Chronic Inflammation: What It Is and What You Can Do
Chronic inflammation is the low-level, long-lasting inflammation that keeps your body in a stressed state. Unlike the redness and pain from a sprain, this one can quietly damage organs over months or years. You don’t always feel dramatic symptoms, but things like persistent fatigue, joint aches, digestive upset, or unexplained weight gain can be signs.
What to look for
Ask yourself: have you had ongoing symptoms for weeks or months that don’t get better? Check for swollen or stiff joints, frequent gut problems, lingering sore throat, or constant tiredness. Your doctor can run simple blood tests like CRP or ESR to measure inflammation. If those are high, they’ll investigate underlying causes—autoimmune disease, chronic infections, or metabolic issues like type 2 diabetes.
How to lower chronic inflammation — practical steps
Change your plate first. Swap sugary drinks and refined carbs for whole foods: fatty fish (salmon, mackerel), leafy greens, berries, nuts, beans, and olive oil. These foods provide omega-3s and antioxidants that calm inflammation. Cut back on processed foods, fried items, and excess sugar—those promote inflammatory signals.
Move more, but keep it realistic. Aim for 150 minutes of moderate activity a week—brisk walking, cycling, or swimming. Exercise lowers inflammatory markers and helps control weight. If joint pain limits you, try low-impact options like water aerobics or chair exercises.
Sleep matters. Poor sleep raises inflammation. Target 7–9 hours per night and keep a regular sleep schedule. Small habits—no screens an hour before bed, a dark cool room, and a wind-down routine—can make a big difference.
Manage stress. Chronic stress keeps your immune system turned on. Try short daily practices that actually fit your life—5 minutes of focused breathing, a quick walk, or a simple body-scan before bed. Even tiny stress breaks add up.
Consider targeted supplements but be cautious. Omega-3 fish oil and curcumin (turmeric extract) show anti-inflammatory effects in many people. Talk to your doctor before starting anything, especially if you take blood thinners or other meds.
Know when medication is needed. Over-the-counter NSAIDs can ease symptoms short-term but aren’t a long-term fix and can cause side effects. For autoimmune or severe cases, doctors may prescribe steroids, DMARDs, or biologic drugs. That decision should be made with a specialist.
Track and review. Keep a simple symptom diary for two weeks—what you eat, activity, sleep, stress, and symptoms. Patterns often emerge and help you and your clinician make targeted changes.
If symptoms persist or tests show high inflammation, see your doctor. Early action reduces long-term risk for heart disease, arthritis progression, and other complications. Small, consistent steps—diet, movement, sleep, and stress control—are the most practical and powerful tools for lowering chronic inflammation.
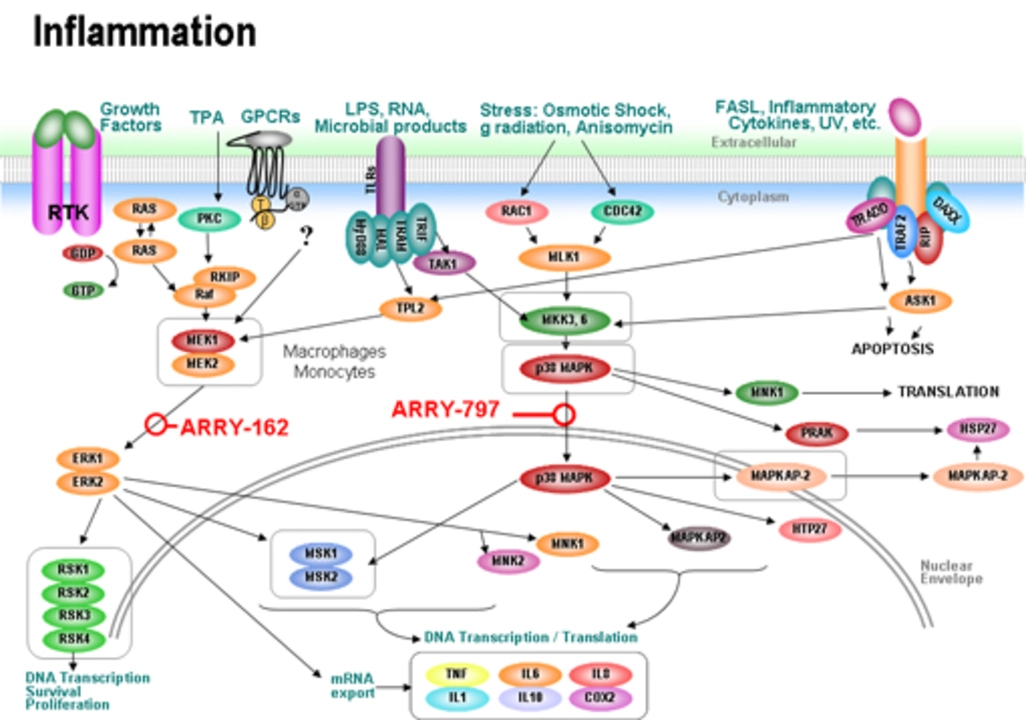
The Connection Between Cancer and Chronic Inflammation
In recent studies, I've discovered a significant connection between cancer and chronic inflammation. It appears that long-term inflammation can lead to DNA damage, fostering an environment for cancer development. Additionally, inflammatory cells can release chemicals that promote tumor growth and suppress our immune system. Therefore, it's crucial for us to manage inflammation through a healthy lifestyle and diet. By doing so, we can reduce our risk of cancer and increase our overall wellbeing.
Read More