Biomarkers: a simple guide to what they are and why they matter
Biomarkers show something measurable about your body—like cholesterol level, a gene variant, or a protein that signals inflammation. They’re not magic answers, but they’re useful clues doctors and researchers use to diagnose problems, pick medicines, and check whether treatment is working.
Think of a biomarker as a signal. A high blood sugar reading is a biomarker for diabetes risk. PSA can be a biomarker for prostate issues. In cancer care, certain gene changes are biomarkers that tell doctors which drugs may or may not work. The clearer the link between biomarker and disease, the more helpful it is.
How biomarkers affect medication and care
Biomarkers can change how a medicine is chosen, dosed, or stopped. For example, genetic tests can predict whether a drug will be effective or cause serious side effects. That helps avoid trial-and-error. Lab tests monitoring liver enzymes or kidney function act as safety biomarkers to catch problems early so dosing can be adjusted.
Some medications require regular biomarker checks. If you're on statins, your doctor may watch liver tests. If you take blood thinners, INR is a biomarker to guide dosing. Newer targeted cancer drugs often require a specific tumor biomarker before treatment starts.
Practical tips for using biomarker info
Don’t panic over a single number. Biomarker values vary by test, lab, and person. Ask your clinician what the result means for you, not just whether it’s "normal." If a test suggests a higher risk, ask about lifestyle or treatment steps you can take now.
Bring previous test results when you visit. Trends matter more than one-off readings. Tell your provider about all meds and supplements—some change biomarker readings or interact with tests. If a drug has monitoring recommendations, follow them. Missing checks can lead to avoidable side effects.
Be cautious with direct-to-consumer tests. They can be helpful but aren’t a replacement for medical advice. If a home test shows concerning results, confirm them with a medical-grade lab and discuss next steps with a clinician who knows your history.
Keep privacy in mind. Genetic and biomarker data can be sensitive. Ask how your results are stored and who can access them before you consent to testing. If you use online services, choose ones with clear data-protection policies.
On this site you'll find articles that mention biomarkers in drug guides, interaction posts, and treatment options. Use those articles to understand why a test matters for a specific medicine or condition, but always pair that with a conversation with your provider.
Want to know if a test fits you? Ask: What will this biomarker tell us? How will it change my treatment? What are the risks of testing? That keeps the focus on useful answers, not on scary numbers.
Examples: If you read an article about clopidogrel or warfarin, look for mentions of CYP2C19 or INR—those are biomarkers that guide dosing. For cancer drugs, the post should say which mutation is required. When in doubt, ask for a simple explanation of what a test result means for your daily life. We update articles with practical monitoring tips—use the search box to find posts that mention biomarkers relevant to your meds. Start by checking your meds' pages today.
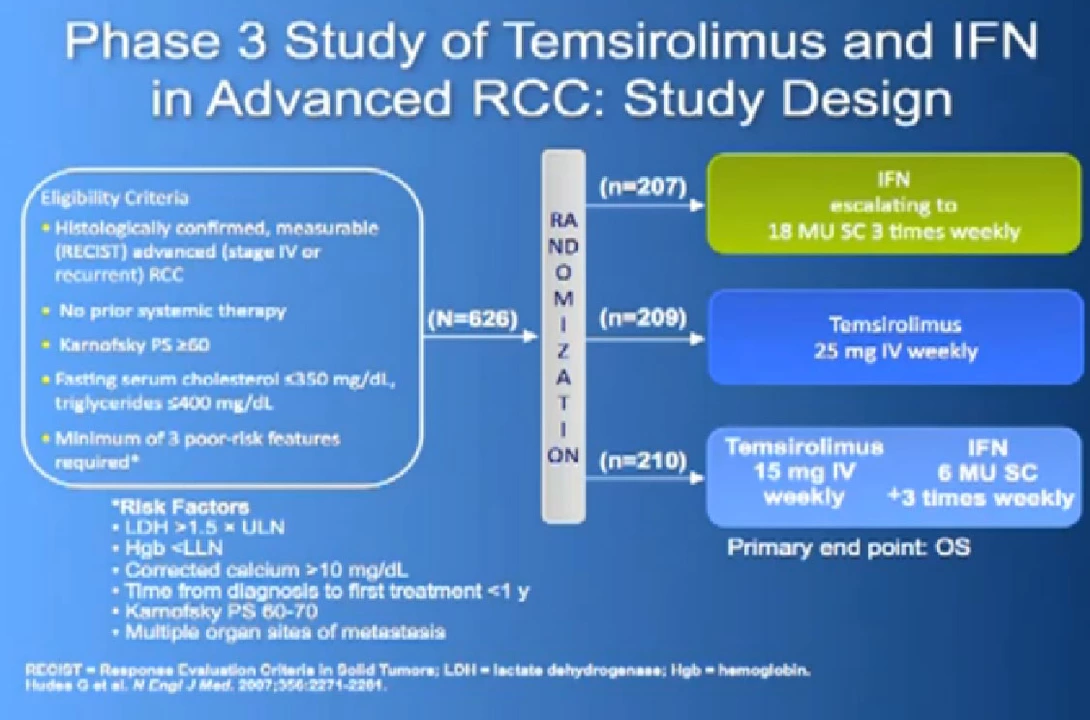
The Role of Biomarkers in Advanced Renal Cell Carcinoma Treatment
As a blogger, I've been researching the role of biomarkers in advanced renal cell carcinoma treatment. Biomarkers have emerged as crucial tools for predicting patient outcomes and personalizing therapy. They help clinicians to determine which patients are more likely to respond to specific treatments, such as immunotherapy or targeted therapy. Additionally, biomarkers can also help monitor treatment effectiveness and detect disease recurrence. Overall, incorporating biomarkers into advanced renal cell carcinoma treatment can significantly improve patient care and outcomes.
Read More