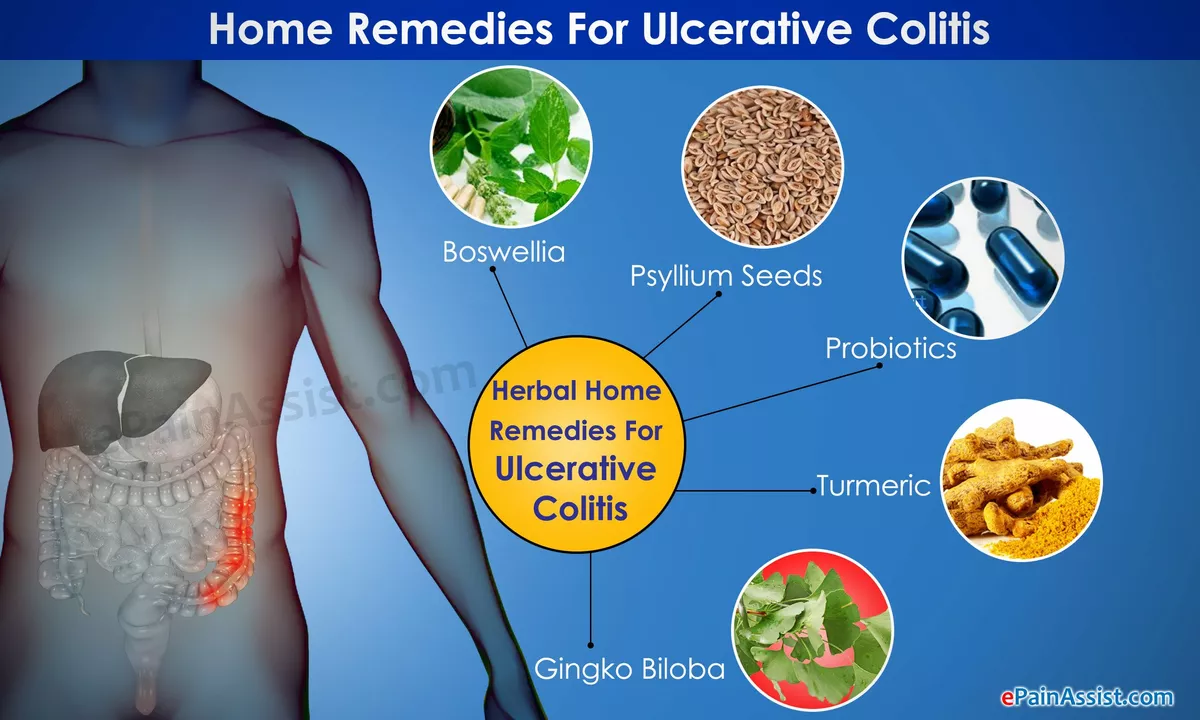
Understanding Ulcerative Colitis and Its Impact on the Gut
As someone who has been dealing with ulcerative colitis (UC) for a while now, I understand the importance of a balanced diet in managing this chronic inflammatory bowel disease. UC affects the lining of the large intestine and rectum, causing inflammation and ulcers. This can lead to abdominal pain, diarrhea, and bloody stools. Over time, UC can significantly impact your quality of life and increase the risk of complications.
In this article, I will break down the importance of a balanced diet for UC management. We will explore how specific nutrients and food choices can help alleviate symptoms, promote gut health, and reduce the risk of flare-ups. So, let's dive into the essential components of a diet tailored for UC management.
Key Nutrients for Maintaining Gut Health and Reducing Inflammation
A balanced diet for UC management should focus on providing key nutrients that promote gut health and reduce inflammation. This includes fiber, antioxidants, and omega-3 fatty acids. Fiber is essential for maintaining regular bowel movements and can help alleviate constipation, which is a common issue for those with UC. Antioxidants, such as vitamin C, vitamin E, and beta-carotene, play a role in reducing inflammation and protecting the gut lining. Omega-3 fatty acids, found in fish and certain plant sources, are known for their anti-inflammatory properties and can help in managing UC symptoms.
It is crucial to incorporate these nutrients into your daily meals by including a variety of fruits, vegetables, whole grains, and lean protein sources. However, it's important to note that individual tolerance to specific foods may vary, so it's essential to pay attention to your body's reactions and adjust your diet accordingly.
Hydration Is Key for Ulcerative Colitis Management
Staying hydrated is crucial for everyone, but it becomes even more important when you have UC. Diarrhea and frequent bowel movements can lead to dehydration, which can exacerbate symptoms and contribute to fatigue. Drinking plenty of water throughout the day can help maintain hydration levels and support overall gut health.
Aim for at least eight cups of water per day, and consider adding electrolyte-rich beverages like coconut water or sports drinks to replenish lost minerals. Avoiding caffeine and alcohol, which can trigger UC symptoms, is also a wise choice for maintaining proper hydration.
Probiotics and Their Role in Ulcerative Colitis Management
Probiotics are beneficial bacteria that live in our gut and play a crucial role in maintaining a healthy digestive system. They can help restore the balance of gut bacteria, reduce inflammation, and improve overall gut health. For people with UC, incorporating probiotics into the diet can be beneficial for symptom management.
Probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi can be easily added to your daily meals. If you're unable to tolerate these foods, consider taking a probiotic supplement after consulting with your healthcare provider.
Identifying and Avoiding Food Triggers for Ulcerative Colitis
Each person with UC may have different food triggers that can exacerbate symptoms and lead to flare-ups. Identifying and avoiding these triggers is critical for successful UC management. Common food triggers include spicy foods, high-fat foods, caffeine, alcohol, and certain high-fiber foods.
Keeping a food diary can help you track your symptoms and identify any potential triggers. Once you have a better understanding of your triggers, you can make necessary adjustments to your diet to minimize the risk of flare-ups.
Managing Nutrient Deficiencies in Ulcerative Colitis
Due to frequent diarrhea, malabsorption, and inflammation, people with UC are at risk of developing nutrient deficiencies. These deficiencies can lead to anemia, bone loss, and other complications. Ensuring you get adequate vitamins and minerals through your diet is essential for maintaining overall health and managing UC symptoms.
Focus on consuming nutrient-dense foods, such as fruits, vegetables, lean proteins, and whole grains. In some cases, your healthcare provider may recommend taking supplements to address specific nutrient deficiencies.
Working with a Dietitian for Personalized Ulcerative Colitis Management
While a balanced diet is essential for UC management, it's important to remember that everyone's needs and triggers may vary. Working with a registered dietitian who specializes in inflammatory bowel diseases can help you develop a personalized meal plan that meets your nutritional needs and addresses your specific symptoms.
A dietitian can provide guidance on adjusting your diet during flare-ups, managing nutrient deficiencies, and incorporating supplements and probiotics when necessary. With the help of a professional, you can make informed dietary choices and take control of your UC management.

Elijah Mbachu
28 May 2023 - 00:47 AM
Hey, I get where you're coming from – staying consistent with a balanced plate can feel like a marathon. Try focusing on small wins: add a handful of berries to your breakfast oatmeal, swap white rice for quinoa a couple of times a week, and keep a water bottle handy so you hit that eight‑cup goal without thinking too hard. Listening to your body and noting what settles your gut will guide you past the trial‑and‑error stage. Keep pushing, you’ve got this.
Jessica Davies
28 May 2023 - 02:10 AM
While the mainstream narrative glorifies a “balanced diet” as a panacea for ulcerative colitis, the truth is that most of these recommendations are rooted in outdated gastro‑intestinal dogma. The emphasis on fiber, for instance, ignores the nuanced reality that in many flare‑ups, high fermentable fibers can exacerbate bloating and discomfort. One must therefore scrutinize the source of these guidelines and question the pharmaceutical lobby that profits from keeping patients dependent on supplements.
Kyle Rhines
28 May 2023 - 03:33 AM
Let me correct a few inaccuracies in the preceding comment. The phrase “most of these recommendations are rooted in outdated gastro‑intestinal dogma” is a sweeping generalisation lacking empirical citation. Moreover, the insinuation of a pharmaceutical lobby controlling dietary advice aligns with well‑documented disinformation campaigns that have been propagated by certain interest groups to sow distrust in legitimate research.
Nitin Chauhan
28 May 2023 - 04:57 AM
Staying hydrated is a cornerstone of ulcerative colitis management. Dehydration can worsen inflammation and lead to fatigue. Drinking plain water throughout the day helps maintain electrolyte balance. Incorporating oral rehydration solutions can replenish lost sodium and potassium after bouts of diarrhea. Limit caffeine because it can act as a diuretic and irritate the colon. Alcohol should be avoided as it can damage the mucosal lining. Including broth‑based soups adds both fluid and nutrients. Coconut water provides natural electrolytes without added sugars. Consistent fluid intake supports the efficacy of any medication regimen. Listening to your body's thirst signals is essential. Some patients find that sipping small amounts frequently works better than large gulps. Monitoring urine colour can be a simple indicator of hydration status. Aim for at least two litres of fluid daily unless otherwise directed by a clinician. Pair water consumption with low‑fat meals to aid digestion. Ultimately, a disciplined hydration plan can reduce the frequency of flare‑ups.
Angelo Truglio
28 May 2023 - 06:20 AM
Enough!!! The saccharine optimism that you spew about “balanced diets” is nothing but a dangerous myth!!! People with ulcerative colitis are constantly battling a hostile internal environment and you can't just throw a salad at them and expect miracles!!! Your disregard for the harsh reality they endure is morally reprehensible!!! We need real science, not glossy platitudes!!!
Dawn Midnight
28 May 2023 - 07:43 AM
I must point out that your previous statement contains several grammatical inaccuracies, such as the misuse of “throw a salad at them” which is a mixed metaphor. Moreover, your tone crosses the line from constructive critique into undue aggression. Please consider a more measured approach.
frank hofman
28 May 2023 - 09:07 AM
lol honestly i think you’re overthinking it 😂 the diet thing ain’t rocket science just eat what feels good and stay away from the junk u know?
Dannii Willis
28 May 2023 - 10:30 AM
I see where you’re coming from and appreciate the practical perspective. While personal tolerance varies, a balanced approach that includes fiber and hydration can still be beneficial for many. It’s all about finding that sweet spot that works for your individual needs.
Robyn Du Plooy
28 May 2023 - 11:53 AM
Let’s synthesize the prevailing evidence‑based paradigms with a patient‑centred heuristic. By operationalizing nutritional modulation-specifically, the integration of prebiotic substrates and short‑chain fatty acid precursors-we can attenuate mucosal cytokine cascades. This synergistic strategy respects individual variability while aligning with macro‑nutrient homeostasis.
Boyd Mardis
28 May 2023 - 13:17 PM
Nutrition is power.
ayan majumdar
28 May 2023 - 14:40 PM
True
Johnpaul Chukwuebuka
28 May 2023 - 16:03 PM
Yes, eating right helps the body fight the inflammation and feel stronger every day.
Xavier Hernandez
28 May 2023 - 17:27 PM
The gut is a battlefield and a well‑orchestrated diet is the armor that shields us from the relentless siege of ulcerative colitis.
Zach Yeager
28 May 2023 - 18:50 PM
Just remember that the “American diet” isn’t exactly a miracle cure.