Understanding Renal Cell Carcinoma and Its Stages
Before diving into the role of biomarkers in advanced renal cell carcinoma treatment, it is essential to understand what renal cell carcinoma (RCC) is and its different stages. RCC is the most common type of kidney cancer, and it typically occurs in the lining of the small tubes within the kidneys. The severity of RCC is categorized into four stages, with stage IV being the most advanced and signifying that the cancer has spread to other organs or distant parts of the body.
At this stage, treatment options become more limited and challenging to administer. It is crucial, therefore, to develop new strategies and tools to improve the management and treatment of advanced renal cell carcinoma. One such approach is the use of biomarkers, which can provide valuable information about the cancer's behavior and help guide treatment decisions.
The Importance of Biomarkers in Cancer Treatment
Biomarkers are biological molecules found in blood, tissue, or other body fluids that can indicate the presence of cancer, its progression, or its response to treatment. They are an essential tool in cancer research and clinical practice, as they can help improve the accuracy of diagnosis, predict patient outcomes, and guide treatment decisions. In the context of advanced RCC, biomarkers can play a critical role in identifying patients who may benefit from specific therapies or may need more aggressive treatment strategies.
Several biomarkers have been identified in RCC, including proteins, genes, and other molecules. These biomarkers can be used for various purposes, such as monitoring disease progression, assessing treatment response, and predicting survival outcomes. In this article, we will discuss the role of some key biomarkers in advanced RCC treatment and how they can potentially improve patient care.
Identifying Prognostic Biomarkers in Advanced RCC
Prognostic biomarkers are molecules that can provide information about a patient's overall survival or the likelihood of cancer recurrence. In advanced RCC, several prognostic biomarkers have been identified, including the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) risk model, which incorporates clinical and laboratory factors to predict patient outcomes. Other prognostic biomarkers in RCC include certain gene mutations, such as BAP1 and PBRM1, which have been associated with poorer survival outcomes.
By identifying these prognostic biomarkers, clinicians can better understand a patient's disease course and develop a more personalized treatment plan. This approach is particularly important in advanced RCC, where treatment options are more limited and can have significant side effects.
Using Predictive Biomarkers to Guide Therapy Selection
Predictive biomarkers are molecules that can help determine the likelihood of a patient responding to a specific therapy. In advanced RCC, several predictive biomarkers have been identified, including programmed death-ligand 1 (PD-L1) expression and tumor mutational burden (TMB). These biomarkers can help guide the selection of targeted therapies, such as immune checkpoint inhibitors, which have shown promising results in treating advanced RCC.
By using predictive biomarkers to identify patients who are more likely to respond to certain treatments, clinicians can make more informed decisions about which therapies to administer and potentially improve patient outcomes.
Monitoring Treatment Response and Resistance with Biomarkers
Biomarkers can also be used to monitor a patient's response to treatment and detect the development of resistance to specific therapies. For example, changes in circulating tumor DNA (ctDNA) levels can provide real-time information about tumor dynamics and help clinicians determine if a patient is responding to treatment or if the cancer is progressing.
Additionally, the identification of biomarkers associated with resistance to targeted therapies, such as tyrosine kinase inhibitors, can help guide clinicians in adjusting treatment strategies and potentially overcoming resistance mechanisms.
Exploring the Potential of Liquid Biopsies in Advanced RCC
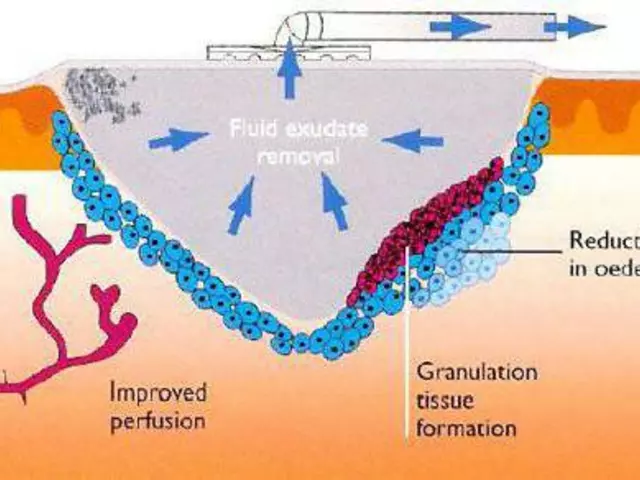
Liquid biopsies are a non-invasive method for collecting and analyzing biological samples, such as blood or urine, to detect cancer biomarkers. In advanced RCC, liquid biopsies can be used to monitor disease progression, assess treatment response, and identify potential resistance mechanisms. This technique offers several advantages over traditional tissue biopsies, including reduced risk of complications, the ability to capture tumor heterogeneity, and the possibility of more frequent sampling to track real-time changes in tumor biology.
As liquid biopsy technology continues to advance, it has the potential to significantly impact the management and treatment of advanced RCC by providing valuable biomarker information in a minimally invasive manner.
Challenges and Limitations of Biomarkers in Advanced RCC
While biomarkers hold great promise in improving the treatment of advanced RCC, there are still several challenges and limitations to their clinical application. Some of these challenges include the identification and validation of new biomarkers, the development of standardized assays and protocols for biomarker assessment, and the need for further research to better understand the complex biology of RCC and its response to treatment.
Despite these challenges, continued research and collaboration between clinicians, researchers, and the pharmaceutical industry will likely lead to the discovery and validation of new biomarkers, ultimately improving the management and treatment of advanced RCC.
Future Directions in Biomarker Research for Advanced RCC
The field of biomarker research in advanced RCC is rapidly evolving, with new discoveries constantly being made. As our understanding of RCC biology and treatment response improves, it is likely that additional biomarkers will be identified, leading to more personalized treatment strategies and better patient outcomes. Some key areas of future research in this field include the identification of novel prognostic and predictive biomarkers, the development of new liquid biopsy techniques, and the exploration of potential biomarkers for emerging therapies, such as adoptive cell therapies and cancer vaccines.
By continuing to advance our knowledge of biomarkers in advanced RCC, we can hope to significantly improve the treatment landscape for patients with this challenging disease.
Conclusion
In conclusion, biomarkers play a crucial role in the management and treatment of advanced renal cell carcinoma. They can help improve the accuracy of diagnosis, predict patient outcomes, guide treatment decisions, and monitor treatment response. Although there are still challenges and limitations to their clinical application, continued research in this area has the potential to significantly impact patient care and ultimately improve outcomes for those living with advanced RCC.


Emma Howard
30 April 2023 - 02:45 AM
Great overview on RCC biomarkers!
dee gillette
4 May 2023 - 17:52 PM
While the article provides a thorough summary, it arguably overstates the current clinical utility of many of these biomarkers; rigorous validation in larger cohorts remains essential before widespread adoption.
Jasin P.
9 May 2023 - 08:59 AM
Oh sure, let’s just throw a few gene panels at every patient and call it a day. As if a handful of mutations can magically solve the deep‑rooted challenges of advanced RCC treatment. This feels more like techno‑optimism than real‑world medicine.
Lily Đàn bà
14 May 2023 - 00:05 AM
Honestly, the enthusiasm feels a bit misplaced – we’re still chasing shadows. Even with all the flashy biomarkers, many patients see little change in outcomes. It’s a dramatic narrative that doesn’t match the gritty reality on the ground.
Joseph O'Sullivan
18 May 2023 - 15:12 PM
Think of biomarkers as the philosophy of medicine – they’re questions we ask the tumor about its own nature. When we listen, we get hints, not answers. It’s an informal dance between data and decision‑making.
Conor McCandless
23 May 2023 - 06:19 AM
When we talk about biomarkers in advanced renal cell carcinoma the conversation quickly moves beyond simple lab values and into the realm of personalized medicine. The IMDC risk model, for instance, is not just a collection of numbers but a sophisticated attempt to stratify patients based on their biology and clinical presentation. In my experience the inclusion of gene mutations such as BAP1 and PBRM1 in prognostic panels adds a layer of depth that traditional imaging simply cannot provide. Moreover the predictive power of PD‑L1 expression and tumor mutational burden has opened doors for checkpoint inhibitor therapies that were once thought out of reach for stage IV disease. One must also consider the logistical challenges of bringing these assays into routine clinical practice; standardization of testing protocols remains a moving target. Liquid biopsies, while promising, still suffer from variability in ctDNA detection thresholds that can lead to false reassurance or unnecessary alarm. Nevertheless the real‑time monitoring capability offered by blood‑based biomarkers could revolutionize how we adapt treatment regimens on the fly. Take for example a patient whose ctDNA levels rise sharply despite radiographic stability; this could signal an emerging resistance mechanism before it becomes clinically apparent. On the therapeutic front the ability to tailor tyrosine kinase inhibitor combinations based on molecular signatures may finally overcome the dreaded resistance patterns that have plagued us for years. It is also worth noting that the economic implications of widespread biomarker testing cannot be ignored; payers are still figuring out cost‑effectiveness models. From a research perspective the ongoing trials exploring novel biomarkers such as circulating microRNAs hold the promise of even finer granularity in patient selection. In short the field is moving at a breakneck pace and the clinician must stay educated or risk being left behind. The collaborative effort between oncologists, pathologists, and bioinformaticians is essential to translate these discoveries into real‑world benefit. Patients, too, should be empowered with knowledge about the tests they undergo, fostering a shared decision‑making environment. Ultimately the goal remains clear: to shift the paradigm from a one‑size‑fits‑all approach to a truly individualized treatment plan that maximizes survival while minimizing toxicity.
kat gee
27 May 2023 - 21:25 PM
Super helpful summary! Keep the momentum going – every bit of info helps us stay hopeful.
Iain Clarke
1 June 2023 - 12:32 PM
Building on the points above, it’s crucial to integrate these biomarkers with existing clinical guidelines to avoid fragmenting care. Consistency across labs and clear reporting standards will make the data actionable for frontline oncologists.
JOJO Yang
6 June 2023 - 03:39 AM
The drama of biomarkers is real – but we cant ignore the basic science, lol.
Faith Leach
10 June 2023 - 18:45 PM
Don’t forget that big pharma might be steering the narrative; they love a good biomarker hype because it fuels new drug pipelines – keep your eyes open.
Adam Martin
15 June 2023 - 09:52 AM
Honestly, the whole biomarker craze feels like a tech‑startup trying to sell a solution before it’s truly proven – yet at the same time, I can’t deny the incremental insights we’ve gained. It’s a paradox: the data promises precision, but the implementation often lags behind, leaving clinicians in a gray zone. We need more real‑world evidence, not just glossy trial results, to convince skeptics. In practice, many of these tests are expensive, and insurance coverage is patchy, which adds another layer of frustration for patients already battling a tough disease. Still, I’m cautiously optimistic – if we can standardize assays and democratize access, biomarkers could become the compass guiding therapy choices rather than an after‑thought.
Ryan Torres
20 June 2023 - 00:59 AM
👍🏼 Absolutely, Adam. The optimism needs to be backed by solid data and affordable testing. 💊💉
shashi Shekhar
24 June 2023 - 16:05 PM
Another endless list of “future possibilities” while patients wait for real cures – classic lazy critique.
Marcia Bailey
29 June 2023 - 07:12 AM
Hey, let’s keep the conversation constructive – every perspective adds value, and supporting each other makes the research community stronger. 😊