Balanced Diet: Real Food Habits You Can Start Today
Think a balanced diet means strict rules and boring food? Think again. A balanced diet is just a simple pattern that keeps your energy steady, helps digestion, and supports whatever meds or supplements you take. Small, clear changes beat big, short-lived diets every time.
What a balanced plate actually looks like
Use this easy visual: half your plate vegetables and fruit, one quarter lean protein, one quarter whole grains or starchy veg, plus a small amount of healthy fat. Practical servings: a fist of veggies (about 1 cup), a palm-sized piece of protein (3–4 oz), a cupped hand of cooked grains (about 1 cup), and a thumb-sized amount of oil, nuts, or cheese.
Examples that hit those targets: grilled chicken with quinoa and roasted broccoli; a chickpea salad with mixed greens and a drizzle of olive oil; oatmeal topped with berries and a spoon of peanut butter. Snacks that fit: an apple with a handful of almonds, or carrot sticks with hummus.
Key rules that actually help
1) Aim for color: different colors mean different nutrients. Add at least two colors at each meal. 2) Favor whole grains over refined ones—brown rice, oats, whole-wheat bread. 3) Choose lean proteins or plant proteins—fish, beans, lentils, eggs, tofu. 4) Include healthy fats—olive oil, avocados, nuts—sparingly. 5) Fiber matters: it keeps you full and helps digestion. Try to get vegetables, fruit, beans, or oats each day.
Hydration is part of balance too. Water before or between meals helps digestion. Limit sugary drinks and replace them with sparkling water, herbal tea, or plain water with lemon.
If you take medicines, be mindful: some drugs interact with certain foods. For example, grapefruit can affect many statins and other meds; vitamin K-rich foods can change how warfarin works. When in doubt, ask your pharmacist or doctor—simple checks can prevent big problems.
Meal timing is flexible. Some people do best with three meals and two small snacks; others prefer fewer meals. What matters is consistent, nourishing choices and avoiding long stretches without food if your energy drops or medications require food.
Shopping and prep tips that save time and stress: keep frozen vegetables and canned beans on hand, cook grains in bulk and portion them, and use a simple week-night rotation of 4–5 go-to meals. Swap white rice for quinoa or bulgur, swap sugary cereal for Greek yogurt with fruit, and swap fried snacks for roasted chickpeas or nuts.
Want a simple habit to start? Add one extra vegetable to every meal this week. Small changes like that stack up fast and make a real difference in how you feel.
Browse our balanced diet articles and meal ideas for more examples, or ask a pharmacist about food–drug interactions if you’re on any prescription meds. Practical, steady steps beat fads—every meal is a chance to get a little healthier.
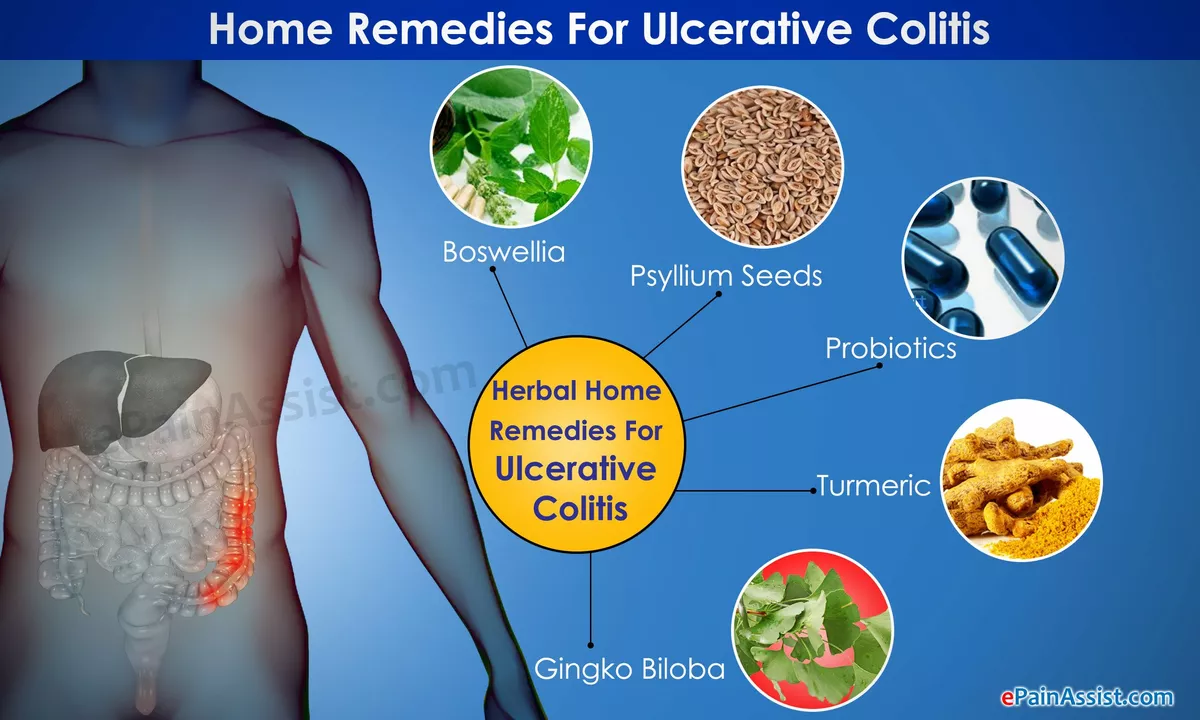
The Importance of a Balanced Diet for Ulcerative Colitis Management
As someone with ulcerative colitis, I cannot stress enough the importance of maintaining a balanced diet for effective management of this condition. A well-rounded diet not only helps reduce inflammation but also aids in maintaining overall gut health. Including a variety of nutrient-rich foods like fruits, vegetables, whole grains, and lean proteins can make a significant difference in symptom management. It's also crucial to pay attention to any personal food triggers and avoid them. Remember, a balanced diet is key to keeping ulcerative colitis under control, so make sure to consult with a healthcare professional or dietitian to find the best plan for you.
Read More