IBS – Irritable Bowel Syndrome Resources
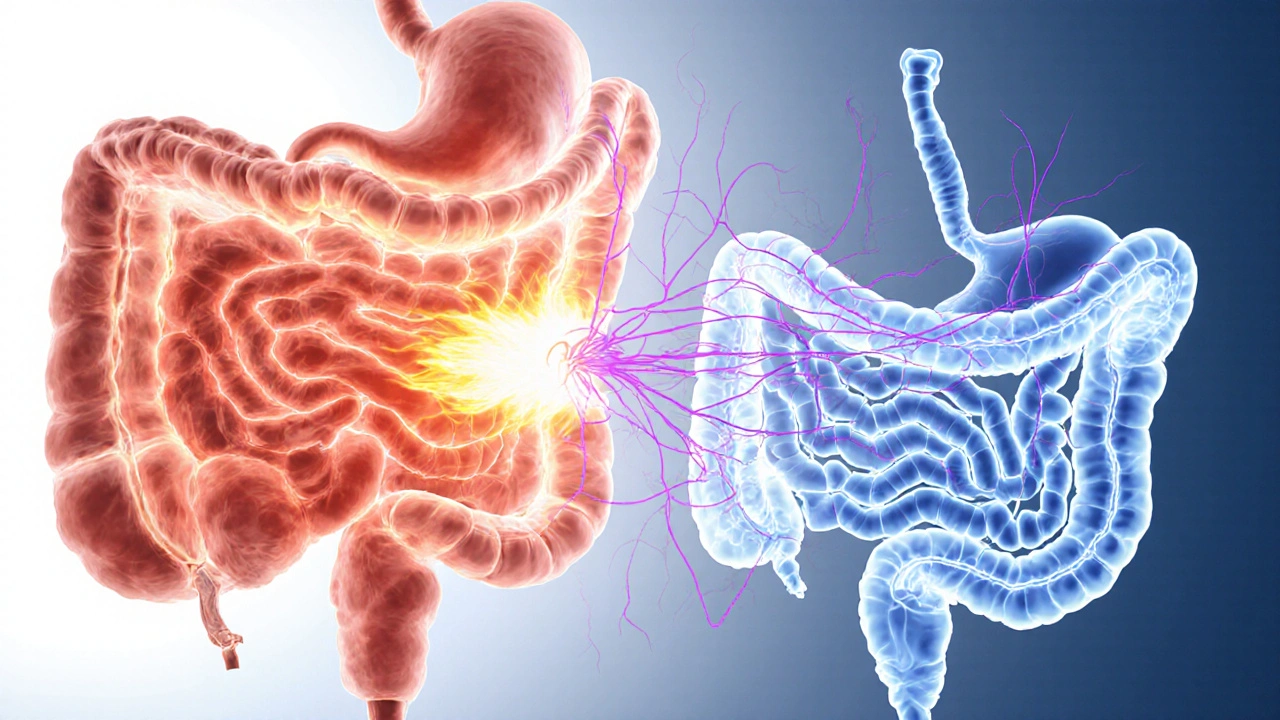
When dealing with IBS, a functional gastrointestinal disorder marked by recurring abdominal pain, bloating, and altered bowel habits. Also known as Irritable Bowel Syndrome, it affects up to 15% of adults worldwide and can disrupt daily life. One of the most effective dietary strategies is the FODMAP diet, a low‑fermentable carbohydrate plan that reduces gas‑producing foods and often relieves symptoms. Alongside diet, many patients turn to probiotics, live microbial supplements that aim to restore a balanced gut flora. Understanding the gut microbiome, the complex community of bacteria, viruses, and fungi living in our intestines is becoming central to modern IBS management. These concepts intertwine: the microbiome influences how we react to FODMAPs, while probiotics can modify microbial composition, potentially easing IBS discomfort.
How these pieces fit together
Clinicians diagnose IBS by ruling out organic disease and looking for patterns described in the Rome IV criteria. The condition reflects a disrupted gut‑brain axis, where stress, hormones, and microbial signals affect motility and sensitivity. A high‑FODMAP meal can increase luminal distension, triggering the brain’s pain pathways—a clear cause‑effect relationship. Meanwhile, a diverse gut microbiome may buffer this response by producing short‑chain fatty acids that soothe the intestinal lining. Research shows that targeted probiotic strains, such as Bifidobacterium infantis, can lower abdominal pain scores, illustrating the triple “diet‑microbiome‑symptom” connection. Lifestyle tweaks like regular exercise, adequate sleep, and mindfulness also modulate these pathways, offering a non‑pharmacologic route to relief.
Beyond diet and microbes, medication options range from antispasmodics to low‑dose antidepressants that calm gut nerves. Each treatment aligns with a specific attribute of IBS: speed of onset, side‑effect profile, and patient preference. Our collection below gathers practical guides on these topics—from FODMAP meal planning and probiotic selection to medication comparisons and stress‑management techniques. Whether you’re just learning what IBS means or seeking the next step in your care plan, you’ll find concise, actionable information ready to help you take control. Understanding IBS is the first step toward a more comfortable life, and the articles ahead will give you the tools you need.
How Acid Indigestion Relates to IBS: Causes, Symptoms & Relief
Explore how acid indigestion and IBS are linked, uncover shared triggers, and learn combined strategies-diet, stress relief, and meds-to ease both conditions.
Read More