Polypharmacy in Seniors: Risks, Red Flags, and Safer Choices
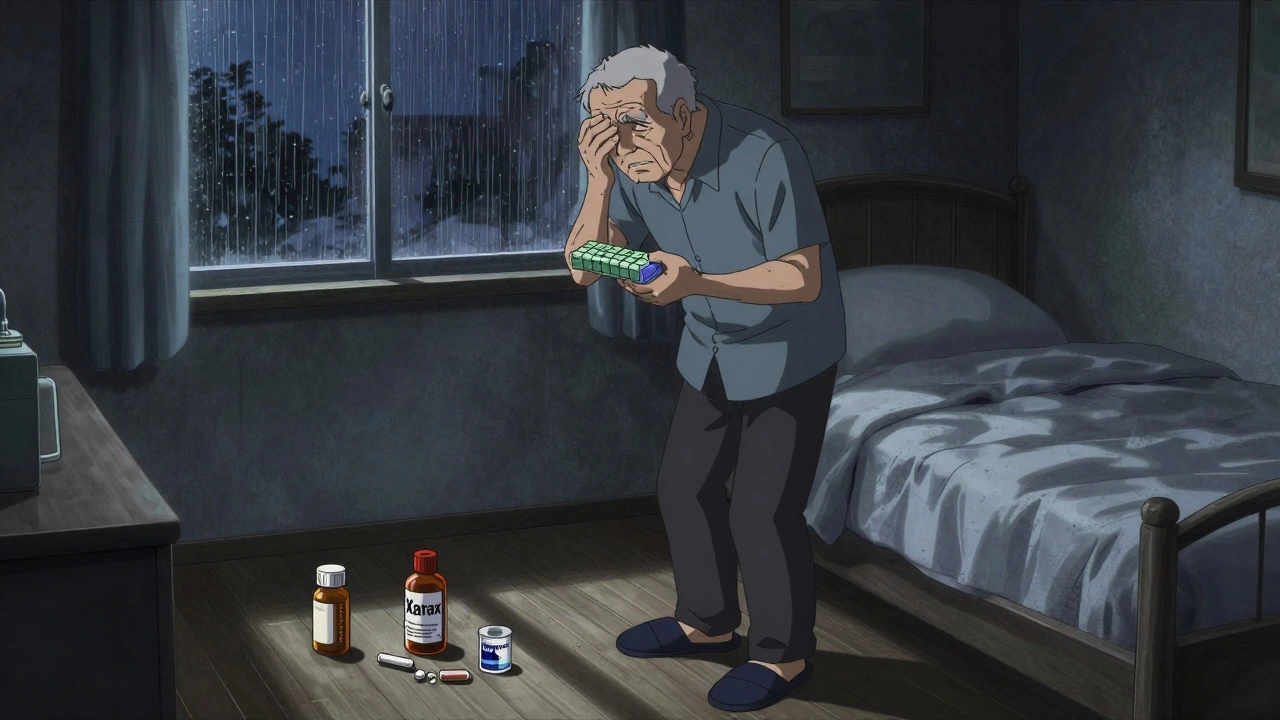
When older adults take polypharmacy in seniors, the use of five or more medications at the same time. Also known as multiple medication use, it’s not always avoidable—but it’s often unnecessary. For many seniors, each pill was prescribed for a different condition by a different doctor, with little coordination between them. The result? A tangled web of drugs that can cause falls, confusion, kidney damage, and even hospital stays.
This isn’t just about quantity—it’s about high-risk medications seniors, drugs that are more likely to cause harm in older adults due to changes in metabolism, kidney function, and brain sensitivity. These include benzodiazepines for sleep, anticholinergics for overactive bladder, and certain painkillers that increase fall risk. The Beers Criteria is the gold standard doctors use to flag these drugs, yet many are still prescribed without review. A 2023 study in JAMA found that over 40% of seniors on five or more drugs were taking at least one high-risk medication with no clear benefit.
Why does this keep happening? Because treating one condition often ignores the others. A blood pressure drug might worsen dizziness. A stomach acid reducer might lower vitamin B12 levels, leading to nerve damage. And when a senior sees three different specialists, none of them are talking to each other—or to the pharmacist. That’s where a medication review, a structured check-up of all current drugs by a pharmacist or doctor to identify duplicates, interactions, and unnecessary prescriptions. Also known as deprescribing, it’s not about stopping everything—it’s about stopping what doesn’t belong.
Many seniors don’t even know they’re on too many drugs. They take what’s in the pill organizer, assuming it’s all necessary. But a simple review can uncover pills that haven’t been needed for years—like an old antidepressant after depression has cleared, or a cholesterol drug that was stopped after a liver issue. The senior drug safety, the practice of choosing medications that minimize harm and maximize quality of life in older adults. Also known as geriatric prescribing, it’s not about age—it’s about physiology.
You don’t need to be a doctor to start asking questions. Bring a full list of every pill, vitamin, and supplement to every appointment. Ask: "Is this still needed?" "Could this be causing my dizziness or confusion?" "Is there a safer alternative?" Small changes—like swapping a sedating sleep aid for better sleep hygiene, or replacing an NSAID with acetaminophen for pain—can make a huge difference. The goal isn’t fewer pills for the sake of it. It’s fewer pills that are actually hurting you.
The posts below give you real, practical tools to take control. You’ll find clear guides on spotting dangerous drugs, understanding the Beers Criteria without the jargon, and how to talk to your doctor about cutting back. You’ll see how common side effects like dizziness or memory lapses might not be "just aging"—they could be medication-related. And you’ll learn what to do when your pharmacy tells you a drug is expired or recalled. This isn’t theory. It’s what works for real people trying to stay safe, strong, and independent as they get older.
Medications That Increase Fall Risk in Older Adults: What You Need to Know
Many older adults fall because of medications they're taking-antidepressants, sleep aids, blood pressure drugs, and more. Learn which drugs raise fall risk and what to do about them.
Read More