Ulcerative Colitis: What to Watch For and What Helps
Ulcerative colitis (UC) is an inflammatory condition that affects the colon and can show up suddenly or slowly. If you’ve been dealing with persistent diarrhea, blood in stool, cramps, or urgent trips to the bathroom, this page gives clear, useful steps you can take and what to expect from treatment.
First, know the common signs: bloody diarrhea, abdominal pain usually on the left side, fatigue, and weight loss. Fever or fast heart rate during a flare can mean the inflammation is severe. Those are not symptoms to ignore.
Treatment options
Doctors use several medicine classes to control UC. Aminosalicylates (like mesalamine) help mild to moderate disease and reduce inflammation in the colon lining. If that’s not enough, short courses of corticosteroids calm flares quickly but aren’t for long-term use because of side effects.
For moderate to severe UC, immunomodulators and biologic drugs target parts of the immune system that drive inflammation. Newer pills (JAK inhibitors) are another option for some people. Surgery—removing the colon—can cure UC but comes with lifestyle changes; it’s a valid choice when meds fail or complications arise.
Always talk with your GI doctor about risks and benefits. Medication choices depend on how much colon is affected, past treatments, and other health issues.
Daily management & diet tips
There’s no single “UC diet,” but small, practical tweaks can ease symptoms. During flares try low-residue foods to reduce bowel frequency: mashed potatoes, white rice, cooked carrots, and lean proteins. Avoid high-fiber, greasy, or very spicy foods until things calm down.
Stay hydrated—diarrhea can cause rapid fluid and salt loss. If you’re anemic, iron supplements or IV iron may be necessary; check levels with your doctor. Vitamin D and B12 are commonly low in people with UC, so testing and supplementing when needed makes a difference.
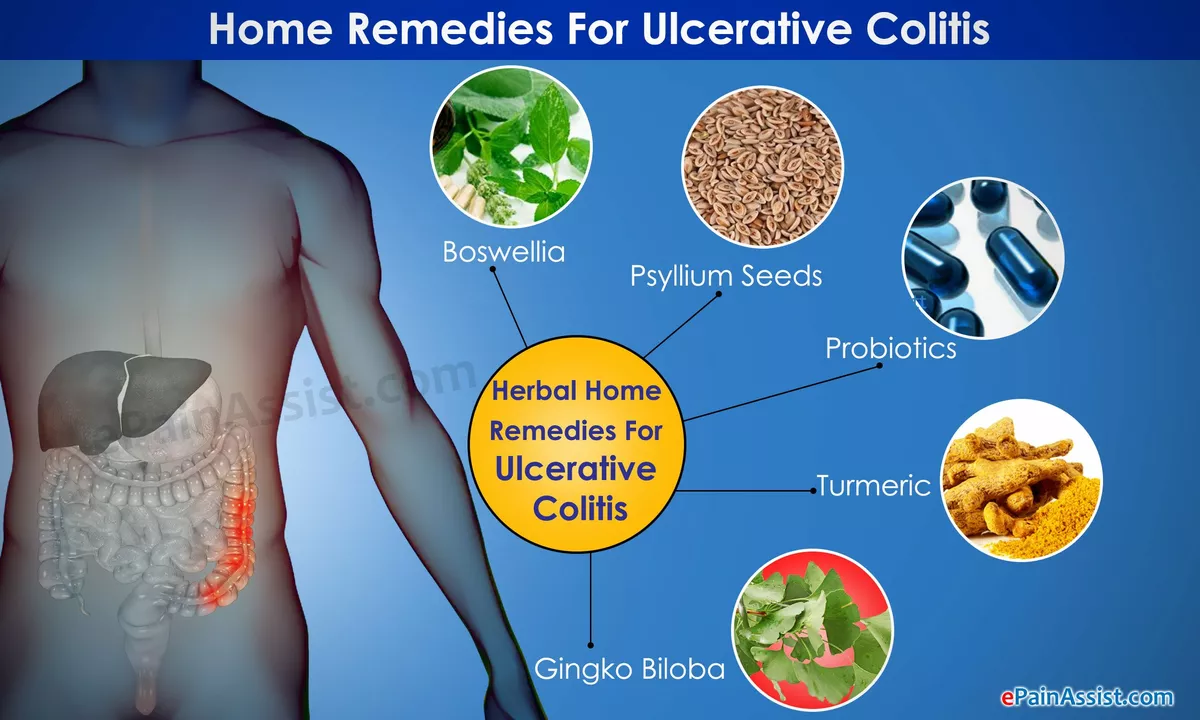
Probiotics help some people, especially with milder symptoms or pouchitis after surgery, but results vary. Keep a food diary to spot personal triggers like dairy, caffeine, or artificial sweeteners.
Manage stress and sleep—both affect flares. Gentle exercise, breathing exercises, and regular sleep patterns reduce symptom severity for many people. Stay up to date on vaccinations before starting immunosuppressive drugs, and coordinate care if you have other conditions.
Know when to call your doctor: heavy bleeding, severe abdominal pain, high fever, fainting, or signs of dehydration require urgent care. Also reach out if medications stop working or side effects become troubling.
Living with UC is a balance of treatment, diet, and lifestyle. Work with your care team, track symptoms, and make small, consistent changes. That approach often brings the best control and helps you get back to daily life faster.
The Importance of a Balanced Diet for Ulcerative Colitis Management
As someone with ulcerative colitis, I cannot stress enough the importance of maintaining a balanced diet for effective management of this condition. A well-rounded diet not only helps reduce inflammation but also aids in maintaining overall gut health. Including a variety of nutrient-rich foods like fruits, vegetables, whole grains, and lean proteins can make a significant difference in symptom management. It's also crucial to pay attention to any personal food triggers and avoid them. Remember, a balanced diet is key to keeping ulcerative colitis under control, so make sure to consult with a healthcare professional or dietitian to find the best plan for you.
Read More