the biggest offenders. Even if you clean them perfectly, bacteria from your fingers during insertion can get under the lens. Water is another silent killer. Showering, swimming, or even splashing your face with water while wearing contacts can introduce dangerous microbes. The FDA has issued multiple warnings about specific lens solutions linked to fungal and amoebic infections. Other risk factors include:- Wearing lenses past their replacement date
- Using tap water or saliva to clean lenses
- Scratched or damaged lenses
- Having dry eyes, blepharitis, or conditions like Bell’s palsy that prevent full eyelid closure
- Using steroid eye drops without medical supervision
Symptoms You Can’t Ignore
If you wear contacts and notice any of these, stop wearing them immediately and call your eye doctor-today:- Severe eye pain, worse than a headache
- Red, bloodshot eye that won’t improve
- Blurry, hazy, or cloudy vision
- White or gray spot on the clear part of your eye
- Excessive tearing or pus-like discharge
- Extreme sensitivity to light-even turning on a lamp feels unbearable
- Feeling like something’s stuck in your eye, even when there’s nothing there
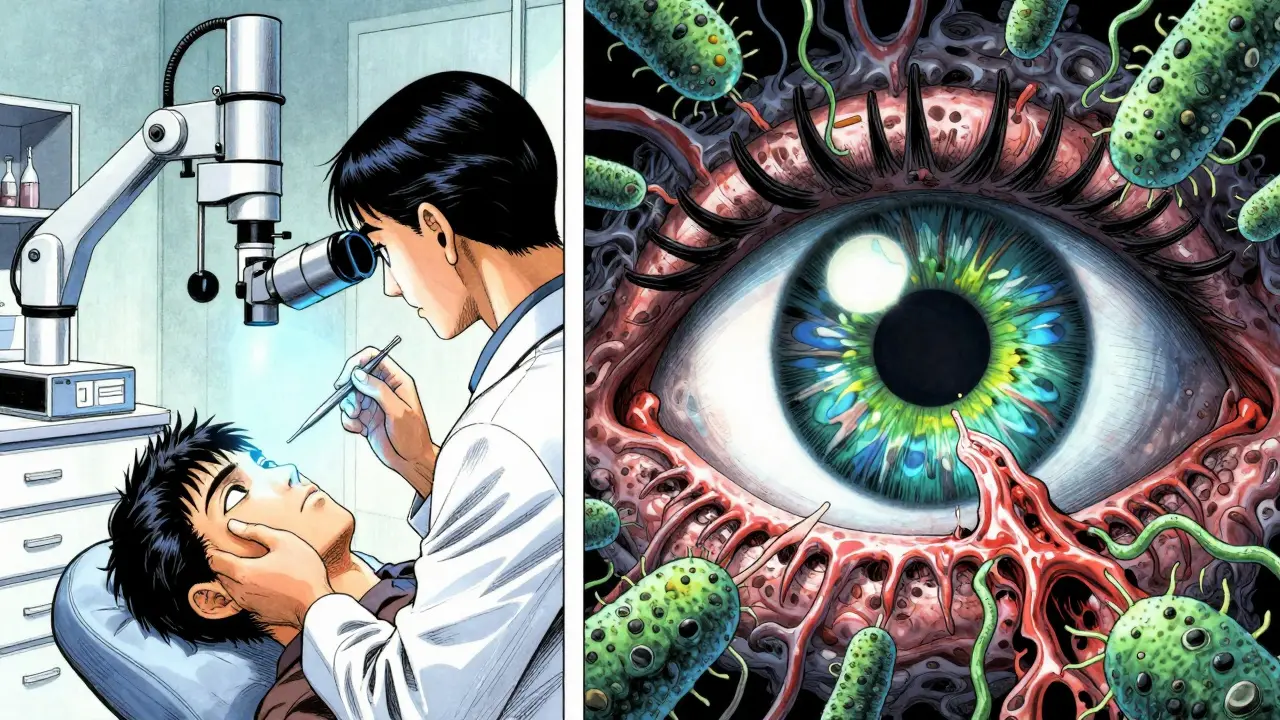
How Doctors Diagnose a Corneal Ulcer
Your eye doctor won’t just look at your eye. They’ll use specialized tools to see what’s happening beneath the surface. First, they’ll put a yellow dye called fluorescein in your eye. Under blue light, any damaged areas on the cornea glow green, making the ulcer visible. Then they’ll use a slit-lamp-a high-powered microscope with a bright light-to examine the size, depth, and location of the sore. If it looks serious, they’ll gently scrape a tiny bit of tissue from the ulcer and send it to a lab. This culture test tells them exactly what’s causing the infection: bacteria? fungus? amoeba? That’s critical because each needs a different treatment. They’ll also check your vision, measure the curvature of your cornea, and monitor for signs the infection is spreading.Treatment: Speed Is Everything
There’s no time to wait. Treatment starts the moment the ulcer is suspected-even before test results come back. For most bacterial ulcers, doctors prescribe strong antibiotic eye drops-usually fluoroquinolones like ciprofloxacin or moxifloxacin. You’ll need to use them every hour or two, day and night, for the first few days. That’s not a suggestion. That’s the protocol. If it’s a fungal infection, you’ll need antifungal drops, which are harder to get and take longer to work. Viral ulcers, often from herpes, are treated with antivirals like acyclovir. In severe cases-where the ulcer is larger than 2 mm, close to the center of your vision, or getting worse after 48 hours of treatment-you might need hospitalization. Some patients require surgery to remove infected tissue or even a corneal transplant if the damage is too deep. Steroid drops? They’re sometimes used to reduce swelling, but only under strict supervision. Using them without knowing the cause of the infection can make things worse-fast.Prevention: The Only Real Safety Net
The best treatment for a corneal ulcer is not having one in the first place. Here’s what actually works:- Never sleep in your contacts. Even if they’re labeled “extended wear,” your eyes don’t get enough oxygen when your eyelids are closed. The 100x risk increase isn’t hype-it’s science.
- Replace lenses on schedule. Daily disposables are safest. If you use monthly lenses, throw them out after 30 days, no exceptions.
- Wash your hands before touching your lenses. Soap and water. Dry with a lint-free towel. Don’t use paper towels-they shed fibers.
- Use only the solution your doctor recommends. Never reuse old solution. Never top off the case. Never use water, saliva, or homemade saline.
- Take your lenses out before swimming, showering, or hot tubbing. Water is not your friend.
- Give your eyes a break. Wear glasses at least one day a week. Let your cornea breathe.
- Inspect your lenses daily. If you see a scratch, tear, or buildup you can’t clean off, toss it.

What to Do Right Now
If you’re wearing contacts and have any of the symptoms listed above:- Take your lenses out immediately.
- Do NOT rub your eye.
- Do NOT use over-the-counter eye drops unless they’re preservative-free artificial tears.
- Call your eye doctor right away. If you can’t reach them, go to an emergency room or urgent eye care center.
- Bring your lens case and solution with you. The doctor may need to test them.
Why This Isn’t Just a Minor Issue
The FDA calls corneal ulcers a “serious hazard” that can lead to blindness. And it’s not rare. With over 85 million contact lens wearers worldwide, thousands develop ulcers every year. Many of them didn’t think they were at risk. They cleaned their lenses. They didn’t sleep in them-every night. But one missed step, one splash of water, one extra day of wear, and it’s enough. Technology is improving. Newer lens materials allow more oxygen. Diagnostic imaging helps catch ulcers earlier. But none of that replaces good habits. No lens is foolproof. No solution is magic. Your eye’s health depends on you.What Comes After Recovery
Even if your ulcer heals completely, you’ll need follow-up visits. Scarring can develop weeks later. Your vision might not return to 100%. Some people can’t wear contacts again. Others need to switch to daily disposables and follow stricter rules. The goal isn’t just to heal the ulcer. It’s to prevent it from ever coming back.Can corneal ulcers go away on their own?
No. Corneal ulcers are open sores caused by infection. They don’t heal without treatment. Delaying care increases the risk of permanent scarring, vision loss, or even eye removal in extreme cases. What feels like irritation today could be irreversible damage in 48 hours.
Are daily contacts safer than monthly ones?
Yes. Daily disposable lenses are the safest option because you’re using a brand-new, sterile lens every day. There’s no buildup of protein, bacteria, or debris. Monthly lenses require cleaning and storage, which introduces more chances for contamination-even if you do everything right.
Can I wear contacts again after a corneal ulcer?
Maybe, but not right away. Your eye doctor will need to confirm the ulcer is fully healed and your cornea has regained strength. Many patients switch to daily disposables and avoid overnight wear. Some are advised to stop wearing contacts entirely. It depends on the severity of the damage and how well you follow hygiene rules going forward.
Is it safe to use eye drops from the pharmacy for a red eye?
No. Over-the-counter redness-relief drops only mask symptoms-they don’t treat infection. If you have a corneal ulcer, these drops can delay diagnosis and make things worse. Never use them if you wear contacts and have pain, light sensitivity, or vision changes.
How fast can a corneal ulcer cause blindness?
In as little as 24 to 48 hours, especially with bacterial infections like Pseudomonas. These infections spread rapidly under contact lenses. That’s why immediate medical care is non-negotiable. Waiting until your eye feels better is the biggest mistake people make.


Katie Mccreary
29 January 2026 - 10:22 AM
I wore contacts for 8 years and never thought twice until I got a nasty infection. Turned out my lens case was gross-like, biofilm city. I threw everything away and switched to dailies. Best decision ever.
SRI GUNTORO
29 January 2026 - 22:56 PM
People today think convenience is more important than their vision. I’ve seen this happen too many times. No one wants to hear it, but if you’re sleeping in lenses, you’re basically gambling with your eyes. And guess what? The house always wins.
Kevin Kennett
30 January 2026 - 15:46 PM
Look, I get it-contacts are easy. But if you’re not treating your eyes like the delicate, irreplaceable organs they are, you’re asking for trouble. I’m an optometrist. I’ve seen people lose vision over a single night of lazy hygiene. Don’t be that person. Wash your hands. Replace your case every month. Stop using water. It’s not that hard.
Jess Bevis
31 January 2026 - 14:24 PM
Just got back from India. Saw a guy in Delhi wearing contacts while riding a motorbike through dust. No goggles. No protection. Just… eyes. Scary.
Rhiannon Bosse
31 January 2026 - 20:19 PM
Okay but have you heard about the government hiding the truth about contact lens chemicals? 🤔 I read a blog that said the FDA approves solutions that literally feed Acanthamoeba. And they’re ALL linked to Big Pharma. Why do you think they don’t warn you about this? 🤫👁️🗨️
doug b
1 February 2026 - 18:30 PM
My buddy got a corneal ulcer after swimming in a lake with his contacts in. He ended up in the ER. Now he only wears glasses. Best thing that ever happened to him. Don’t be stubborn. Your eyes don’t care how cool you think you are.
Jeffrey Carroll
3 February 2026 - 02:00 AM
While the medical information presented here is accurate and well-documented, I believe it is equally important to emphasize the psychological burden that such conditions place on patients. The fear of permanent vision loss can be as debilitating as the physical symptoms themselves.
Mel MJPS
3 February 2026 - 20:22 PM
OMG I had this happen last year. Thought it was just dry eyes. Turned out I had a tiny scratch on my lens I didn’t see. Took me 3 days to finally go to the doctor. Felt like my eye was on fire. Don’t wait. Just go.
Amber Daugs
3 February 2026 - 23:02 PM
People who wear contacts are just lazy. If you can’t be bothered to wash your hands or replace your case, why are you even wearing them? Your vision isn’t a luxury-it’s a responsibility. And you’re failing.
matthew martin
5 February 2026 - 08:43 AM
I used to be the guy who slept in his lenses ‘just one night.’ Then I woke up with a red eye that looked like a tomato with a pupil. Now I treat my eyes like a newborn kitten-gentle, clean, and never ignored. Dailies for life. No regrets.
Colin Pierce
6 February 2026 - 06:57 AM
One thing nobody talks about: your lens case is a germ hotel. I clean mine with rubbing alcohol every week and let it air dry. No solution residue. No biofilm. Simple. Free. Works. Also, never top off the case-dump it and refill. It’s not rocket science.
Mark Alan
6 February 2026 - 14:05 PM
USAF veteran here. We used to have drills for this exact thing in basic training. ‘If your eye hurts and you wear contacts-TAKE THEM OUT.’ Simple. No drama. No excuses. You want to see your kids grow up? Then stop being dumb. 🤡👁️
Ambrose Curtis
8 February 2026 - 09:05 AM
so i got this ulcer last year and it was wild. i thought it was just redness so i kept wearing my lenses. big mistake. ended up in the er at 3am with a doc who looked at me like i was an idiot (fair). now i use dailies, wash my hands like i’m about to perform surgery, and never touch my eyes without thinking ‘is this worth it?’
Linda O'neil
9 February 2026 - 06:14 AM
You got this! I know it’s overwhelming, but changing your habits is totally doable. Start with one thing-like switching to dailies. Then add another. You’re not alone. So many of us have been there. Your eyes will thank you.
Robert Cardoso
9 February 2026 - 18:41 PM
It’s not the lenses. It’s not the solutions. It’s the systemic failure of modern society to prioritize bodily autonomy over convenience. We’ve commodified our senses. We treat our eyes like disposable tech. And when they fail, we blame the victim instead of the culture that normalized this negligence.